Profiling of Breast Cancer Prevalence and its Diagnosis Using Varied Imaging Techniques in Tanzania
Received: 25-Jul-2024 / Manuscript No. JIDT-24-143201 / Editor assigned: 29-Jul-2024 / PreQC No. JIDT-24-143201 (PQ) / Reviewed: 12-Aug-2024 / QC No. JIDT-24-143201 (QC) / Revised: 19-Aug-2024 / Manuscript No. JIDT-24-143201 (R) / Published Date: 26-Aug-2024 DOI: 10.4172/2332-0877.1000605
Abstract
Breast cancer is not only the most commonly occurring cancer among women, but also the most frequent cause of the cancer-related deaths in women in developing countries. Mortality rate is marginally higher in developing countries than in developed countries with about 60% of the death occurring in developing countries. In Tanzania for example, breast cancer is the second leading cancer in terms of incidence and mortality among women after cervical cancer. Approximately half of all women diagnosed with breast cancer in Tanzania die of the disease. This is due to poor and shortage of medical facilities for cancer screening and diagnosis, poor number of oncologists and pathologists and the diagnosis costs in the country. Due to the mentioned factors, it is approximated that, 80% of breast cancer cases in in Tanzania are diagnosed at advanced stages (III or IV), when treatment is less effective and outcomes are poor. By 2030, new breast cancer cases are approximated to increase by 82% in Tanzania. The diagnosis/screening of breast cancer starts with breast imaging with ultrasound and mammograms. Suspected cases are then subjected into pathology for confirmatory tests. Although breast imaging plays a major role in both breast cancer screening and diagnosis, the service is largely not available in many developing countries. Our study found absence of routinely breast cancer screening in Tanzania, resulting in late-stage detection of many cases. This is mainly due to lack of enough well-trained radiologists to read the images and the costs of the process. This study aimed at exploring the role and challenges of breast imaging in the screening and diagnosis of breast cancer in Tanzania, a developing country. Our results found that, there is a significant number of malignancies under the recommended age of breast cancer screening of fifty years of age. Our study also found a very high Inter variability among radiologists, which suggest the necessity of at least two radiologists reading same case before conclusion of the diagnosis. This study also discovered in our sample size that 66% patients did not have their samples taken for confirmation by the pathologists. This might be due to the costs of the process or loss of follow ups as many patients came far from diagnosis centre. Due to the challenges observed in breast imaging, this study recommends the use of Computer Aided Diagnosis (CAD) with Artificial Intelligence to assist the few numbers of radiologists available.
Keywords: Cancer; Diagnosis; Low-and Middle-Income Countries (LMICs); Pathology
Introduction
Breast cancer is currently the most common cancer globally, affecting mostly women compared to men. It forms in the cells of the breasts and arises either in the lining cells (epithelium) of the ducts or lobules in the glandular tissue of the breast [1,2]. According to WHO, 85% of breast cancer occurs in the lining cells of the ducts whereas 15% occurs in the lobules in the glandular tissue of the breast [3-5].
There are many known risk factors leading to breast cancer, but the causes are not fully understood. The strongest risk factors for breast cancer are being a female gender and to some extent getting older [3]. But studies have shown that the number of young people diagnosed with breast cancer is increasing. Also, black women are reported to be at higher risk of dying from breast cancer compared to women from other ethnic groups.
The early diagnosis of breast cancer is associated with adequate prognosis. This early diagnosis is made possible by the standard way of screening which involves the use of mammogram or ultrasound imaging to detect an anatomical derangement which will be confirmed by a pathologist.
Recent report by Globocan shows that 18.1 million new cases were recorded in 2018 and deaths of 9.6 million people on the same year. The report also tells us that 70% of that death toll occurred in low-and middle-income countries [6]. Also, only 26% of Low-and Middle-Income Countries (LMICs) reported having pathology services available in the public sector compared to 90% of high-income countries [7].
According to WHO, breast cancer is the most frequent cancer among women, impacting 2.1 million women each year and causes the greatest number of cancer-related deaths among women [8]. Breast cancer is the second most common cancer and the second leading cause of cancer mortality among women in Tanzania [9,10]. Approximately half of all women diagnosed with breast cancer in Tanzania die of the disease and approximately 80% of women diagnosed with breast cancer in Tanzania happen at advanced stages (III or IV), when treatment is less effective and outcomes are poor [9-11]. It is predicted that by 2030, new breast cancer cases will increase by 82% in the country [9,10]. It is worth noting that, Tanzania has a very few well trained radiologists and pathologists. This has resulted in a lack of systematic breast cancer screening programs. Efficient breast cancer screening systems are largely unavailable in many developing countries, leading to delayed diagnosis which results and by extension high mortality rate.
The burden of breast cancer in the LMICs is escalated by different factors including ignorance of the susceptible, limited technology, shortages of cancer healthcare related personnel and the associated costs of the current ways for cancer diagnosis [12-15]. The listed factors account for the big number of deaths caused by breast cancer because of the late of detection of the disease. To alleviate the problem, the factors contributing to the burden need to be handled simultaneously. Also, systematic breast cancer screening programs can largely lower the breast cancer morbidity and mortality.
This study aims at exploring the prevalence of breast cancer in Tanzania, the current situation of screening and diagnosis process of breast cancer, the role of breast imaging and proposes potential ways to address the challenges facing the process of screening and diagnosis of breast cancer in the country.
Materials And Methods
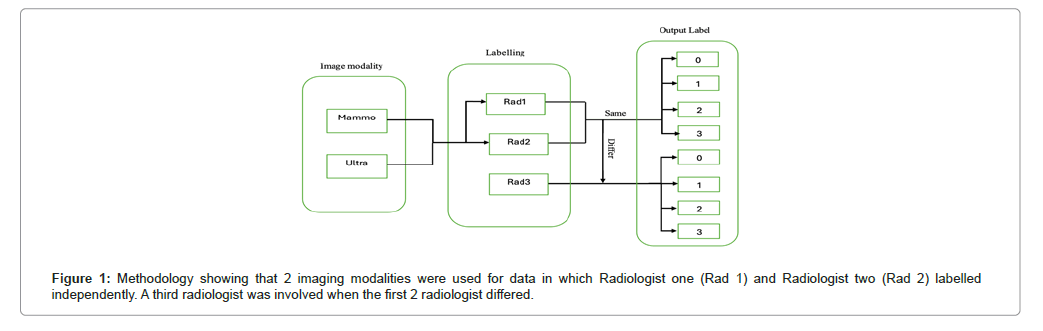
Breast imaging modalities, mammography and ultrasound are the primary imaging modalities for the detection of breast cancer. Mammography may detect cancer one and a half to four years before a cancer becomes clinically evident. We explored the role of the two methods as described in section “materials”. The performance of the two methods was also compared as shown in Table 1. The role of human readers was compared in terms of variations among themselves when reading ultrasound images in Table 2 and when reading mammograms in Table 3. The imaging data used in this analysis was labelled by radiologists with a reference to a ground truth of pathology results as described in Figure 1.
| Both ultrasound and mammogram | Mammogram only | Ultrasound only | Total | |
|---|---|---|---|---|
| Malignant cases | 53 | 100 | 1 | 154 (15.602%) |
| Benign cases | 67 | 86 | 5 | 158 (16.008%) |
| Normal | 11 | 12 | 0 | 23 (2.330%) |
| No histology results | 158 | 450 | 44 | 652 (66.058%) |
| Total | 289 | 648 | 50 | 987 (100%) |
Table 1: The confirmation of the malignant, benign and normal cases was based on the pathology results.
| Pathology results | ||||||
|---|---|---|---|---|---|---|
| Normal (54) | Benign (375) | Malignant (274) | ||||
| Rad. agreement | True labeling | False labeling | True labeling | False labeling | True labeling | False labeling |
| 3 out of 3 | 20/29 | Sep-29 | 99/218 | 119/218 | 58/164 | 106/164 |
| 2 out of 3 | 20/24 | Apr-24 | 79/149 | 70/149 | 16/101 | 85/101 |
| 1 out of 3 | 0/1 | Jan-01 | Aug-03 | Aug-05 | Sep-01 | Sep-08 |
Table 2: Summary of the results indicating the true and false labeling of the ultrasound images compared to the pathologist results.
| Pathology results | ||||||
|---|---|---|---|---|---|---|
| Normal (37) | Benign (252) | Malignant (205) | ||||
| Rad agreement | True labeling | False labeling | True labeling | False labeling | True labeling | False labeling |
| 3 out of 3 | Oct-04 | Oct-06 | 30/70 | 40/70 | 74/97 | 23/97 |
| 2 out of 3 | Sep-19 | Oct-19 | 36/109 | 73/109 | Apr-66 | 62/66 |
| 1 out of 3 | Aug-02 | Aug-06 | 25/73 | 48/73 | Mar-42 | 39/42 |
Table 3: Summary of the results indicating the true and false labeling of the mammogram images compared to the pathologist results.
The data sets consist of images that were collected by using two different imaging technologies which are ultrasound and mammogram. The ultrasound images were obtained using a GE Voluson Pro 8 while the mammography was obtained using a Genoray DMX600. Initially, a total of 1014 patients data was extracted, which included duplicates. After removal of duplicates, 987 patients ranging from 22 to 90 years of ages were involved in the study. From the involved patients, a total of 3842 mammogram and 2021 ultrasound images were obtained. The study included all symptomatic women who came to the radiology department at Muhimbili Mloganzila National Hospital, for breast cancer diagnostic imaging. However, those whose retrieval of images was not successful were excluded.
The labeling process for the obtained dataset was conducted by three radiologists. Two radiologists labeled the images independently, a third radiologist was involved only when the labelling of the first two radiologists differed. The images were labeled into either normal, benign, or malignant. Different labels were used for indicating the status of the patients: Number “0” indicates normal, “1” for benign, “2” for malignant and “3” for inconclusive. Most of the inconclusive cases were due to the quality of images which affected the reading by radiologists. The images were stored in Picture Archiving and Communication Systems (PACS) server and they were extracted by using clear canvas Digital Imaging and Communications in Medicine (DICOM) viewer. For this case, clear canvas facilitates management of the medical images whereas DICOM viewer communicates with PACS servers and viewing DICOM studies [16]. The methodology can be described as in Figure 1 below.
Study design
This was a retrospective study applying quantitative designs. Several patients attending breast cancer clinic at Muhimbili Mloganzila National Hospital from October, 2018 to February, 2022 were identified and included in the study. This study explored the diagnosis process and qualities of the current diagnosis modalities available at the hospital, which represent majority part of the country, as it is in many developing countries. The study was approved by the Institutional Ethical Review Board of Muhimbili University of Health and Allied Sciences (MUHAS). All the methods used in this study were performed in accordance with the guidelines and regulations of MUHAS.
Study settings
This was a retrospective study that was conducted at Muhimbili Mloganzila National Hospital. Analysis of the data was conducted at the Emerging Technologies for Health Research and Development Laboratory (ETH), which is under the Muhimbili University of Health and Allied Sciences (MUHAS), unit of biomedical engineering. The lab is equipped with necessary computing facilities, including Graphics Processing Units (GPUs). This project was funded by the International Development Research Centre (IDRC) through Villgro Africa under the Artificial Intelligence for Development (AI4D) initiative, Google Ireland limited and Swedish International Development Cooperation Agency (SIDA) through MUHAS small grant research program.
Results
Data analysis was conducted to assess the prevalence of breast cancer in Tanzania by looking into the burden of the disease geographically, the role of breast imaging in diagnosis of the diseases with reference to pathology results as a ground truth. The implementation was done by using python programming language.
Prevalence analysis
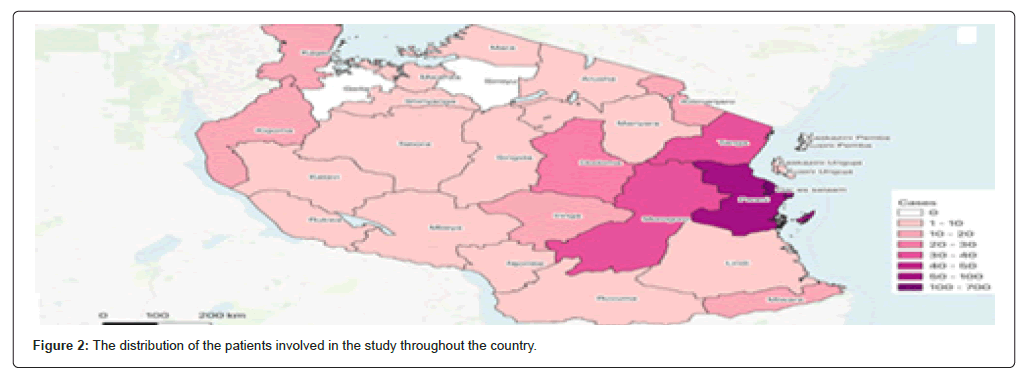
The analysis performed in this study was focused on the representative sample collected at Mloganzila hospital. The findings in this study may vary from the results obtained using data from other regions of the country. But it is worth noting that Mloganzila Hospital is one of the few government hospitals in the country with breast cancer diagnosis clinic using mammogram. Hence, these results may be a good indicator of the prevalence of breast cancer in the country. Figure 2 showing the distribution of the patients involved in the study throughout the country.
Table 1 shows that 15.602% of all the patients in this study were malignant based on who did both imaging (53 patients), mammogram only (100 patients) and ultrasound alone (1 patient). Studies shows that doing both imaging is more accurate in detecting breast cancer than doing one. In our case, we found that only 29% patients used both mammogram and ultrasound, with majority (66%) did only mammogram. Only 5% did ultrasound. Although mammogram is better at detecting abnormalities deeper within the breast tissue, which can tell why it was frequently used, ultrasound might be a potential alternative especially in resource limited countries like Tanzania. There is less than ten mammogram machine in government hospitals compared to ultrasounds which available up to district level hospitals. The high number of patients who did not conduct pathology process (66%), might be due to the high cost associated with the process.
Note that patients who had status indicating right breast: Benign and left breast: Malignant or the other way around was counted in the malignant cases in this analysis. The patients without histology results did not have their samples taken for pathological test. Most of these cases were normal on the image-based screening, hence not subjected to pathology examination. But it is also possible that some patients had different status as some of the image based suspected cases didn’t not proceed into pathology examination most likely due to the associated costs of the procedure or didn’t not go back to the hospital due to the travel distance from their initial locations. The small number of patients with normal status in the tables throughout this paper indicates image based suspected cases who were sent to the pathologists and confirmed to be normal.
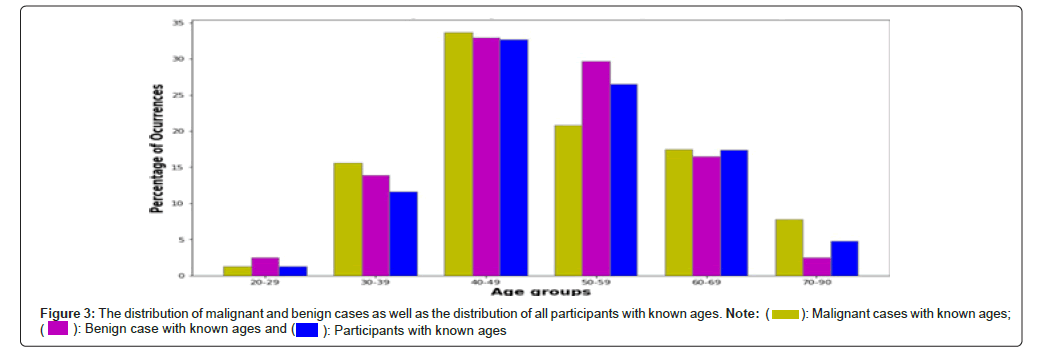
The distribution of the malignant cases is normally distributed across the age groups. The group ranging between 40 to 49 years of age is mostly affected because the highest number of malignant cases fall in this group. Most of the recommendations for breast cancer screening suggest starting at the age of 50. Table 4 shows a significant number of women who are malignant under that age of screening recommendation. Figure 3 shows distribution based on the percentage of benign and malignant in their respective age groups. The graph shows that malignant cases are found almost in all age groups with different intensities.
| Age groups | ||||||||
|---|---|---|---|---|---|---|---|---|
| 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | 70-90 | Unspecified | Total | |
| Malignant cases | 2 (1.3%) | 24 (15.6%) | 52 (33.7%) | 32 (20.8%) | 27 (17.5%) | 12 (7.8%) | 5 (3.2%) | 154 (100%) |
| Benign cases | 4 (2.5%) | 22 (13.9%) | 52 (32.9%) | 47 (29.7%) | 26 (16.5%) | 4 (2.5%) | 3 (1.9%) | 158 (100%) |
| All participants | 13 (1.3%) | 115 (11.6%) | 323 (32.7%) | 262 (26.5%) | 172 (17.4%) | 48 (4.8%) | 54 (5.5%) | 987 (100%) |
Table 4: Distribution of malignant and benign cases based on their ages. The numbers in the third row for all participants also include the participants who did not have histology results.
Current situation of breast cancer screening and diagnosis program
Breast cancer screening involves the organized checking of women’s breasts for cancer before there are signs or symptoms of the disease [17]. According to WHO, the organized and effective screening program is the one in which the participation rate (number of invitees screened) of the target population is over 70% [18]. Even though breast cancer screening cannot prevent the occurrence of breast cancer it can help detecting it early if there are any symptoms of breast cancer and when it is easier to be treated. In Tanzania, different studies about breast- cancer have been performed but currently, there is no systematically organized screening program that performs breast cancer screening for the whole country except some studies [17] (the study carried at Ocean Road Cancer Institute is the National Cancer Center), the one carried in this study and other related studies. They highlight the status of breast cancer in certain localized places and sometimes are not fully focused on screening.
Based on the incidence of breast cancer in Tanzania the records indicate that the problem of breast cancer is steadily growing as breast- cancer is the second most common cancer and the second most common cause of cancer death among women in Tanzanian [19,20]. Tanzania is predicted to have an 82% increase in breast cancer from 2017 to 2030 [15]. This paper shows that mammogram was significantly used for diagnosis of breast cancer in Tanzania. There are very few mammogram machines in Tanzania compared to ultrasound. In addition, ultrasound has no radiation and more user friendly than Mammo, hence can be a perfect tool for mass screening.
Inter variability between the radiologists
Although breast imaging can play a major role in early detection of breast cancer for early intervention, accurate reading of the obtained images is of high significance. Many studies have reported a very high inter variability among radiologists in reading mammograms for detection of breast cancer [21,22]. Tables 2 and 3 present results comparing the labeling for breast cancer that were done by three radiologists for ultrasound and mammogram images respectively. The pathology results were used as the gold standard (ground truth). Only patients who had results from the pathologists indicating the tumor status had their results compared to the radiologist labels. Any patient missing any of the information was excluded from this analysis.
We compared the analysis results of the images in which all the three radiologists labeled correctly and the vice versa against the pathology results. Also, we checked when only two radiologists out of three labeled correctly and vice-versa against pathology results. We also present the situation where all the three radiologists differed from each other in their labels compared to the pathology results.
Looking at Tables 2 and 3 the three status (normal, benign, malignant) each case shows true as well as false labeling by the radiologists. In each row both true and false labels have a common denominator. The common denominator under each case corresponds to the radiologist’s agreement is the number of pathology results in that case. In each case the numerators are the predictions done by radiologist.
Discussion
The burden of breast cancer among women in lower-income countries is contributed by late/missed diagnosis of the disease. The results show that 15% among those who were tested were pathologically confirmed to be malignant. This is a significant percentage of malignancies, and it cannot be overlooked. It is possible that more cases were malignant because 66% patients did not have their samples taken for confirmation by the pathologists.
The WHO recommends mammography screening based on age group and resource setting [23,24]. It recommends organized and population-based mammography screening programs for women aged 50 to 69 years. Despite the recommended age for breast cancer screening, in this study about 50% of malignant cases occurred among women below the WHO recommended age. The results show that 33.7% of the malignant cases are from women with age 40 to 49.
The high prevalence of breast cancer in low-income countries is most likely contributed to different factors. It is possible that poor technological advancement causes many people to be diagnosed late or missed the opportunity. This can be supported by the absence of screening programs in many developing countries. For example, in Tanzania, the screening program is conducted only once a year, in October during breast cancer awareness month with the support of the Medical Women Association of Tanzania (MEWATA).
The analysis has shown that patients involved in the study mostly come Dar es Salaam region and the nearby regions. This situation can be justified by the fact that Mloganzila Hospital was the only government hospital in the country with a breast cancer diagnosis clinic using mammograms. That is the possible reason that drives patients to travel and access the service. It is also possible that the high concentration of patients in Dar es Salaam might be influenced by economic status. The distribution map has indicated that few patients came from regions from the peripheral. These patients traveled long distances to access mammogram diagnosis services.
Conclusion
There are only a few, who can afford it but there are many out there who need similar services. This suggests that the diagnosis needs to be performed in a different part of the country. In addition, although there are already a few numbers of radiologists, further training to use affordable and available imaging methods like ultrasound might reduce the current burden of breast cancer in the country.
Also, there is a limited number of radiologists. It is possible the regions which do not have any data in this study do not have radiologists to interpret the images. This fact does not indicate that these regions do not have breast cancer cases. The results suggest that there is a need for screening programs available in many regions that start at an early age. According to the data analysis presented in this paper, women below 50 years of age are also at high risk of getting breast cancer. The results suggest that there is a need of recommending a new lower age threshold for beginning breast cancer screening to reduce the burden of breast cancer that is likely to happen in old age.
References
- Hinck L, Nathke I (2014) Changes in cell and tissue organization in cancer of the breast and colon. Curr Opin Cell Biol 26:87-95.
[Crossref] [Google Scholar] [PubMed]
- Feng Y, Spezia M, Huang S, Yuan C, Zeng Z, et al. (2018) Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics and molecular pathogenesis. Genes Dis 5:77-106.
[Crossref] [Google Scholar] [PubMed]
- World Healt Organisation (2023) Breast Cancer.
- Pfizer Inc (2024) Breast Cancer.
- Agarwal R (2023) Breast cancer awareness: Breast cancer facts, causes and risk factors.
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394-424.
[Crossref] [Google Scholar] [PubMed]
- Mikhail Lette MN, Paez D, Shulman LN, Guckenberger M, Douillard JY, et al. (2022) Toward improved outcomes for patients with lung cancer globally: The essential role of radiology and nuclear medicine. JCO Glob Oncol 8:e2100100.
[Crossref] [Google Scholar] [PubMed]
- Giordano SB, Gradishar W (2017) Breast cancer: Updates and advances in 2016. Curr Opin Obstet Gyneco 29:12-17.
[Crossref] [Google Scholar] [PubMed]
- Breast Cancer Initiative (2017) Tanzania breast health care assessment 2017: An assessment of breast cancer early detection, diagnosis and treatment in Tanzania.
- Ginsburg O, Yip CH, Brooks A, Cabanes A, Caleffi M, et al. (2020) Breast cancer early detection: A phased approach to implementation. Cancer 126:2379-2393.
[Crossref] [Google Scholar] [PubMed]
- Sakafu LL, Philipo GS, Malichewe CV, Fundikira LS, Lwakatare FA, et al. (2022) Delayed diagnostic evaluation of symptomatic breast cancer in sub-Saharan Africa: A qualitative study of Tanzanian women. Plos one 17:e0275639.
[Crossref] [Google Scholar] [PubMed]
- Mlange R, Matovelo D, Rambau P, Kidenya B (2015) Patient and disease characteristics associated with late tumour stage at presentation of cervical cancer in Northwestern Tanzania. BMC women's health 16:1-6.
[Crossref] [Google Scholar] [PubMed]
- Ngoma T, Mandeli J, Holland JF (2015) Downstaging cancer in rural Africa. Int J Cancer 136:2875-2879.
[Crossref] [Google Scholar] [PubMed]
- Makene FS, Ngilangwa R, Santos C, Cross C, Ngoma T, et al. (2022) Patients’ pathways to cancer care in Tanzania: Documenting and addressing social inequalities in reaching a cancer diagnosis. BMC Health Serv Res 22:189.
[Crossref] [Google Scholar] [PubMed]
- Sood R, Masalu N, Connolly RM, Chao CA, Faustine L, et al. (2021) Invasive breast cancer treatment in Tanzania: Landscape assessment to prepare for implementation of standardized treatment guidelines. BMC cancer 21:1.
[Crossref] [Google Scholar] [PubMed]
- (2023) Clearcanvas DICOM viwer.
- Cherlin DS, Mwaiselage J, Msami K, Heisler Z, Young H, et al. (2022) Breast cancer screening in low-income countries: A new program for downstaging breast cancer in Tanzania. BioMed Res Int. 2022:9795534.
[Crossref] [Google Scholar] [PubMed]
- Salaam DE (2018) The ministry of health, community development, gender, elderly and children. Tanzania.
- Chao CA, Huang L, Visvanathan K, Mwakatobe K, Masalu N, et al. (2020) Understanding women’s perspectives on breast cancer is essential for cancer control: knowledge, risk awareness and care-seeking in Mwanza, Tanzania. BMC Public Health 20:1.
[Crossref] [Google Scholar] [PubMed]
- The Foundation for Cancer Care in Tanzania (2024) Breast Cancer Screening Added to KCMC’s Screening and Earlier Diagnostic Efforts.
- Beam CA, Layde PM, Sullivan DC (1996) Variability in the interpretation of screening mammograms by US radiologists: Findings from a national sample. Arch Intern Med 156:209-213.
[Crossref] [Google Scholar] [PubMed]
- Redondo A, Comas M, Macia F, Ferrer F, Murta-Nascimento C, et al. (2012) Inter-and intraradiologist variability in the BI-RADS assessment and breast density categories for screening mammograms. The Br J Radiol 85:1465-70.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization (2014) WHO Position Paper on Mammography Screening. WHO Press, Switzerland:78.
- Astbury-Ward E (2021) Breast Imaging in Tanzania. UCSF Global Cancer Program, Aunt Minnie Europe.
Citation: Mzurikwao D, Sakafu L, Mayala S, Mzurikwao Z, Nyatega C, et al. (2024) Profiling of Breast Cancer Prevalence and its Diagnosis Using Varied Imaging Techniques in Tanzania. J Infect Dis Ther 12:605. DOI: 10.4172/2332-0877.1000605
Copyright: © 2024 Mzurikwao D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1643
- [From(publication date): 0-2024 - Nov 18, 2025]
- Breakdown by view type
- HTML page views: 1334
- PDF downloads: 309