Case Report Open Access
Primary Intestinal Lymphangieactasia in a Child
Sumathi Bavanandam*, Nirmala Dheivamani and Bhaskar Raju
Department of Pediatric Gastroenterology, Institute of Child Health & Hospital for children, Chennai, India
- Corresponding Author:
- Sumathi Bavanandam
Senior Assistant Professor of Pediatric Gastroenterology
Department of Pediatric Gastroenterology
Institute of Child Health & Hospital for Children, Chennai, India
Tel: 09841371490
E-mail: mailto:drbsumathi@rediffmail.com
Received date: March 11, 2016; Accepted date: June 05, 2016; Published date: June 15, 2016
Citation: Bavanandam S, Dheivamani N, Raju B (2016) Primary Intestinal Lymphangieactasia in a Child. J Gastrointest Dig Syst 6:446. doi:10.4172/2161-069X.1000446
Copyright: © 2016 Bavanandam S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Primary intestinal lymphangiectasia is one of the causes of protein losing enteropathy in children. Three years old female child presented with anasarca, failure to thrive, anemia due to primary intestinal lymphangieactasia. Diagnosis was made by endoscopic finding with histopathology of small intestinal mucosa. She responded to diet therapy with medium chain triglycerides along with fat soluble vitamin supplementation. She is in clinical remission without loose stools, fluid retention with catch up growth on follow up period of three years till now.
Keywords
Primary intestinal lymphangiectasia; Protein losing enteropathy; Chronic diarrhea; Children; Small intestinal biopsy
Case Report
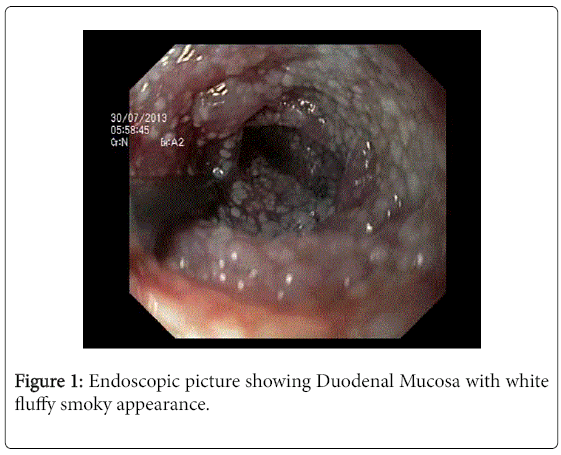
Three years old female child, third born of non-consanguineous parents presented with recurrent loose watery stools without blood, 6-8 episodes per day with pedal edema and puffiness of face since infancy. There was no history of cough, wheeze, rash or vomiting. Clinical examination revealed mild pallor, pedal edema, facial puffiness with weight and height less than 3SD as per WHO growth chart. Abdomen was distended with free fluid without organomegaly. Differential diagnosis of chronic diarrhea with hypoproteinemia in young children can be either primary or secondary. Some of the secondary causes include cow’s milk protein allergy, intestinal tuberculosis, Strongyloidiasis, Crohn’s disease, eosinphilic enteritis and hence investigations were done accordingly. Investigations showed Hb 10 gm/dl, TC 12,000 cells/cu mm. differential count polymorphs 70%, lymphocytes 30%, platelet count 4 lakhs and peripheral smear showed moderate hypochromic anemia. Blood sugar, renal function tests were normal. Motion for ova, cyst and occult blood were negative on three different occasions. Serum total protein was 4.5 gm/dl with albumin 2 gm/dl. Ascitic fluid protein was 134 mg/dl with elevated triglycerides. Chest X-ray was normal. Mantoux and retroviral tests were negative. USG abdomen showed thickened and edematous bowel with ascites. Upper GI endoscopy done using Olympus Video scope, under conscious sedation showed white fluffy flakes of duodenal mucosa due to oozing of lymph (Figure 1) and duodenal biopsy was done. Histopathology of duodenum showed prominent dilatation of lymphatic vessels within lamina propria, blunting of villi, and mild increase in plasma cells, scattered neutrophils and eosinophils consistent with intestinal lymphangiectasia. Child is on nutritional rehabilitation along with low fat diet and medium chain triglycerides, regular fat soluble vitamin supplementation. She is on regular follow up for three years and she is asymptomatic without loose stools, fluid retention with weight of sixteen kg at six years (3rd centile as per CDC growth chart).
Discussion
Primary intestinal lymphangiectasia (PIL) is a rare disorder often diagnosed in children before three years of age and rarely in adolescents. It is also called as Waldmann disease who first identified this clinical condition as “idiopathic hypercatabolic hypoproteinemia” [1]. It is characterized by dilated intestinal lacteals resulting in lymph leakage into the small bowel lumen presenting as protein-losing enteropathy with lymphopenia, hypoalbuminemia and hypogammaglobulinemia. Clinically children present with bilateral pedal often symmetrical edema with serosal involvement or chylous ascites. Symptoms include easy fatiguability, abdominal pain, weight loss, failure to gain weight, diarrhea or fat-soluble vitamin deficiencies [2]. Some of the secondary causes of protein-losing enteropathies associated with intestinal lymphangiectasia are intestinal tuberculosis, Crohn’s disease, intestinal lymphoma, lymphenteric fistula, Whipple's disease, radiation and/or chemotherapy with retroperitoneal fibrosis, human immunodeficiency virus-related enteropathy. Cow’s milk protein allergy is another common cause in infants with chronic diarrhea with hypoproteinemia. Failure of response after observation period to elimination of animal milk products in infants may require prompt referral to pediatric gastrointestinal clinic. Diagnosis of PIL is made by endoscopic appearance showing white opacities of small bowel mucosa confirmed by histological evidence of dilated lacteals of intestinal biopsy specimens. Axial abdominal CT images with oral and intravenous contrast if done, typically shows diffuse, nodular, small bowel wall-thickening and edema, due to dilated lymphatics within the villi, some degree of small bowel dilation and in few cases, classical "halo sign" can be appreciated [3]. However CT abdomen was not done in our case as the diagnosis was made on histology. Management consists of low-fat diet and supplementation with medium chain triglycerides to reduce ensuing intestinal lymph loss as medium chain triglycerides do not require bile salt activated lipase for absorption [4]. In those who do not respond to conservative line of management like dietary modification with medium chain triglycerides supplementation, enteral nutrition with elemental, semi elemental and polymeric diets may be required and even total parenteral nutrition in severe cases. Apart from diet modification other modalities of treatment include use of antiplasmin, octreotide or corticosteroids. Octreotide at 150-200 μg, twice a day or the slow-release formulation might lead to clinical, biochemical and histological improvement The exact mechanism of action of the somatostatin analog on the gastrointestinal tract remains unclear but by virtue of causing shortlasting splanchnic vasoconstriction and inhibiting absorption of triglycerides may be of help in this condition [5].
This case is being reported to highlight the need for early referral of children presenting with protein losing enteropathy to a specialised gastroenterology clinic for further evaluation.
References
- Waldmann TA, Steinfeld JL, Dutcher TF, Davidson JD, Gordon RS (1961) The role of the gastrointestinal system in "idiopathic hypoproteinemia". Gastroenterology41: 197-207.
- Vardy PA, Lebenthal E, Shwachmann H (1975) Intestinal lymphangiectasia: a reappraisal. Pediatrics55: 842-850.
- Mazzie JP, Maslin PI, Moy L, Price AP, Katz DS (2003) Congenital intestinal lymphangiectasia: CT demonstration in a young child. Clin Imaging 27: 330-332.
- Jeffries GH, Champan A, Sleisenger MH (1964) Low fat diet in intestinal lymphangiectasia: its effect on albumin metabolism. N Engl J Med 270: 761-766.
- Vignes S,JérômeBellanger J (2008) Primary intestinal lymphangiectasia (Waldmann's disease) :Orphanet J Rare Dis 3: 5.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11727
- [From(publication date):
June-2016 - Apr 11, 2025] - Breakdown by view type
- HTML page views : 10842
- PDF downloads : 885