Prevalence of Tobacco Product Consumption and Exposure among Healthcare Students in King Saud University in Riyadh, Saudi Arabia
Received: 13-Nov-2017 / Accepted Date: 16-Nov-2017 / Published Date: 20-Nov-2017 DOI: 10.4172/2161-0711.1000567
Abstract
Objectives: The goal of this study is to find out the prevalence of tobacco smoking and environmental exposure with its potential influential factors in healthcare students in King Saud University, in Riyadh, Saudi Arabia.
Methods: It is an observational cross-sectional study, which has been held in King Saud University, Riyadh, Saudi Arabia. This study included 1207 first to fifth year male and female undergraduate healthcare students in all the health colleges, randomly selected according to a list of names with a self-administrated questionnaire during February-March 2017. Descriptive analysis was performed on all data and associations between variables were tested using Chi-square test with statistical significance was set at P-value<0.05.
Results: A total of 1207 healthcare students completed the questionnaire; the prevalence of tobacco product smoking was 13.5%. This study showed variation between the colleges which was highest in the college of nursery 19.23%, and lowest in the college of pharmacy 10.11% with a significant p-value of 0.001. The age group of 18-21 years old, the prevalence was only 9.54%, while the age group of 22-25 was 19.25%, and for 26 years old students or more was 33.33%, which shows a significant difference. One of the major causes of smoking cigarettes was having stress 33.33%. The prevalence of smoking water pipe came to be 12.1% and of small-pipe (Midwakh) 5.6%. The most common cause of smoking water pipe was to enjoy its flavors 43.54% of the participants. The prevalence of students with direct home exposure was 31.48% and environment exposure such as hanging out with friends was 40.93%.
Conclusion: Tobacco consumption is a common problem among healthcare students. As it is known to contain chemicals that increase the risk of many diseases. Thus, a comprehensive program is needed to reduce or stop tobacco product.
Keywords: Healthcare students; Smoking; Prevalence; Water pipe; Small pipe; Environment exposure
Introduction
The usage of tobacco product is a worldwide leading health complication. Near 1.1 billion smokers live in lower and middleincome countries that represents 82% of the world's smokers [1]. In 2014, 5.4 million people died from tobacco-related illness and 80% of those deaths occurred in developing countries [2]. Actually, nowadays smokers aren’t only harming themselves, but they may hurt the people around them as they are considered passive smokers. Passive smoking (PS) or second-hand smoke (SHS) is defined as the inhalation of tobacco particle by nonsmokers against their will by having involuntary exposure to tobacco smoke in public areas [3].
Consumption of tobacco product can lead to many complications, for example, a population with a long duration and massive intensity of cigarette smoking, the ratio of lung cancer attributable to smoking is 90% [4] and 35% increase in the risk among people with tobacco exposure [5]. Also, it is a major risk factor for coronary heart disease where 38.9% of cardiac patients were smokers [6]. A study was conducted in the Middle East from 1994 to 2014, revealed that the prevalence of stroke in smoking population was 19.3% [7]. Also smoking increase the risk of dementia by 1.47% [8]. Moreover, it is known that men who smoked 25 or more cigarettes daily had a relative risk of diabetes of 1.94% [9].
According to our society, cigarette production has been increasing worldwide at an average of 2.2% each year, overcoming the population growth rate of 1.7% [10], making adolescents both male and female smoking ratio increase and popularize. Many people started smoking at an early age out of curiosity and discovering behavior. Approximately 90% of the people who smoke for the first time are adolescents, younger than 18 [11]. Inhalation of nicotine substance from the tobacco product will carry the particles into the lungs, where it is rapidly absorbed into the pulmonary venous circulation. Then the nicotine enters the arterial circulation and moves quickly from the lungs to the brain, where it binds to nicotinic cholinergic receptors making it addictive from a young age and hard to quit [12]. In the developed countries such as the United States, the current cigarette smoking prevalence among adults had declined from 20.9% (45.1 million persons) in 2005 to 16.8% (40.0 million) in 2014, representing a 19.8% decrease [13]. Comparing to Saudi Arabia, the smoking rates reported by averaging statistics from several studies conducted over a 16-year period came to be 35-40% of adult males where 24% of preparatory school students were considered regular smokers [14]. From 1996 through 2012, tobacco consumption rates in Saudi Arabia have risen from 21.9% of males and 0.6% of females to 37% of males and 6% of females [15,16].
An international board review showed that the prevalence of tobacco smoking varies widely among medical students from one region to another. Its prevalence varies among male medical students from 3% in the United States to 53% in Japan. With an overall prevalence of smoking in both the general population and university students ranges from 21% to 25%. Tobacco smoking reported being practiced by approximately 13% of male medical students [17].
In Saudi Arabia, a study was done in 1991 by Taha A. to measure and evaluate the smoking habit on King Saud University students in Riyadh, the sample size was 2264 students, the results were 37% of the students were current smokers, and over 19% smoked more than 15 cigarettes per day (heavy smokers) [18]. In 2000 another study was done by Hasim TJ to measure and evaluate the smoking habits in Saudi Arabia on Medical Science students, the study was done on 647 students, the result came to be that 29% were current smokers [19].
In 2005 a study was done in central Saudi Arabia by Al-Turki YA to estimate the prevalence of smoking habits among male medical students. The study was done on 322 medical students; the results showed that 13% of male medical students were current smokers, 44.1% of these student’s smoke water pipe alone, 32.2% smoke cigarette only, 23.7% smoke both cigarette and water pipe, 5.3% were exsmokers, and 38.2% were passive smokers [20].
In 2011 a study was done in western Saudi Arabia by Wali SO to estimate the prevalence of tobacco smoking among 643 medical students. The prevalence of smoking was 24.8% among males, and 9.1% among females and the prevalence of using water pipe was 11.7% [21].
In 2013 a recent study was done in Riyadh by Almutairi to estimate the prevalence of tobacco use and exposure to environmental tobacco smoke among the Saudi medical students. The study was done on 805 medical students. The results showed the prevalence of experimentation with cigarette smoking was 11.3%. The estimated prevalence of current smoking among the study participants was 4.7% [22].
Regarding small pipe (Midwakh) smoking, we could not see enough studies touching this habit, but a study was conducted in Ajman, United Arab of Emirates about prevalence of small pipe in healthcare students which came to be 11.5% [23]. This is why we included this smoking habit in this study to get some information about its prevalence in our society.
Methodology
This is a survey which depends on observing and analyzing tobacco product prevalence in analytical cross-sectional study among healthcare students that was conducted at five major health colleges (College of Medicine, College of Dentistry, College of Pharmacy, College of Nursing and College of Medical Applied Science) of King Saud University in Riyadh, Saudi Arabia, during time period of February and March 2017. The colleges were stratified according to the type of the specialty and number of registered students.
Sampling
We used this formula for calculating sample size: [ N = Z2 × (P) × (1-P) / D2] where (P) is the average prevalence from previous studies that conducted in our field which is 20% and (Z) is constant value (1.96) with 95% confidence interval, for precision with 80% power (D=0.05). After using this mathematical technique we needed at minimum 246 students to complete the survey.
The questionnaire form was administered and enrolled into undergraduate medical students at their designated courses from the first year to fifth-year in both genders from these health colleges. The total number of the students was 1207 who completed the questionnaire. Microsoft Excel program was used to randomly select the study sample within each year and sex after getting the list of students’ names in each year.
The study was approved by the Institutional Review Board (IRB) of the College of Medicine, King Saud University, and performed in accordance with the ethical standard that was laid down in 1964's Declaration of Helsinki and its later amendments.
Instrumentation
The self-administered questionnaire included many domains, student’s demography (age, gender, attending college and academic year), the consumption prevalence and behavior of various forms of tobacco products such as (cigarettes, water pipe and small pipe). Moreover, the possible leading factor of tobacco usage, the prevalence of environmental and home exposure of passive smoking, the behavior practice of smoking cessation and the possible reasons of smoking abstention has been also included in our study.
The questionnaire form was distributed in English and Arabic for more accuracy, and validated by a consultant in family medicine and in community medicine. The instrument was first pilot tested among 20 healthcare students, for validation purposes in terms of feasibility and clarity and possibility of any changes. The informed consent to the participant was clear and indicated the purpose of the study and the right of the participants to withdraw at any time without any obligation towards the study team. The research study data were distributed; screened and eligible criteria were used for analysis with exclusion of substantial missing or error information in our study.
Statistical analysis
All the Data were analyzed by using Statistical Package for Social Studies (SPSS 22; IBM Corp., New York, NY, USA). Categorical variables were expressed as percentages. Chi-square test was used for categorical variables. A p-value<0.05 was considered statistically significant.
Results
The survey was completed by 1207 students that fulfilled the inclusion criteria from first-year to fifth-year (60.3% males, 39.7% females). The percentage of current tobacco users among healthcare students came to be 13.5%.
Healthcare student’s demographic
Respondents were distributed over different academic years, from (preclinical students) first year 15.7% (190), the second year 32.6% (394) and for (clinical students) third year 22.6% (273), the fourth year 18.6% (224), fifth-year 10.4% (126). The information carried from five health colleges depended on their student ratio distribution: college of medicine 35.2% (425), college of dentistry 12.6% (152), college of pharmacy 15.6% (188), college of medical applied science 25.8% (312) and college of nursing 10.8% (130) as shown in Table 1.
| Details | N=(1207) | % |
|---|---|---|
| Age group | ||
| from 18 to 21 years | 754 | 62.5 |
| from 22 to 25 years | 426 | 35.3 |
| age 26 or more | 27 | 2.2 |
| Gender | ||
| Female | 479 | 39.7 |
| Male | 728 | 60.3 |
| Academic year | ||
| 1st year | 190 | 15.7 |
| 2nd year | 394 | 32.6 |
| 3rd year | 273 | 22.6 |
| 4th year | 224 | 18.6 |
| 5th year | 126 | 10.4 |
| College | ||
| College of Medicine | 425 | 35.2 |
| College of Dentistry | 152 | 12.6 |
| College of Pharmacy | 188 | 15.6 |
| College of Medical Applied science | 312 | 25.8 |
| College of Nursing | 130 | 10.8 |
Table 1: Demographic characteristics of study subjects.
Prevalence and characteristics of smoking tobacco product
The prevalence of tobacco product consumption in males came to be ten times higher than female students as (20.74% for male students and 2.51% for female students) as shown in the Table 2. Most of the tobacco users started smoking less than four years (74.85%).
| Time start using tobacco product | N=163 | Prevalence% | |
|---|---|---|---|
| Less than one year | 19 | 11.66 | |
| From 1 to 2 years | 45 | 27.61 | |
| From 3 to 4 years | 58 | 35.58 | |
| From 5 to 6 years | 21 | 12.89 | |
| From 7 to 8 years | 14 | 8.59 | |
| More than 9 years | 6 | 3.68 | |
| Prevalence of tobacco smoking | No. | Prevalence% | P value |
| Over all | 163 | 13.5 | <0.001* |
| Gender | |||
| Female | 12 | 2.51 | |
| Male | 151 | 20.74 | |
| Age group | |||
| From 18 to 21 years | 72 | 9.54 | <0.001* |
| From 22 to 25 years | 82 | 19.25 | |
| from age 26 or more | 9 | 33.33 | |
| Academic year | |||
| 1st year | 19 | 10 | 0.071* |
| 2nd year | 45 | 11.42 | |
| 3rd year | 47 | 17.22 | |
| 4th year | 35 | 15.63 | |
| 5th year | 17 | 13.49 | |
| College | |||
| College of Medicine | 44 | 10.35 | 0.001* |
| College of Dentistry | 20 | 13.16 | |
| College of Pharmacy | 19 | 10.11 | |
| College of Medical Applied science | 55 | 17.63 | |
| College of Nursing | 25 | 19.23 | |
| *Significant value | |||
Table 2: The prevalence of tobacco smoking among healthcare students.
The highest prevalence was in third year students (17.22%) with a significant difference between the age groups as it increases per age as in group of students between 18-21 years old the prevalence was only (9.54%), among age group between 22-25 it was (19.25%), and for 26 years old students or more it was (33.33%) p-value <0.001. The study also showed variation in prevalence between the colleges as it was highest in nursing college (19.23%) and lowest in the college of pharmacy (10.11%) as shown in Table 2.
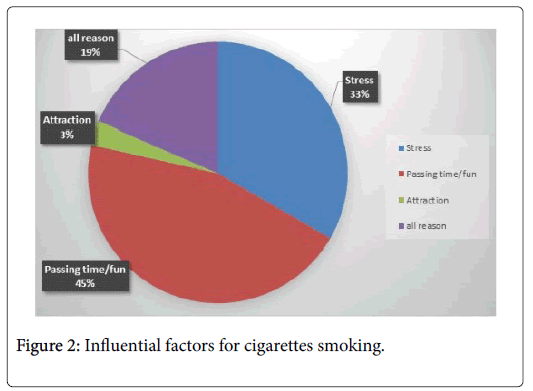
Prevalence and characteristics of smoking cigarettes
The prevalence of smoking cigarettes in these healthcare students were 11.2% and most of them smoke less than 20 cigarettes per day (93.33%) and only 6.66% smoke more than 20 cigarettes in a day. A huge number of the students smoke cigarettes only for fun or just passing time (45.19%) and (33.33%) of the students smoke to reduce their stress and (18.52%) for both reasons. Most of the students smoke their first cigarette after 30 minutes of awakening (61.48%) and (12.59%) less than 10 minutes and (25.93%) in between 10-30 minutes as shown in Table 3.
| Smoking cigarettes | N=135 | Prevalence%=11.2 |
|---|---|---|
| Cigarette per day | ||
| Less than 5 | 35 | 25.93 |
| From 5 to 10 | 32 | 23.53 |
| From 10 to 15 | 31 | 22.96 |
| From 15 to 20 | 28 | 20.74 |
| More than 20 | 9 | 6.66 |
| First cigarette after waking up | ||
| Less than 10 minutes | 17 | 12.59 |
| From 10 to 30 minutes | 35 | 25.93 |
| From 30 to 60 minutes | 30 | 22.22 |
| More than 60 minutes | 53 | 39.26 |
| Reason for smoking cigarettes | ||
| For stress relief | 45 | 33.33 |
| For attraction | 4 | 2.96 |
| For fun or passing time | 61 | 45.19 |
| Stress relief / fun or passing time | 25 | 18.52 |
Table 3: Criteria of smoking cigarettes among healthcare students.
Prevalence and characteristics of smoking water pipe and small pipe (Midwakh)
For the water pipe smokers, the prevalence was 12.1% where the majority of the students smoke water pipe just to enjoy its flavor (43.53%) and (29.25%) of students smoke just for fun or passing time, and only (3.4%) for relieving their stress. More than half of the students (59.86%) smoke water pipe monthly or occasionally and only (8.84%) on a daily use. For smoking a small pipe (Midwakh) the prevalence was lower than the other products as it came to be 5.6%. Half of the students (51.47%) smoke it monthly or occasionally and only (23.53%) on daily uses as shown in Table 4.
| Water pipe | N=147 | Prevalence%=12.1 |
|---|---|---|
| Smoking water pipe | ||
| Daily | 13 | 8.84 |
| From 3 to 4 days per week | 14 | 9.52 |
| Weekends | 32 | 21.77 |
| Monthly (occasionally) | 88 | 59.86 |
| Reason for smoking water pipe | ||
| For stress relief | 5 | 3.4 |
| For attraction | 2 | 1.36 |
| For fun or passing time | 43 | 29.25 |
| To enjoy sheesha flavor | 64 | 43.54 |
| For fun or pass time / enjoy the sheesha flavors | 26 | 17.69 |
| Small pipe | N=68 | Prevalence%=5.6 |
| Smoking small pipe | ||
| Daily | 16 | 23.53 |
| From 3 to 4 days per week | 13 | 19.12 |
| Weekends | 4 | 5.88 |
| Monthly (occasionally) | 35 | 51.47 |
Table 4: Criteria of smoking water pipe and small pipe among healthcare students.
Exposure to tobacco product
The prevalence of tobacco users among students' families came to be (51.14%) in female students and (53.71%) in male students and only (31.48%) of the overall students were exposed by their family member.
The prevalence of students who sit with their family on a daily basis was (8.62%) and monthly or occasionally was (10.27%). Regarding sitting with their friends, (40.93%) of the students sit with them while smoking, and the ratio of male students was 12 times higher than females. Overall students, who sit with them on a monthly basis came to be (11.02%), Table 5.
| Male% total N=728 | Female%Total N=479 | Overall%Total N=1207 | |
|---|---|---|---|
| Family member using tobacco product | |||
| Yes | 53.71(391) | 51.14(245) | 52.78(636) |
| No | 46.29(337) | 48.86(234) | 47.22(571) |
| Siting with family member while using tobacco product | |||
| Yes | 36.54(266) | 25.47(122) | 31.48(380) |
| No | 63.46(462) | 74.52(357) | 68.51(827) |
| Number of tobacco product exposure by family member | |||
| Daily | 9.89(72) | 6.68(32) | 8.62(104) |
| From 3 to 4 days per week | 8.10(59) | 5.85(28) | 7.21(87) |
| Weekends | 7.42(54) | 3.97(19) | 6.49(73) |
| Monthly(occasionally) | 11.13(81) | 8.98(43) | 10.27(122) |
| Sitting with friends while they are using tobacco product | |||
| Yes | 61.26(446) | 10.02(48) | 40.93(494) |
| No | 38.74(282) | 89.98(431) | 59.07(713) |
| Number of tobacco product exposure by friends | |||
| Daily | 16.76(122) | 2.08(10) | 10.94(132) |
| From 3 to 4 days per week | 12.78(93) | 0.63(3) | 7.95(96) |
| Weekends | 16.90(123) | 2.08(10) | 11.02(133) |
| Monthly(occasionally) | 14.84(108) | 5.22(25) | 11.02(133) |
Table 5: Environmental exposure to tobacco product among healthcare students.
Reasons of non-smoking
Many of the respondents didn’t have specific reasons, but the majority (32.85%) they don’t smoke because they assumed that smoking is bad for their health. Other reasons like “I don’t like to smoke” (13.41%), others think that smoking is a bad habit (7.00%), and (26.92%) had all of these reasons. Some students don’t smoke for religious reasons (4.21%), then there were a variety of others reasons as shown in Table 6 all together they occupied (6.98%).
| No. | Prevalence% | |
|---|---|---|
| Reason for non-smoking | 1044 | |
| Don’t like smoking | 140 | 13.41 |
| Smoking is a bad habit | 73 | 7 |
| Smoking affect health | 343 | 32.85 |
| Don’t like smoking / bad habit | 16 | 1.53 |
| Don’t like smoking / affect health | 45 | 4.31 |
| Smoking is a bad habit / affect health | 73 | 7 |
| Don’t like smoking / bad habit / affect health | 281 | 26.92 |
| Others | ||
| Religion reasons | 44 | 4.21 |
| Social reasons | 7 | 0.67 |
| Family reason | 5 | 0.48 |
| Bad smell | 13 | 1.25 |
| Asthma | 3 | 0.29 |
Table 6: Reasons of non-smoking among healthcare students.
Behavior of quitting smoking
The prevalence of Ex-smokers in this study was only 2.73% of the students and the percentage among cigarette smokers' students who did try quitting came to be (74.07%). Near half (45.00%) tried three times or more to quit and the majority (65.19%) plan to quit smoking in the future while (34.81%) have no plan to stop using tobacco consumption. For the water pipe users, half of them (52.38%) didn’t try to quit in the past and almost half these students (48.30%) have no plan to quit in future as shown in Table 7.
| No. | Prevalence% | |
|---|---|---|
| Prevalence of Ex- smokers | 33 | 2.73 |
| Try to quit smoking cigarette in the past N=135 | ||
| Yes | 100 | 74.07 |
| No | 35 | 25.93 |
| Number of times try to quit cigarettes smoking in the past N=100 | ||
| One time | 32 | 32 |
| Two times | 23 | 23 |
| 3 times or more | 45 | 45 |
| Plan to quit smoking cigarette in future N=135 | ||
| Yes | 88 | 65.19 |
| No | 47 | 34.81 |
| Try to quit smoking water pipe in the past N=147 | ||
| Yes | 70 | 47.62 |
| No | 77 | 52.38 |
| Plan to quit smoking water pipe in future N=147 | ||
| Yes | 76 | 51.7 |
| No | 71 | 48.3 |
Table 7: Quitting of smoking among healthcare students.
Discussion
Since the objective of our study is to estimate the prevalence of tobacco consumption among the healthcare students along with the influential risk factors, so among all of the 1207 subjects, the prevalence demonstrated a significant increase in tobacco. However, the correlation of our justified hypothesis implicated some significant controversial outcomes, so the importance of the results might lead to the important need of effective programs in smoking cessation.
The findings from this study proved that the participants of healthcare students have a higher prevalence unlike our hypothesis that assumes the use of tobacco products in healthcare student will be less than 10% depending on the findings of previous studies, however, we found an increment of the percentage by 3.5%.
Significantly in our 2nd hypothesis, we assumed the environmental exposure will be less than 50%, and home exposure less than 15%, the study showed 9.07% decrease in the environmental exposure and 17.15% increment in the home exposure.
In a relationship with similar studies that were conducted in Texas, United States, the prevalence of smoking in healthcare students was higher than our finding with the lowest prevalence healthcare college was nursing college while in our study the nursing college showed the highest by one and half times than in the Unites States [23].
Also, there are other relative findings showed that pharmacy students were lowest in smoking prevalence and this is supported by the study among healthcare students in Hungary [24].
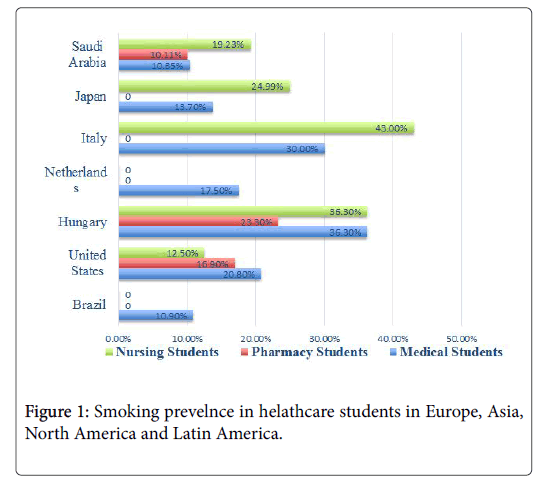
The overall smoking rates showed that the prevalence of smoking among medical students in our study was implicated some significant controversial outcomes compared to the other regions, as it was lower than Japan, Italy, Netherlands, Hungary, United States and Brazil as shown in Figure 1 [25-29].
The previous studies that were conducted in Saudi Arabia supported our findings and have shown that smoking among medical students in eastern and western regions in Saudi Arabia was similar in prevalence. The prevalence, in general, was between 6.8% and 14% [21,30]. These findings supported our study in the central region, which came to be within the same range. All of these results have common point to our finding with the highest prevalence was in the third year.
The prevalence of medical student’s tobacco consumption was noticed to be rising by 6% if compared to a sturdy in King Saud University campus, four years ago, which revealed a significant rising change [22]. The prevalence of water pipe smoking came to be near the prevalence of cigarette smoking and near double the prevalence of small pipe, as most prefer to smoke water pipe in rest places in peripheries of Riyadh especially in social gatherings with friends. Comparing this to the western region, the prevalence of smoking water pipe alone was three times higher than only cigarette smoking [21]. The reasons behind that were related to cultural difference, which has been demonstrated however, more studies might be needed for this smoking habit.
The study also revealed new information that was a relative change from previous studies and new to the region about prevalence and characteristics of smoking a small pipe (Midwakh). Small pipe is a newcomer as tobacco consumption; though the prevalence is still low as compared by the study conducted in Al-Emarat [23] by near 6%, but might be starting to increase in future.
The Prevalence of tobacco environment exposure was almost constant with the previous studies in the region [22], however, there was a significant increase in the prevalence of home exposure in this study by more than double to be a future risk for the healthcare student as it might increase the health hazards from passive smoking. One of the unique features in our study was the number of female participants, most of the previous local studies were limited to only the male gender hence the low number of female participants, because of that various association between genders were well established.
Several studies have demonstrated a strong relationship between stress and smoking such a prospective study held in the United States between 1995 to 2005, which showed that smoking tobacco is an indicator for relationship stress, financial stress, and personal problems [31]. On the contrary, our study showed that one of the big reasons to smoke cigarettes in healthcare students is by having stress as shown in Figure 2, which might lead to create over burden on the future healthcare practitioners.
This research has faced a number of limitations, such as it didn’t seek information regarding the behavior and attitude of tobacco products control nor the student’s knowledge about the smoking complication as it was well documented before. Secondly, this study does not represent all the healthcare students in the country. However, it represents the main portion, as it was held in one of the biggest universities in Saudi Arabia, which thus may be has a great influence and lead to promote health awareness in healthcare institutions and colleges in the region.
Conclusion
The results of this cross-sectional study on smoking prevalence among healthcare students revealed that 13.5% of healthcare students at King Saud University were smokers. Having fun and passing time were identified as the main reasons for smoking and stress was considered the secondary reason. Healthcare schools should educate and train healthcare students on effective strategies in managing stress during their studies. There is a general belief among healthcare students that public tobacco consumption is not well addressed in the healthcare college curriculum, and that they are not trained to implement tobacco cessation programs. Future studies should focus on including more females and more highlight on new tobacco comer, which is the small pipe, as the previous trials have little data regarding them. We recommend including more medical colleges (in addition to King Saud University health colleges) to get a better knowledge, enhance the quality and have more accurate results that could have better reflection of most health college students.
Acknowledgments
The authors gratefully and extend their appreciation to the support of Research Chair, Deanship of Scientific Research, King Saud University, Riyadh, Saudi Arabia.
References
- Gajalakshmi CK, Jha P, Ranson K, Nguyen S (2000) Global patterns of smoking and smoking attributable mortality. Tobacco use and its consequences 11-39.
- WHO (2010) World health report: Health systems financing the path to universal coverage. Geneva, Switzerland.
- Palazzi DL (2012) Etiologies of fever of unknown origin in children 1-21.
- Stewart BW, Kleihues P (2003) World cancer report 2003. International agency for research on cancer.
- Wald NJ, Nanchahal K, Thompson SG, Cuckle HS (1986) Does breathing other people's tobacco smoke cause lung cancer. Br Med J 293: 1217-1222.
- Gikas A, Lambadiari V, Sotiropoulos A, Panagiotakos D, Pappas S (2016) Prevalence of major cardiovascular risk factors and coronary heart disease in a sample of Greek adults: The saronikos study. Open Cardiovasc Med J 10: 69-80.
- Behrouz R, Powers CJ (2016) Epidemiology of classical risk factors in stroke patients in the Middle East. Eur J Neurol 23: 262-269.
- Whitmer RA, Sidney S, Selby J, Johnston SC, Yaffe K (2005) Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 64: 277-281.
- Rimm EB, Chan J, Stampfer MJ, Colditz GA, Willett WC (1995) Prospective study of cigarette smoking, alcohol use, and the risk of diabetes in men. BMJ 310: 555-559.
- Al-Kaabba AF, Saeed AA, Abdalla AM, Hassan HA, Mustafa AA (2011) Prevalence and associated factors of cigarette smoking among medical students at king fahad medical city in Riyadh of Saudi Arabia. J Family Community Med 18: 8-12.
- Tucker JS, Ellickson PL, Klein DJ (2003) Predictors of the transition to regular smoking during adolescence and young adulthood. J adolesc health 32: 314-324.
- Mineur YS, Picciotto MR (2016) Genetics of nicotinic acetylcholine receptors: Relevance to nicotine addiction. Biochem Pharmaco 119: 1-104.
- Jamal A, Homa DM, O'Connor E, Babb SD, Caraballo RS, et al. (2015) Current cigarette smoking among adults-United States, 2005-2014. CDC 64: 1233-1240.
- Al-Haqwi A, Tamim H, Asery A (2010) Knowledge, attitude and practice of tobacco smoking by medical students in Riyadh, Saudi Arabia. Ann Thorac Med 5: 145-148.
- World Health Organization (2011) Report on the global tobacco epidemic 2011. Geneva.
- Jarallah JS, al-Rubeaan KA, al-Nuaim AR, al-Ruhaily AA, Kalantan KA (1999) Prevalence and determinants of smoking in three regions of Saudi Arabia. Tob Control 8: 53-56.
- Smith DR, Leggat PA (2007) An international review of tobacco smoking among medical students. J Postgrad Med 53: 55-62.
- Taha A, Bener A, Noah MS, Saeed A, Al-Harthy S (1991) Smoking habits of king Saud university students in Riyadh. Ann Saudi Med 11: 141-143
- Hasim TJ (2000) Smoking habits of students in college of applied medical science, Saudi Arabia. Saudi Med J 21: 76-80.
- Al-Turki YA (2006) Smoking habits among medical students in central Saudi Arabia. Saudi Med J 27: 700-703.
- Wali SO (2011) Smoking habits among medical students in western Saudi Arabia. Saudi Med J 32: 843-848.
- Almutairi KM (2014) Prevalence of tobacco use and exposure to environmental tobacco smoke among Saudi medical students in Riyadh, Saudi Arabia. J Community Health 39: 668-673.
- Morrell HER, Cohen LM, Dempsey JP (2008) Smoking prevalence and awareness among undergraduate and health care students. Am J Addict 17: 181-186.
- Piko BF (2002) Does knowledge count? Attitudes toward smoking among medical, nursing and pharmacy students in Hungary. J Community Health 27: 269-276.
- Suzuki M, Ohida T, Yokoyama E, Kaneita Y, Takemura S (2005) Smoking among Japanese nursing students: Nationwide survey. J Adv Nurs 49: 268-275.
- Tamaki T, Kaneita Y, Ohida T, Yokoyama E, Osaki Y, et al. (2010) Prevalence of and factors associated with smoking among Japanese medical students. J Epidemiol 20: 339-345.
- Melani AS, Verponziani W, Boccoli E, Trianni GL, Federici, et al. (2000) Tobacco smoking habits, attitudes and beliefs among nurse and medical students in Tuscany. Eur J Epidemiol 16: 607-611.
- Dekker HM, Looman CW, Adriaanse HP, vander Maas PJ (1993) Prevalence of smoking in physicians and medical students, and the generation effect in The Netherlands. Soc Sci Med 36: 817-822.
- Daudt AW, Alberg AJ, Prola JC, Fialho L, Petracco A, et al. (1999) A first step incorporating smoking education into a Brazilian medical school curriculum: Results of a survey to assess the cigarette smoking knowledge, attitudes, behavior, and clinical practices of medical students. J Addict Dis 18: 19-29.
- Al-Mohamed HI, Amin TT (2010) Pattern and prevalence of smoking among students at King Faisal University, Al Hassa, Saudi Arabia. East Mediterr Health J 16: 56-64.
- Slopen N, Kontos EZ, Ryff CD, Ayanian JZ, Albert MA, et al. (2013) Psychosocial stress and cigarette smoking persistence, cessation, and relapse over 9-10 years: A prospective study of middle-aged adults in the United States. Cancer Causes Control 24: 1849-1863.
Citation: Amin HS, Alomair ANA, Alhammad AHA, Altwijri FAA, Altaweel AAA, et al. (2017) Prevalence of Tobacco Product Consumption and Exposure among Healthcare Students in King Saud University in Riyadh, Saudi Arabia. J Community Med Health Educ 7: 567. DOI: 10.4172/2161-0711.1000567
Copyright: © 2017 Amin HS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5192
- [From(publication date): 0-2017 - Apr 07, 2025]
- Breakdown by view type
- HTML page views: 4389
- PDF downloads: 803