Prevalence of Pregnancy Induced Hypertension and Its Bad Birth Outcome among Women Attending Delivery Service
Received: 25-Sep-2017 / Accepted Date: 18-Oct-2017 / Published Date: 25-Oct-2017 DOI: 10.4172/2376-127X.1000355
Abstract
Background: Hypertensive disorders of pregnancy are a major health burden in the obstetric population as it is one of the leading causes of maternal and perinatal morbidity and mortality. World Health Organization estimates that, at least one woman dies every 7 min from complications of hypertensive disorders of pregnancy. Objective: To assess prevalence of pregnancy induced hypertension and bad birth outcome of pregnancy induced hypertension among women attending delivery service at Mizan Tepi university teaching hospital, Tepi and Gebretsadik shawo hospitals, south west Ethiopia. Methods: Health facility based cross-sectional study design was carried out from October 01 to November 30, 2016. The total sample size (422) was proportionally allocated to the three hospitals. Then the study participants were systematically selected from each facility. Prior to analysis, data was entered using Epi data and cleaned and exported in to SPSS version 20.00 and descriptive statistics was computed. Results: The prevalence of pregnancy induced hypertension among women admitted for delivery in the three hospitals were 33 (7.9%), of which 5 (15.2%) were gestational hypertension, 12 (36.4%) were mild preeclampsia, 15 (45.5%) were severe preeclampsia and 3% were eclampsia. Out of the 33 cases, the birth outcome indicates 8 (24.2%) were low birth weight and only 2 (6.1%) were very low birth weight neonates, 3 (9.1%) were stillbirths, 6 (1.4%) had birth asphyxia, 17 (51.5%) were preterm delivery and 7 (21.2%) infants were admitted in neonatal intensive care unit, while 3 (9.1%) were neonatal deaths. Conclusion: The prevalence of pregnancy induced hypertension among women attending delivery service were 7.9%. Bad birth outcome of pregnancy induced hypertension, 24.2% were low birth weight and only 6.1% were very low birth weight neonates and 9.1% were stillbirths.
Keywords: Pregnancy induced hypertension; Delivered women; Bad birth outcome
Abbreviations
ACOG: American Congress of Obstetricians and Gynaecologists; ANC: Antenatal Care; EDHS: Ethiopian Demographic Health Surveys; FMOH: Federal Ministry of Health; HDP: Hypertensive Disorders of Pregnancy; PIH: Pregnancy Induced Hypertension; SOGC: Society of Obstetricians and Gynaecologists of Canada; MTUTH: Mizan-Tepi University Teaching Hospital
Background
Hypertension in pregnancy is defined as a systolic blood pressure ≥ 140 or diastolic blood pressure ≥ 90 mm Hg or both. Both systolic and diastolic blood pressure elevations are important in the identification of Hypertension Disorder of Pregnancy (HDP) [1].
Pregnancy induced hypertension that occurs after 20 weeks of gestation in a woman with previously normal blood pressure. The general classification of pregnancy-induced hypertension during pregnancy are gestational hypertension (without proteinúria), pre-eclampsia (with proteinúria) and eclampsia (pre-eclampsia with convulsions) [2].
Severe preeclampsia in pregnancy is defined as systolic blood pressure ≥ 160 mm Hg or diastolic blood pressure ≥ 110 mm Hg or both. The Society of Obstetric and Gyneacologists of Canada (SOGC) expert consensus suggests that a single reading at this level be confirmed the sever pregnancy induced hypertension within 15 min [3]. Eclampsia is a severe form of pregnancy induced hypertension and women with eclampsia have seizures resulting from the condition [4].
The hypertensive disorders of pregnancy are major contributors to maternal and perinatal morbidity and mortality. Approximately 15% of maternal deaths are attributable to hypertension, making it the second leading cause of maternal mortality in the United States. Severe hypertension increases the mother’s risk of heart attack, cardiac failure, cerebral vascular accidents and renal failure and also fetus is at increased risk from complications such as poor placental transfer of oxygen, fetal growth restriction, preterm birth, placental abruption, stillbirth and neonatal death [2]. Hypertensive disorders represent the most common medical complications of pregnancy with a reported incidence between 5 and 10% and World Health Organization estimates that at least one woman dies every 7 min from complications of hypertensive disorders of pregnancy [5-7].
According to a population based study in South Africa the incidence of hypertensive disorders of pregnancy was 12% and hypertension disorder of pregnancy was the commonest cause of maternal death which contributed 20.7% of maternal deaths [8].
Studies in Ethiopia show that the incidence of hypertension disorder of pregnancy is around 5% of which majority were due to severe preeclampsia and the disorders are major causes of maternal and perinatal morbidities and mortalities [6]. As Ethiopian Demographic Health survey (EDHS) 2016 reported, maternal mortality ratio is 412 deaths per 100,000 live births and pregnancy induced hypertension has a great role for this maternal death [9]. A review study conducted on the causes of maternal mortality in Ethiopia showed that, the proportion of maternal mortality in Ethiopia due to hypertensive disorders between 1980 and 2012 is increased from 4%-29% at different health facilities [10].
The Federal Ministry of Health (FMOH) has applied multi-pronged approaches to reducing maternal and newborn morbidity and mortality by improving access to and strengthening facility-based maternal and newborn services but the maternal morbidity and mortality due to pregnancy induced hypertension was in increasing trend [11].
In Ethiopia, specifically in study areas, there is no clear prevalence of pregnancy induced hypertension and birth outcome of PIH among pregnant women attending delivery service have not been conducted, so this study is proposed to fill this gap.
Methods
Study area and period
The study was conducted in Mizan Tepi University teaching hospital, Tepi and Gebretsadik shawo public hospitals from October 01-November 30, 2016. Mizan Tepi University teaching hospital is located in Bench Maji zone 560 km far from Addis Ababa and Gebretsadik shawo is found on 441 km from Addis Ababa in kefa zone and Tepi hospital is located in sheka zone on 565 km from capital city of Ethiopia, Addis Ababa.
Study design
Health facility based cross-sectional study design with quantitative data collection method was used.
Source and study population
All women admitted to delivery ward of public hospitals in study area considered as source of population and sampled women were study population.
Inclusion and exclusion criteria
All admitted women in delivery ward with gestational age greater than 28 weeks and who can communicate verbally included in the study where as those of critically ill and unable to communicate after full course of treatment and women with known chronic hypertension were excluded from the study.
Sample size determination and sampling techniques
The sample size was calculated by using a single population proportion sample size calculation formula and then the final sample size was 422. The source of population was taken from six month report of deliveries (1030) and the sample size was proportionally allocated to the three public hospitals based on their source of population. Then the study participants were systematically selected from each hospital and admitted mothers for delivery who were eligible to the study were included in the study.
Operational definitions
In this study pregnancy induced hypertension was operationalized as the blood pressures of pregnant women come for delivery service is ≥ 140/90 mm Hg after 28 weeks of gestation, measured two times 6 h apart by trained data collectors and with or without proteinuria, pregnancy induced hypertension includes gestational hypertension, pre-eclampsia and eclampsia.
Instruments and data collection procedure
The data was collected using pre-tested semi-structured questionnaire adapted from validated questionnaire [12-14]. Questionnaires were first adapted in English and translate to Amharic by expert and translated back to english to see consistency of the question. Six data collectors who are degree midwives in qualification and who are fluent in speaking, writing and reading local language were recruited and three supervisors were recruited who are BSc in field of health. Data was collected through face to face interview and reviewing of medical record of the mother and newborn using pretested structured questionnaire by trained data collectors and data were collected day and night not to miss the cases.
Blood pressure readings were taken while the woman was seated in the upright position and supine position using a mercury sphygmomanometer apparatus and for referred women, blood pressure and protein urea at time of diagnosis was taken.
Data processing and analysis
EPI data Statistical software version 3.1 and Statistical Package for Social Sciences (SPSS) software version 21.0 was used for data entry and analysis. After organizing and cleaning the data, frequencies and percentages were calculated to all variables that are related to the objectives of the study.
Data quality control measures
The quality of the data was assured by using validated pre-tested questionnaires. Prior to the actual data collection, pre-testing was done on 5% of the total study eligible subjects and has similar characteristics. Data collectors were trained for one day intensively on the study instrument and data collection procedure that includes the relevance of the study, objective of the study, confidentiality of the information, informed consent and interview technique. The data collectors were work under close supervision of the supervisors to ensure adherence to correct data collection procedures. Supervisors were reviewed the filled questionnaires at the end of data collection every day for completeness. Moreover, the data was carefully entered and cleaned before the beginning of the analysis.
Ethical considerations
Ethical clearance from Mizan Tepi University and permission from respective authorities and written consent of respondents’ was obtained before the data collection. To get full co-operation, respondents were reassured about the confidentiality of their response. They were also ensured their voluntarily participation and right to take part or terminate at any time they wanted. Those mothers developed pregnancy induced hypertension were treated in respective health facilities by case manager.
Results
From 422 questionnaires distributed, 416 were returned which makes 98.6% response rate. Among the total study participants, 155 (37.3%) were age between 20-24 categories, more than half of the respondents were 236 (56.7%) orthodox in religion and 403 (97%) were married in their marital status. Almost half of the study participants were rural 214 (51.4%) in their residence. Regarding their educational level, 150 (36.1%) of the respondents were attended primary school, majority of the respondents 276 (66.3%) were house wife and the 230 (55.3) family sizes of the participants were between 3-4 (Table 1).
| Variables | Frequency (n=416) | Percent | |
|---|---|---|---|
| Age of women | <20 | 54 | 13.0 |
| 20-24 | 155 | 37.3 | |
| 25-29 | 131 | 31.5 | |
| 30-34 | 45 | 10.8 | |
| ³ 35 | 31 | 7.5 | |
| Address of women | Rural | 214 | 51.4 |
| Urban | 202 | 48.6 | |
| Religion | Muslim | 57 | 13.7 |
| Orthodox | 236 | 56.7 | |
| Protestant | 118 | 28.4 | |
| Catholic Other* |
1 4 |
0.2 1.0 |
|
| Marital status | Married | 403 | 96.9 |
| Single Divorced Widowed |
10 2 1 |
2.4 0.5 0.2 |
|
| Educational status | Illiterate | 104 | 25.0 |
| Primary | 151 | 36.3 | |
| Secondary school | 78 | 18.8 | |
| Preparatory school | 26 | 6.2 | |
| Diploma | 47 | 11.3 | |
| Degree and above | 10 | 2.4 | |
| Occupational status | Housewife | 277 | 66.6 |
| Governmental | 69 | 16.6 | |
| NGO | 53 | 12.7 | |
| Self | 17 | 4.1 | |
| Family size | 1-2 | 83 | 20.0 |
| 3-4 | 230 | 55.3 | |
| ≥5 | 103 | 24.8 | |
*Other- neutral.
Table 1: Distribution of the study participants by their socio-demographic characteristics at MTUTH, Tepi and Gebretsadik Shawo Hospitals, South-west Ethiopia, Nov, 2016.
Prevalence of pregnancy induced hypertension
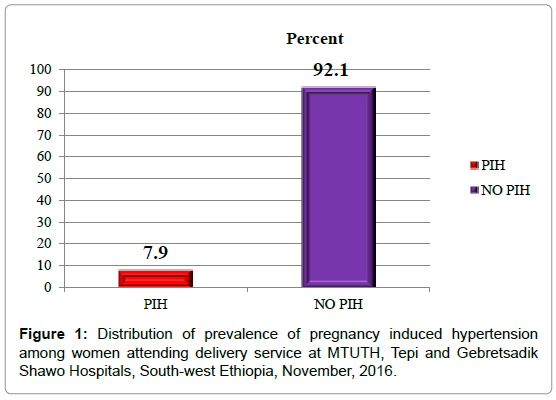
The prevalence of pregnancy induced hypertension among women attending delivery service in the three hospitals of this study was 33 (7.9%).The mean of systolic blood pressure was 110.72 ± 15.315 with the range of 90 mm Hg to 210 mm Hg and the mean of diastolic blood pressure was 72.71 ± 13.093 with range of 50 mm Hg to160 mm Hg. The result of proteinuria ranges from negative to 3+ in dipstick test (Figure 1).
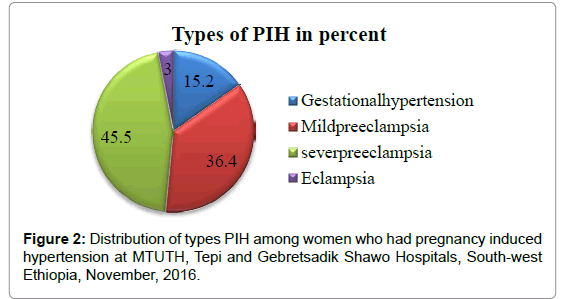
Out of the total of 33 women who had pregnancy induced hypertension, 5 (15.2%) were gestational hypertension, 12 (36.4%) were mild preeclampsia, 15 (45.5%) were severe preeclampsia and 1 (3%) were eclampsia (Figure 2).
| Birth outcome | Frequency (n=33) | Percent | |
|---|---|---|---|
| Low birth weight | Yes | 8 | 24.2 |
| No | 25 | 75.8 | |
| Very low birth weight | Yes | 2 | 6.1 |
| No | 31 | 93.9 | |
| Still birth | Yes | 3 | 9.1 |
| No | 30 | 90.9 | |
| Preterm delivery | Yes | 17 | 51.5 |
| No | 16 | 48.5 | |
| Neonatal death | Yes | 3 | 9.1 |
| No | 30 | 90.9 | |
| Admission to NICU | Yes | 7 | 21.2 |
| No | 26 | 78.8 | |
| Birth asphyxia | Yes | 6 | 1.4 |
| No | 26 | 6.2 | |
Table 2: Bad birth outcomes of PIH among women attending delivery service at MTUTH, Tepi and Gebretsadik Shawo Hospitals, South-west Ethiopia.
Bad birth outcome among mothers developed PIH
Out of the 33 cases, the outcome of PIH indicates 8 (24.2%) were low birth weight and only 2 (6.1%) were very low birth weight neonates, 3 (9.1%) were stillbirths and 6 (1.4%) had birth asphyxia. Almost half 17 (51.5%) were preterm delivery and 7 (21.2%) infants were admitted
Discussion
The prevalence of pregnancy induced hypertension among women attending delivery service in this study was 33 (7.9%). This might increases the morbidity and mortality of the mother and fetus. The prevalence of PIH in this study is similar with the study conducted in India which was 7.8% [15]. And it is slightly lower than the studies done in Iran 9.8%, in Ethiopia Jimma University specialized hospitals 8.48% and Dessie Referal hospital 8.4% [16-18]. This difference is might be due to different in the study period, sample size and also the population might be different in their lifestyle and culture. However the prevalence of this study was still greater than the study done in Ethiopia at Tikur Anbessa hospital which was 5.3% and Mettu Karl hospital 2.4% [6,19].
This discrepancy might be because of different in the study period, sample size and health seeking behaviors of the individual pregnant women. In addition to this, the gap might be due to current health policy which focuses on implementation of focused antenatal care and exempted service for maternal care increases the health care seeking behavior of pregnant women and delivery at health facility which increases detection of the case.
The bad outcome of PIH in this study showed 24.2% were low birth weight and only 6.1% were very low birth weight neonates and 9.1% were stillbirths. This is similar to the study conducted in Ethiopia at Mettu Karl Hospital which shows 24.8% and 3.3% were low and very low birth weight respectively and 10.2 were still births [19]. However it is lower than the study done in Jimma University Teaching Hospitals that indicate 35.6% low and 12.3% very low birth weight neonates , 27.5% stillbirths [17]. This difference is might be due to the study time which means that the current health policy has being intervened to reduce the risk of maternal and neonate morbidity and mortality is effective. Early neonatal death in this study was 3 out of 33 which is greater than the study done in Mettu Karl hospital that was 2 out of 108 [19]. The difference is might be attributed to the difference in resource, quality of newborn care by the skilled and experienced health professionals. The possible limitation of this study was as its descriptive study, the result did not show the association between pregnancy induced hypertension and its independent variables. And also other limitation of this study was bad birth outcome among mothers developed PIH and not developed PIH were not compared.
Conclusion
The prevalence of pregnancy induced hypertension among women attending delivery service was 7.9% which indicates that significant numbers of women attending delivery services at the Mizan Tepi Teaching Hospital, Gebretsadik shawo and Tepi hospitals developed pregnancy induced hypertension. Among pregnancy induced hypertension, severe preeclampsia was the most common. The bad birth outcome of PIH in this study showed that 24.2% low Birth weight, 6.1% were very low birth weight, 9.1% stillbirths and out of 33 births, 3 were early neonatal deaths.
Declarations
Ethical approval and consent to participants
Written ethical approval was obtained from Mizan Tepi University of Institutional Review Board. Permission was obtained from respective health institutions and written consent was obtained from delivery service after discussing the objective of the study.
Availability of data and material
The data sets and/or analysed during the current study is available from the corresponding author on reasonable request. The SPSS data and the questionnaires on which the information’s were collected are available. If the data is needed, we can hyperlink/send the data.
Acknowledgement
The budget of this study was funded by Mizan Tepi University and the researchers of Mizan-Tepi University participated on this study from proposal development, data collection and analysis and writing the manuscript. We would like to express our deepest gratitude to Mizan Tepi University for financially supporting us. Our appreciation also goes to our data collectors, supervisors, Mizan-Tepi university teaching hospital, Tepi and Gebretsadik shawo hospitals and study participants for their valuable contribution in the realization of this study. TA and TM developed a concept of research work, proposal development, data collection, analysis, report writing and writing of the manuscript. All authors read and approved the final manuscript.
References
- Kacica M, Dennison B, Aubrey R (2013) Hypertensive disorders in pregnancy guideline summary. New York State Department of Health.
- DeCherney AH, Nathan L, Goodwin TM (2006) Current diagnosis and treatment in obstetrics and gynecology. The McGraw-Hill, Companies, Inc.
- Menzies J, Magee LA, Li J, MacNab YC, Yin R, et al (2007) Instituting surveillance guidelines and adverse outcomes in preeclampsia. Obstet Gynecol 110: 121-127.
- Parmar MT, Solanki HM, Gosalia VV (2012) Study of risk factors of perinatal death in Pregnancy Induced Hypertension (PIH). Natl J Community Med.
- Prakash J, Pandey LK, Singh AK, Kar B (2006) Hypertension in pregnancy: Hospital based study. J Assoc Physicians India 54: 273-278.
- Teklu S, Gaym A (2006) Prevalence and clinical correlates of the hypertensive disorders of pregnancy at Tikur Anbessa Hospital, Addis Ababa, Ethiopia. Ethiop Med J 44: 17-26.
- Dadelszen P, Magee L (2008) What matters in preeclampsia are the associated adverse outcomes: The view from Canada. Curr Opin Obstet Gynecol 20: 110-115.
- Moodey J (2005) Maternal death associated with hypertensive disorders of pregnancy: A population based study. Hypertens Pregnancy 23: 247-256.
- Central Statistical Agency (CSA), ICF (2016) Ethiopia demographic and health survey 2016: Key indicators report. Addis Ababa, Ethiopia, Rockville, Maryland, USA.
- Berhan Y, Berhan A (2014) Cause of maternal mortality in Ethiopia: A significant decline in abortion related death. Ethiop J Health Sci 24: 15-28.
- Federal democratic republic of Ethiopia ministry of health. Health sector development program IV 2010/2011-2014/2015.
- Kilembe FD (2008) Hypertensive disorders of pregnancy: Prevalence, maternal complications and perinatal outcomes at Lilongwe Central Hospital, Malawi.
- (2009) CDC: Pregnancy risk assessment monitoring system, Phase 6 core questionnaire.
- Fundamental measures of disease occurrence and association. Disease Occurrence.
- Sajith M, Vandana NV, Modi A, Sumariya R, Pawar A (2014) Incidence of pregnancy induced hypertension and prescription pattern of antihypertensive drugs in pregnancy. Int J Pharma Sci Res.
- Khosravi, S, Dabiran, S, Lotfi M, Asnavandy M (2014) Study of the prevalence of hypertension and complications of hypertensive disorders in pregnancy. Open J Prev Med 4: 860-867.
- Wolde Z, Segni H, Woldie M (2011) Hypertensive disorders of pregnancy in Jimma University specialized hospital. Ethiop J Health Sci 21: 147-154.
- Tessema GA, Tekeste A, Ayele TA (2015) Preeclampsia and associated factors among pregnant women attending antenatal care in Dessie Referral Hospital, Northeast Ethiopia: A hospital-based study. BMC Pregnancy Childbirth 15: 73.
- Seyom E, Abera M, Tesfaye M, Fentahun N (2015) Maternal and fetal outcome of pregnancy related hypertension in Mettu Karl Referral Hospital, Ethiopia. J Ovarian Res 8: 10.
Citation: Gudeta TA, Regassa TM (2017) Prevalence of Pregnancy Induced Hypertension and Its Bad Birth Outcome among Women Attending Delivery Service. J Preg Child Health 4: 355. DOI: 10.4172/2376-127X.1000355
Copyright: © 2017 Gudeta TA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11351
- [From(publication date): 0-2017 - Dec 18, 2024]
- Breakdown by view type
- HTML page views: 9834
- PDF downloads: 1517