Prevalence of Malaria Diseases among Pregnant Women at Sudanese Family Planning Association, El-Fateh El-Nour Clinic in El-Obeid City, North Kordofan State, Sudan
Received: 29-Nov-2021 / Accepted Date: 22-Dec-2021 / Published Date: 29-Dec-2021
Abstract
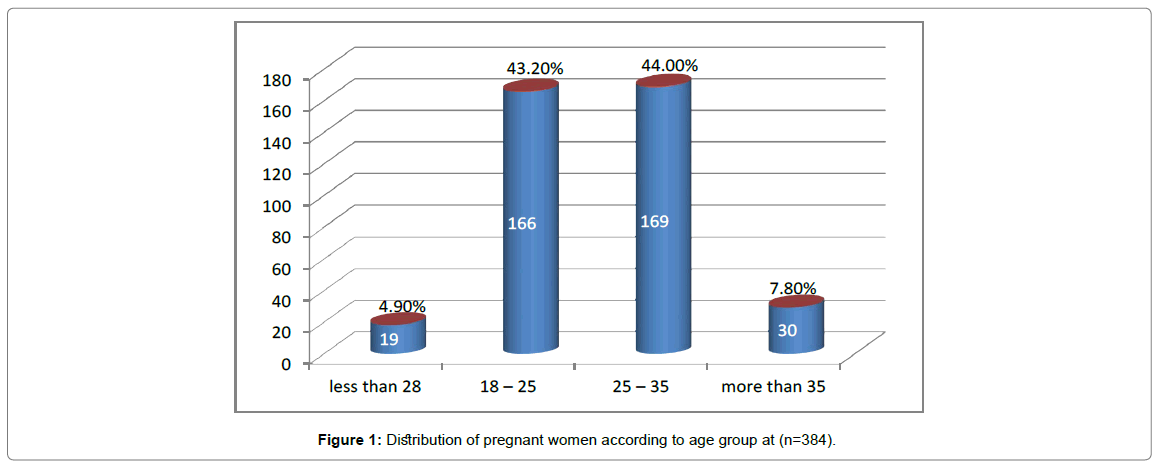
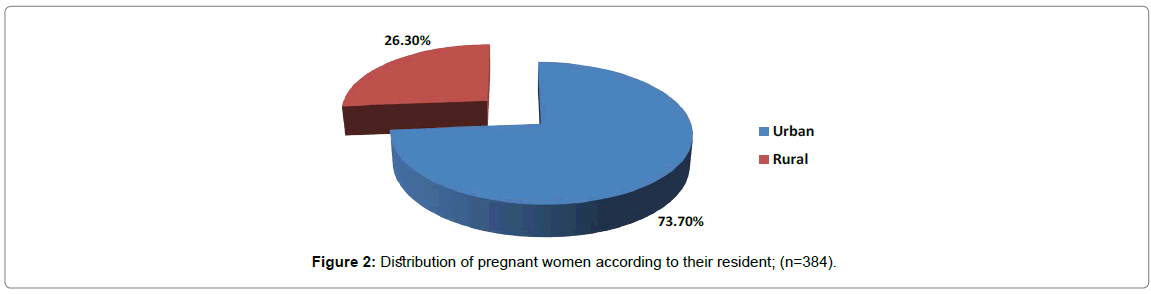
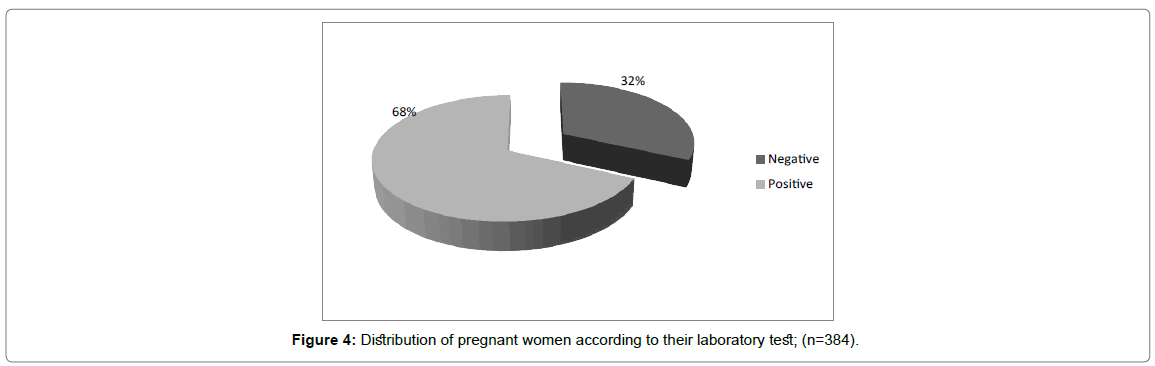
A cross-sectional descriptive institutional based study was conducted among pregnant women admitted to Sudanese family planning association, El-Fateh El-Nour clinic in El-Obeid city, North Kordofan state during dry season from 25 April – 25 June 2021. The study aimed to determine the prevalence of malaria disease and factors associated with repeated malaria among pregnant women. The study covered 384 of pregnant women attending the clinic during study period who had one or more indications for malaria diagnosis. Data was collected using self-administrative questionnaire and microscopic blood test for malaria. Simple random sampling technique was used. Data analyzed and processed using the Statistical Package of Social Sciences (SPSS) version (23.0) and Microsoft Excel (2010) software. Total of (384) pregnant women were selected. More than two third (73.7%) of pregnant women from urban area and (26.3%) from rural area. About (4.9%) of pregnant women fall in the less than 18 years, (43.2%) of them fall in the 18 - 25 years age group, (44%) in the 25 – 35 years age group and (7.8%) were more than 35 years old. Malaria prevalence was (32%). All samples collected from pregnant women showed that Plasmodium falciparum is predominant species. There was highly statistically significant between malaria prevalence and age group (P-value= 0.000, X2= 1.982). There was highly statistically significant between malaria prevalence and gestational age of pregnancy (P-value= 0.000, X2= 3.046). There was highly statistically significant between the malaria prevalence and education (P-value= 0.000, X2= 2.350).
Keywords: Malaria; Prevalence; Pregnant Women; El-Obeid; Kordofan; Sudan
Introduction
Malaria is both an acute and chronic disease caused by protozoa of the genus Plasmodium. Four species cause human malaria: P. falciparum, P. vivax, P. malariae, and P. ovale. The protozoa are transmitted to persons by female mosquitoes of the genus Anopheles [1]. Malaria predominantly affects low and lower income nations and within endemic countries, the poorest and most sidelined communities [2]. Globally, the number of countries that were malaria endemic in 2000 and that reported fewer than 10000 malaria cases increased from 26 in 2000 to 46 in 2019. In the same period, the number of countries with fewer than 100 indigenous cases increased from six to 27. In the period 2010–2019, total malaria cases in the 21 E-2020 countries reduced by 79%. There were more cases in 2019 than in 2018 in Comoros, Costa Rica, Ecuador and Suriname, which reported 1986, 25, 150 and 66 additional cases, respectively [3].
Most of malaria cases and deaths occur in Sub-Saharan Africa, but Asia, Latin America and to a lesser extent the Middle East and part of Europe are also affected. Approximately 25 million pregnant women are at risk of infection by Plasmodium falciparum annually in Africa. About 90% of all malaria mortality in the world today occurs in Africa south of the Sahara (Figure 1). This is because the majority of infections in Africa are caused by P. Falciparum, the most dangerous of the four human malaria parasites. It is also because the most effective malaria vector “the mosquito Anopheles gambiae” is the most prevalent in Africa and the most difficult to control. In areas of stable malaria transmission, very young children and pregnant women are the population groups at highest risk for malaria morbidity and mortality [4]. Apparently there was no difference between male and female. Similarly, the lowermost economic class is at higher risk. Internally displaced people and refugee camps reported prevalence doubled that in rural areas and 3 times higher than that in urban areas. Despite rigorous effort made to control malaria for more than a century. Majority of deaths associated with malaria occur in sub-Sahara Africa among biologically risked groups [5]. In most areas of Africa, P. vivax infection is basically absent because of the hereditary lack of Duffy antigen receptor for chemokines on the surface of red blood cells that is involved in the parasite invasion of erythrocytes (Table 1). Therefore, in Africa, most malaria cases are by P. falciparum and the highest burden of P. vivax infection is in Southeast Asia and South America. Plasmodium falciparum is the most virulent and as such, it is responsible for the majority of malarial mortality, particularly in Africa. Another characteristic feature of P. vivax infection, compared to P. falciparum infection, is persistence of the parasite as dormant liver-stage hypnozoites, causing recurrent episodes of malaria.
| Education | Laboratory Test | No. of Examined | |||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Illiterate | 23 | 30.6% | 52 | 69.4% | 75 |
| Basic | 49 | 29.5% | 107 | 70.5% | 156 |
| Secondary | 32 | 31.7% | 69 | 68.3% | 101 |
| Undergraduate | 16 | 32% | 34 | 68% | 50 |
| Postgraduate | 0 | 0 | 1 | 100% | 1 |
| Religious Education | 0 | 0 | 1 | 100% | 1 |
| Total | 120 | 31% | 264 | 69% | 384 |
| P-value= 0.000 df=5 X2= 2.350 | |||||
Table 1: Relationship between malaria prevalence and education; (n=384).
Malaria in Sudan is a major public Health Problem. Almost, 75% of residents is at risk of developing malaria. Malaria transmission is unstable putting the whole country under the risk of malaria epidemic. The opportunity of epidemic increased with heavy rains, floods and in case of interruption of control activities [6]. It leads to an estimated 7.5-10 million cases and 35000 deaths every year, Plasmodium falciparum is responsible for about > 90% of cases, but other species are also present. Malaria in pregnancy (MIP) in Sudan constitutes a real problem [7]. In 2015, 586,827 confirmed cases were reported from public health facilities out of the estimated 1,400,000 cases (970,000; 1,900,000). As well, 868 deaths were reported out of the estimated 3,500 deaths (130; 6800). The reported malaria cases represent 8.7% and 12.2% of the total outpatient attendance and of hospital admissions respectively. The disease proportional mortality was 4.3% in hospital admissions respectively. The disease proportional mortality was 4.3% in 2015 putting malaria as one of the main causes of death in Sudan. Results of the Sudan Malaria Indicators Survey in 2016 (Sudan MIS 2016), showed an overall parasite prevalence of 5.9% (Table 2). The prevalence is range between <1 in Red Sea, Northern, River Nile and Khartoum States to >20% in Central Darfur State. In South Darfur, West Darfur, Blue Nile and South Kordofan states the prevalence approached or exceeded 10%. The prevalence correlates with age, as children are 3 times more likely to get malaria than adults. The main species is the P. falciparum (pf) representing 87.6% of cases. However, the P. vivax (pv) unexpectedly reaches 8.1% and mixed infection (pf & pv) approached 5%. P. vivax alone plus mixed infection exceeded 15% in North Darfur, West Darfur, South Darfur, River Nile and Khartoum states.
| Age of pregnancy | Laboratory Test | No. of Examined | |||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| 1st Trimester | 31 | 31.6% | 67 | 68.4% | 98 (25.5%) |
| 2nd Trimester | 31 | 31.6% | 67 | 68.4% | 98 (25.5%) |
| 3rd Trimester | 57 | 31% | 127 | 69% | 184 (47.9%) |
| I don’t know | 1 | 25% | 3 | 75% | 4 (1%) |
| Total | 120 | 31% | 264 | 69% | 384 (100%) |
| P-value= 0.000 df=3 X2= 3.046 | |||||
Table 2: Distribution of pregnant women according to gestational age of pregnancy; (n=384).
The prevalence of malaria vector was associated with rainy season when presence of breeding sites although there is malaria incidence during the dry season. Therefore, the solution must be among the environment of the human and his behavior. In El-Obeid town found the parasitemia level was ≥10000 during the rainy season, this level indicates that the town was in high parasitemia level because of prevalence of the vector when there are establishment of temporary breeding sites (Table 3). Malaria in El-Obeid was once considered as the most important disease of human, being widely distributed and causing damage to human health. Transmission of the disease is confined to rainy season, while the frequency of malaria causes peaks after rainy season. In El-Obeid and as in the other part of the region, Plasmodium falciparum considered being the commonest malaria parasite species and Anopheles arabiensis is considered to be the main malaria vector [8]. It is indicated that about 1–3 million mortalities per year, mainly in children and pregnant women, are due to severe malaria caused by P. falciparum [9].
| Variables | Frequency | Percent (%) |
|---|---|---|
| Have you take malaria medication? (n=247) | ||
| Yes | 214 | 86.6% |
| No | 33 | 13.4% |
| What is type of this medication? | ||
| Artemether | 75 | 35% |
| Artesunate | 74 | 34.6% |
| Quinine | 48 | 22.4% |
| Herbal treatment | 8 | 3.7% |
| All sated | 1 | 0.5% |
| Other | 8 | 3.7% |
| How you used the medication? (n=384) | ||
| I completed the doses | 174 | 45.3% |
| I don’t completed doses | 31 | 8.1% |
| Other | 5 | 1.3% |
| I don’t remember | 4 | 1% |
| Not applicable | 170 | 44.3% |
Table 3: Distribution of pregnant women according to prior infection with malaria during pregnancy; (n=384).
Materials And Methods
A cross-sectional descriptive institutional based study was conducted among pregnant women admitted to Sudanese family planning association, El-Faiteh El-Nour clinic in El-Obeid city, North Kordofan state during dry season from 25 April 25 June 2021. The study aimed to determine the prevalence of malaria disease and factors associated with repeated malaria among pregnant women. It covered 384 of pregnant women attending the clinic during study period who had one or more indications for malaria diagnosis. El-Obeid city is the capital of North Kordofan State. Its area has been estimated by 81 km2 and the distance from Khartoum is about 560 km. North Kordofan State is one of the biggest states in Sudan; it is one of the 18 states of Sudan. It has an area of 185,302 km² and an estimated population of 2,920,890 (Table 4).
| Age | Laboratory Test | Total | |||
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Less than 18 | 6 | 31.6% | 13 | 68.4% | 19 |
| 18 – 25 | 52 | 31.1% | 115 | 68.9% | 167 |
| 25 – 35 | 53 | 31.4% | 116 | 68.6% | 169 |
| More than 35 | 9 | 31% | 20 | 69% | 29 |
| Total | 120 | 31.3% | 264 | 69.7% | 384 |
| P-value= 0.000 df=3 X2= 1.982 | |||||
Table 4: Relationship between malaria prevalence and age group; (n=384).
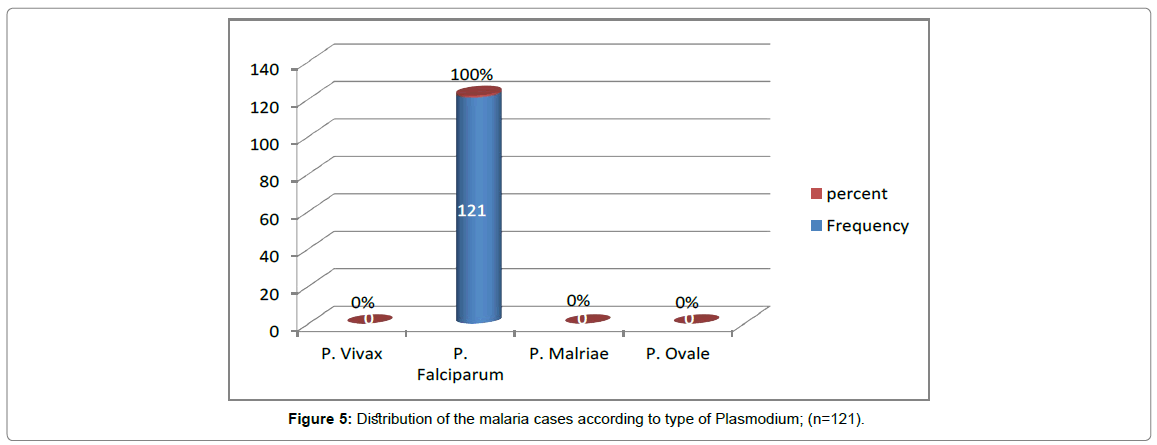
A total of 384 pregnant women were selected for study of malaria prevalence. Sample size was determined by using the following formula:
Where:
n: Sample size,
z: The value of the standard normal variable corresponding to a confidence rate (95%), equal to 1.96
p: Probability value = (0.50),
q: Complement value = (1- 0.50),
d: Marginal of error = (0.05)
Sample Techniques
Peripheral blood samples were collected from pregnant women during the antenatal visits. The microscopically method was used for detection of malaria prevalence. It depends on the identification of parasites on human blood as it is the gold standard method because it is informative (parasite species, stage and density) (Figure 2). Microscopic examination of malaria depends on a proper preparation of a thick & thin blood film stained with Giemsa stain. According to the Standard Operating Procedure (SOP) in malaria diagnosis, the researchers adhered to main steps of stains and staining methods (Giemsa stain); as following [10]:
1. Fix each thin film with methanol.
2. Place the slides back to back in staining trough.
3. Prepare 3% Giemsa stain with buffer solution 7.2 PH.
4. Pour the stain in the trough avoiding pouring it direct to the thick film.
5. Stain for 30 mines.
6. Pour clean water gently to float off the scum of stain and solution of stain become feasible and clean
This method is preferred to use in surveys, research and training purposes.
Data collection
A Blood sample from pregnant women has been collected and had used the microscope to determine the positive and negative samples and determine the type of plasmodium, and using self-administrative questionnaire.
Data processing and analysis
Data was collected and analyzed using the Statistical Package of Social Sciences (SPSS) version (23.0) and Microsoft Excel software (2010).
Results
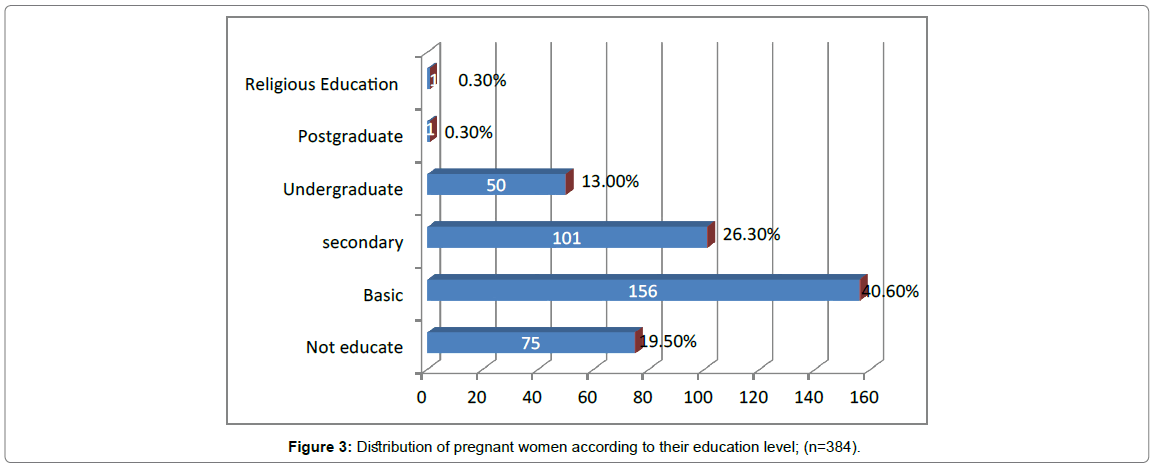
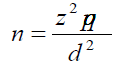
A total of (384) pregnant women were selected, were participated (100%) response rate, among the total participants (73.7%) of pregnant women from urban area and (26.3%) from rural area. About (4.9%) of pregnant women fall in the less than 18 years, (43.2%) of them fall in the 18 - 25 years age group, (44%) in the 25-35 years age group and (7.8%) were more than 35 years old. According to their education level; (40.6%) of pregnant women had education qualified basic school, (26.3%) secondary, (13%) university graduate and (19.5%) illiterate. the prevalence of malaria was 32%, (Figures 3,4). According to the laboratory tests all sample collected from pregnant women showed that Plasmodium falciparum is predominant species (100%) in study area. It was observed that according to gestational age of pregnancy, the prevalence of malaria which was 31.6% during the first trimester and second trimester, and 31% during the third trimester. There was highly statistically significant between malaria prevalence and education (P-value= 0.000, X2= 2.350). Malaria prevalence in women with no education was (30.6%), while in those with basic, secondary and Undergraduate, it was (29.5%), (31.7%), and (32%) respectively (Table 1). There was highly statistically significant between malaria prevalence and gestational age of pregnancy (P-value= 0.000, X2= 3.046) (Table 2). There was highly statistically significant between malaria prevalence disease and age group (P-value= 0.000, X2= 1.982) (Tables 5,6). The obtained result below.
| Did you have completed medication? | Laboratory Test | Total | |
|---|---|---|---|
| Positive | Negative | ||
| I completed all doses | 54 | 120 | 174 |
| I don’t the completed doses | 10 | 21 | 31 |
| I don’t remember | 2 | 3 | 5 |
| Other | 1 | 3 | 4 |
| Not applicable | 53 | 117 | 170 |
| Total | 120 | 264 | 384 |
| P-value= 0.000 df=4 X2= 2.107 | |||
Table 5: Relationship between malaria prevalence and completed doses; (n=384).
Discussion
The study showed that the prevalence of malaria among pregnant women was (32%), This finding is a high because this study was conducted in dry season, in rainy season high relative humidity increases mosquito life-span, thereby increasing the probability of mosquitoes becoming infective. Areas with high rainfall have increased malaria incidence because of an increase in breeding sites. The accompanying high humidity increases survival rates of female anopheline mosquitoes. This finding was in line with a study done among Cameroon pregnant women showed that (33%) of pregnant women suffering from malaria infection. A study carried out in India showed that a positive diagnostic test for malaria was obtained in (5.4%) of the total cohort [12]. The current is lower than that from a study conducted in north-western Nigeria, showed that malaria prevalence was (41.6%) of pregnant women. This result is higher than that found in Ghana, where overall malaria parasite prevalence was (20.4%) (Figure 5).
The present study revealed that the dominant type of plasmodium was P. falciparum. The present finding was higher than that from a study conducted in India, where P. falciparum was identified in 5.4% of the total cohort, [12]. A similar study conducted in Ghana showed that Plasmodium falciparum was the only species identified among the Plasmodium isolates.
The present study discovered that there was highly statistically significant between the prevalence of malaria disease and age group (P-value= 0.000, X2= 1.982). This finding is in disagreement with a study conducted in north-western Nigeria, where age was not significantly associated with malaria prevalence (x2 = 5.27, p = 0.153). The current study revealed that there was highly statistically significant between malaria prevalence and education (P-value= 0.000, X2= 2.350). This result is in line with the study conducted in north-western Nigeria showed that there was a significant association between malaria prevalence and education (x2 = 20.9, p = 0.000), [13].
Conclusion
Plasmodium falciparum is predominant species in study area. Close to third of pregnant women have suffering from malaria. There was highly statistically significant between malaria prevalence and age group (P-value= 0.000). There was highly statistically significant between malaria prevalence and gestational age of pregnancy (P-value= 0.000). There was highly statistically significant between the malaria prevalence and education (P-value= 0.000).
Ethical Considerations
A letter of Identification from the Faculty of Public and Environmental Health, University of Kordofan, El-Obeid was used in pre survey visits made to the State Ministry of Health to obtain permission from the ministry’ authorities. The informed consent of pregnant women was obtained before the commencement of the study. This project was peer- reviewed and approved for funding by Joint EMRO/TDR Small Grants Scheme for Implementation Research in Communicable Diseases. The final report will be submitted to World Health Organization and State Ministry of Health research board. Also the results will be available through Publication in journals.
Acknowledgment
Firstly, the authors are thankful to the World Health Organization and staff member of the Eastern Mediterranean Office (EMRO) and the Special Programmme for Research and Training in Tropical Diseases (TDR). The authors are thankful to the administrations of (University of Kordofan, and State Ministry of Health - North Kordofan for giving permission to conduct this project and staff member of Sudanese family planning association (SFPA) for their collaborate throughout.
Funding
This project was funded by World Health Organization Joint EMRO/TDR Small Grants Scheme for Implementation Research in Communicable Diseases 2020-2021.
References
- Navy Medical Department Center (2000) Guide to Malaria Prevention and Control, Malaria: Disease, Life Cycle, Distribution. 2510 Walmer Avenue Norfolk, Virginia.
- World Health Organization (2020) World malaria report 2020: 20 years of global progress and challenges. The burden of malaria in Africa, 2010.
- Geleta G, Ketema T (2016) Severe Malaria Associated with Plasmodium falciparum and P. vivax among Children in Pawe Hospital, Northwest Ethiopia, College of Natural Sciences, Jimma University, Jimma, Ethiopia.
- Federal Ministry of Health (2017) Malaria Treatment Protocol, Khartoum, Sudan, 42.
- Mohamed ME, Osman K (2004) Malaria in Sudan: past, present and the future. Gezira Journal of Health Sciences 2004: 1.
- Elhag F, Abukashowa S, Abushama H (2015) Parasitemia Level of Falciparum Malaria in Elobied,North Kordofan State, Sudan. Int J Sci Res 5: 868.
- Snow RW, Guerra CA, Noor AM, Myint HY, Hay SI (2005) The global distribution of clinical episodes of Plasmodium falciparum malaria. Nature 434: 214-217.
- Dayananda KK, Achur RN, Gowda CD (2018) Epidemiology, drug resistance, and pathophysiology of Plasmodium vivax malaria, Pennsylvania State University College of Medicine, Hershey, Pennsylvania, USA.
- Federal Ministry of Health (2017) Laboratory Diagnosis of Malaria, Microscopy & Rapid diagnostic tests, Training Manual, Communicable & non Communicable disease control Directorate, Republic of Sudan.
- Sohail M, Shakeel S, Kumari S, Bharti A, Zahid F, et al. (2015) Prevalence of Malaria Infection and Risk Factors Associated with Anaemia among Pregnant Women in Semiurban Community of Hazaribag, Jharkhand, India. BioMed Res Int Vol 2015: 740512.
- Abdullahi FS, Abubakar BMD, Aliyu AS, Umar IA, Usman NS (2015) Prevalence and risk factors associated with malaria infection among pregnant women in a semi-urban community of north-western Nigeria. Infect Dis Poverty 4: 24.
- Azizi MA, Nadia NAC, Cédric Y, Igor SFE, Christian NO, et al. (2020) Comparative Study of Malaria Infections and Associated Risk Factors among Pregnant and Non- Pregnant Women in the Town of Foumbot, Western Region- Cameroon.
Citation: Tigaidi HBG, Ahmmed HAS, Mohammed MAO, Hammad KAE (2021) Prevalence of Malaria Diseases among Pregnant Women at Sudanese Family Planning Association, El-Fateh El-Nour Clinic in El-Obeid City, North Kordofan State, Sudan. J Preg Child Health 8: 504.
Copyright: © 2021 Tigaidi HBG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4420
- [From(publication date): 0-2021 - Jan 30, 2025]
- Breakdown by view type
- HTML page views: 3873
- PDF downloads: 547