Prevalence of Low Birth Weight in Districts of Gujarat: A Temporal Comprehensive Study Based on Health Management Information System Data
Received: 26-May-2022 / Manuscript No. ECR-22-63400 / Editor assigned: 30-May-2022 / PreQC No. ECR-22-63400 / Reviewed: 13-Jun-2022 / QC No. ECR-22-63400 / Revised: 17-Jun-2022 / Manuscript No. ECR-22-63400 / Published Date: 24-Jun-2022 DOI: 10.4172/2161-1165.1000444
Abstract
Background: Globally 20.5 million babies suffered from low birth weight (LBW) and about four million deaths per year are caused by the same. LBW prevalence is higher in the developing countries compared to the developed ones. The present study investigates the district wise prevalence of LBW in last two years (2019-20 & 2020-21) along with spatial-temporal changes taken place between the times in districts of Gujarat.
Materials and Methods: The present study has used HMIS data (2019-20 and 2020-21) which is the official facility-based health service data source given by Ministry of Health and Family Welfare (MoHFW), Government of India. Arc-GIS 10.8 has been used to show the spatial prevalence and spatial-temporal changes of LBW.
Results: The prevalence of LBW has increased from 12.9% to 13.4% in between the year 2020 to 2021 in Gujarat. Only 39% of districts (13 districts) show the decreasing pattern and 61% of districts (21 districts) show increasing pattern of LBW in between 2019-20 to 2020-21 which is indicative of serious problems existing in those districts. Morbi district shows the highest improvement in LBW prevalence followed by Surendranagar, Gir Somnath, and Kheda etc. On the other hand, Navsari district represents the highest increase in the prevalence of LBW followed by Mahesana and Jam Nagar etc.
Conclusion: The study highlights the most vulnerable districts of LBW prevalence from Gujarat. So policy makers can implement a policy for the high prevalence districts and districts which have shown increase in LBW prevalence - to reduce the risk for the same in Gujarat.
Keywords
Low Birth Weight; Prevalence; Spatial temporal changes; Arc-GIS; Vulnerable
Introduction
Low birth weight (LBW) has become one of the major public health challenges on maternal and child health for both developed and developing countries. It is the single most important factor that determines the chances of child-survival; the neonatal mortality rate is about 20 times higher for LBW babies [1].
Birth weight is defined as the first weight of an infant obtained within the first hour of birth. It is one of the indicators of health of a new-born. Along with the health status at infancy and childhood, birth weight is also an indicator of a child’s health in later life. A full size infant is one whose birth weight is 2500 gm or more. Birth weight less than 2500 gm is considered as low birth weight [2].
Globally 20.5 million babies suffered from LBW in 2015 [3]. As per the UNICEF, 2009 report 27% of new-borns in India are of LBW and also the death rate is high among them during the first year of life [4]. Globally, about four million deaths per year are caused by low birth weight. Compared to the infants with normal birth weight, the infants with low birth weight are more likely to die within four weeks of birth [5]. In India, birth weights of 78 percent of the live births occurring in the past five years were obtained in the fourth round of National Family Health Survey. Within those live births, 18 percent new-borns had a low birth weight. Although the prevalence of low birth weight has reduced from 22 percent during NFHS-3 to 18 percent in NFHS-4, still the prevalence of low birth weight is high in India as compared to several other countries [6,7].
The prevalence of the same is higher in the developing countries compared to the developed countries. Prevalence of low birth weight in world is about 15 percent which is below the prevalence of low birth weight in India.
Many studies have demonstrated the risk factors associated with LBW such as, biological [8-10] demographic [11,12], nutritional [13- 15], or socio-economic [16,17], in different regions of the world.
Females with low birth weight have an additional risk of having smaller babies when they become mothers. Many studies show that, maternal age, mother’s poor health and nutrition conditions, the total number of antenatal visits, physical activities during pregnancy, height and weight during pregnancy, maternal education, and per capita income of the household determin the LBW of newborns [18-21]. A study based on Gujarat reported that Out of 404 infants born during the study period, 26.7% were premature (<37 weeks gestation) and 29% were of low birth weight [22].
The LBW is one of the major health issues in developing countries including India. Due to the fact that around half of the Asian LBW new-borns are born in India, there is a need for developing a policy which can subjugate the severity of the issue. One of the Sustainable Development Goals (SGD 3.2) aim to reduce the preventable deaths of new-borns and neonatal mortality to at least as low as 12 per 1000 live births by 2030 [23]. The National Health Policy of India targets to reduce the neo-natal mortality to 16 and still birth rate to “single digit” by 2025 [24].
HMIS is the largest source of vital statistics based on the public health facilities in India. The present study investigates the district wise prevalence of LBW in last two years (2019-20 & 2020-21) along with spatial-temporal changes taken place between the time in districts of Gujarat.
Materials & Methods
The present study will use HMIS data which is the official facilitybased health service data source given by Ministry of Health and Family Welfare (MoHFW), Government of India. HMIS extracts the consolidated data from the Health Sub-Centres, Primary Health Centres, Community Health Centres, Sub-Divisional Hospitals and District Hospitals throughout the country. Arc-GIS 10.8 has been used to show the spatial prevalence and spatial-temporal changes of LBW in two successive years (i.e., 2019-20 & 2020-21).
We have used the HMIS data of years 2019-20 to 2020-21 for estimating the prevalence of LBW in Gujarat. The HMIS provide information on population health including elements associated with the delivery services i.e., no of delivery conducted, no of live birth, no of new born weight <2.5 kg etc. We have used LBW prevalence data of Gujarat and used for the study.
Results
Geographical variation of Low-Birth-Weight Babyis in districts of Gujarat in 2020-21
The result shows the prevalence of low birth weight (LBW) babies in Gujarat across all districts (Table 1). The prevalence of LBW has increased from 12.9% to 13.4% from the year 2019-20 to 2020-21 in Gujarat. In 2019-20 the prevalence of LBW was the highest in Morbi (28.9%) district and lowest in Surat (7.4%) district of Gujarat. In 2020- 21, Valsad (25.2%) represents the highest prevalence whereas Gir Somnath (7.9%) has the lowest. Changes result show that the highest negative change has been taken place in Morbi (-17.01%) district and lowest in Vadodara (-0.52%) district of Gujarat from the year 2019-20 to 2020-21. Furthermore, Navsari (12.1%) district shows the highest positive change whereas Bhavnagar (0.4%) has the lowest between the same time periods.
| Districts of Gujarat | % New-borns having weight less than 2.5 kg to New-borns weighed at birth | ||
|---|---|---|---|
| 2019-20 | 2020-21 | Temporal Changes (2020-21) | |
| Ahmadabad | 12.5 | 11 | -1.55 |
| Amreli | 10.3 | 10.9 | 0.61 |
| Anand | 13.7 | 16.7 | 2.96 |
| Arvalli | 14.3 | 17.6 | 3.33 |
| Banas Kantha | 13.1 | 11.5 | -1.6 |
| Bharuch | 15.4 | 21.2 | 5.78 |
| Bhavnagar | 8.9 | 9.3 | 0.4 |
| Botad | 10.6 | 8.6 | -1.97 |
| Chhotaudepur | 11.2 | 13.8 | 2.57 |
| Dang | 9.9 | 17.3 | 7.43 |
| Devbhumi Dwarka | 10.6 | 18.3 | 7.71 |
| Dohad | 16 | 10.7 | -5.29 |
| Gandhinagar | 9.6 | 16.9 | 7.33 |
| Gir Somnath | 17.1 | 7.9 | -9.21 |
| Jamnagar | 10.3 | 18.6 | 8.34 |
| Junagadh | 8.2 | 12.9 | 4.68 |
| Kachchh | 8 | 9.5 | 1.52 |
| Kheda | 15.5 | 9.1 | -6.41 |
| Mahesana | 9.9 | 18.6 | 8.65 |
| Mahisagar | 11.2 | 13.6 | 2.41 |
| Morbi | 28.9 | 11.9 | -17.01 |
| Narmada | 21.5 | 24.1 | 2.59 |
| Navsari | 10.2 | 22.3 | 12.07 |
| Panch Mahals | 12.1 | 9.1 | -2.97 |
| Patan | 9.8 | 13.2 | 3.42 |
| Porbandar | 15.7 | 10.4 | -5.35 |
| Rajkot | 17 | 15.7 | -1.29 |
| Sabar Kantha | 12 | 14.7 | 2.73 |
| Surat | 7.4 | 11.7 | 4.32 |
| Surendranagar | 20.7 | 8.7 | -12.03 |
| Tapi | 24.4 | 23.4 | -1.01 |
| Vadodara | 16.1 | 15.6 | -0.52 |
| Valsad | 23.7 | 25.2 | 1.48 |
| Gujarat | 12.9 | 13.4 | 0.47 |
| Source: Health Management Information System (HMIS, 2019-20 and HMIS, 2020-21) | |||
Table 1: prevalence of Low Birth Weight (In Percentage) of all districts of Gujarat, India.
Spatial pattern of Low-birth-weight babies in districts of Gujarat in 2019-20 and 2020-21
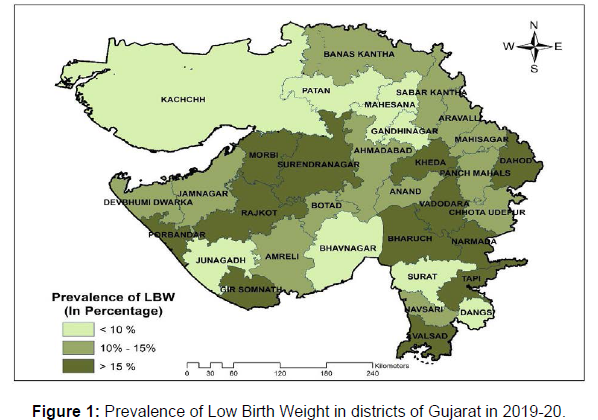
In (Figure 1), the prevalence of LBW of all districts of Gujarat has been demonstrated for the year 2019-20. Out of 33 districts, 12 districts (i.e Morbi, Tapi, Valsad, Narmada, Surendranagar, Gir Somnath, Rajkot, Vadodara, Dohad, Porbandar, Kheda and Bharuch) have a higher prevalence (more than 15%) of LBW in Gujarat. Whereas 8 districts (i.e Surat, Kachchh, Junagadh, Bhavnagar, Gandhinagar, Patan, Dang and Mahesana) show the low prevalence (less than 10%) of LBW in the same year. Remaining 13 districts belong to the range between 10% to 15% prevalence of LBW.
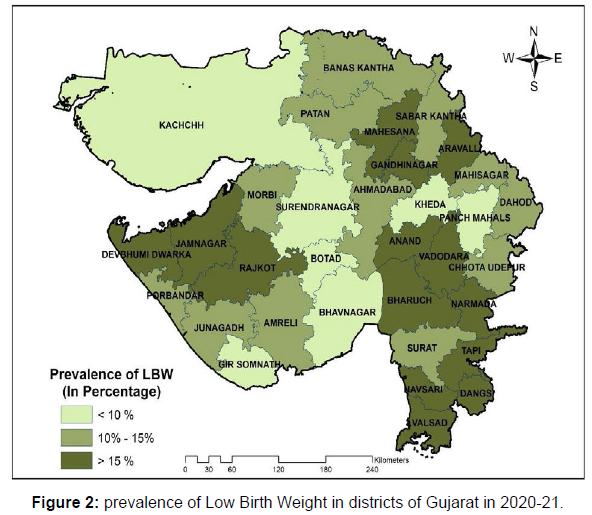
Figure 2 represents LBW prevalence of 2020-21 for all districts of Gujarat. Out of 33 districts 14 districts (Valsad, Narmada, Tapi, Navsari, Bharuch, Jamnagar, Mahesana, Devbhumi Dwarka, Aravalli, Dang, Gandginagar, Anand, Rajakot and Vadodara) show high (more than 15%) prevalence of LBW whereas, 7 districts (i.e Gir Somnath, Botad, Surendranagar, Panch Mahals, Kheda, Bhavnagar and Kachchh) show low (less than 10%) prevalence. Remaining 12 belong to the range between 10% to 15% of LBW.
Temporal changes on LBW in districts of Gujarat
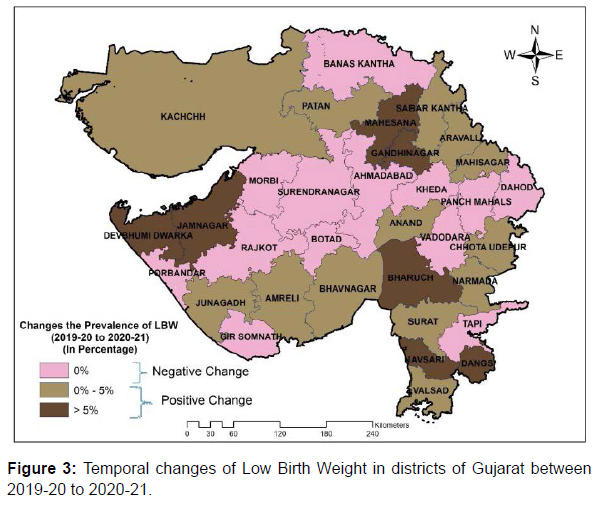
Figure 3 shows the temporal changes of prevalence of LBW between 2019-20 and 2020-21 in all districts of Gujarat. Out of 33 districts, only 39% of districts (13 districts) have shown negative changes (decreased the prevalence between the year) in LBW prevalence in Gujrat between the time. For an example Morbi district shows the highest reduction in LBW from 2019-20 to 2020-21 followed by Surendranagar, Gir Somnath, Kheda, Porbandar, Dohad, Pamch Mahals, Botad, BanasKantha, Ahmedabad Rajkot, Tapi and Vadodara. On the other hand, 61% of districts (remaining 21 districts) show positive changes between the times. The increase in LBW has been the highest in Navsari (12.1%) followed by Mahesana (8.7%) and JamNagar etc. Out of the 21 districts with positive changes in LBW prevalence, 7 belong to the high-level (More than 5%) prevalence whereas 14 are in the group of low level (less than 5%) of LBW prevalence across the different districts of Gujarat.
Discussion
The analysis has been carried out using HMIS data of all districts of Gujarat and tried a spatial-temporal comparison with the latest published HMIS, 2019-20 and HMIS, 2020-21-data of Gujarat. The average prevalence of LBW shows an impressive picture in Gujarat state. But insight into the prevalence level across all districts shows significant changes. Only 39% of districts (13 districts) show the decreasing pattern and 61% of districts (21 districts) show increasing pattern of LBW in between 2019-20 to 2020-21 which is indicative of serious problems existing in those districts. Hence district level policy needs to be implemented targeting specific child birth health issues.
The prevalence of LBW has increased from 12.9% to 13.4% in between the year 2020 to 2021 in Gujarat (HMIS). The results of spatial prevalence maps highlighted that in 2019-20 only 12 districts were in the high prevalence range (>15%) of LBW; which has changed -to 14 districts in this category in 2020-21.
When we come - to the spatial-temporal changes of LBW it shows a significant result. The prevalence of LBW has - increased by 0.5% between the time period. Out of 33 districts of Gujarat, 13 districts show- negative change in LBW (decrease in the prevalence) prevalence and 21 districts show- positive change in LBW (increase in the prevalence) in between 2019-20 to 2020-21.
Morbi district shows the highest improvement in LBW prevalence followed by Surendranagar, Gir Somnath, Kheda, Porbandar, Dohad Pamch Mahals, Botad, Bans Kantha, Ahmedabad Rajkot, Tapi and Vadodara. On the other hand, Navsari district represents the highest increase in the prevalence of LBW followed by Mahesana and Jam Nagar, Devbhumi Dwarka, Dang, Gandhinagar, Bharuch, Junagadh, Surat, and Patan etc.
The preventable interventions like increase in mother education [25,26], media –exposer, intake of iron tablets, mother nutrition, full ANC long birth interval can help to prevent the incidence of LBW. Such meassures can be adopted with a special focus on those districts which are showing increase in prevalence overtime.
Conclusion
prevalence from Gujarat. The study has used spatial tools to present the temporal changes in two points of time. The districts which have shown positive changes in LBW status - indicate- - improvements in terms of interventions and initiatives taken by state and central government. However, few - districts have shown negative changes which means that the necessary strategies were not - sufficient for prevention of LBW prevalence. Therefore, state government must focus on specific districts where prevalence is high and launch- various programmes and schemes -, especially programmes related to maternal and child health (MNCH) and Integrated child development (ICDS) programme and prevent LBW status in Gujarat.
The study will help to identify the high LBW prevalence districts of Gujarat for the given study period along with the temporal changes. So policy makers can implement a policy for the high prevalence districts and districts which have shown increase in LBW prevalence - to reduce the risk for the same in Gujarat.
References
- WHO (2004) Towards the development of a strategy for promoting optimal fetalgrowth. Geneva: World Health Organization.
- Wardlaw TM (Ed) (2004) Low birthweight: country, regional and global estimates. Unicef.
- UNICEF (2019) Monitoring the situation of children and women.
- UNICEF (2009) State of the world's children: Celebrating 20 years of the convention on the rights of the child: Unicef.
- Singh G, Chouhan K, Sidhu K (2009) Maternal factors for low birth weight babies. Med J Armed Forces India 65: 10-12.
- IIPS (2007) National Family Health Survey (NFHS-3) 2005-06. International Institute for Population Sciences, Mumbai, India.
- IIPS (2017) National Family Health Survey (NFHS-4) 2015–16. International Institute for Population Sciences (IIPS), Mumbai, India.
- Amory JM, Adams KM (2004) Adverse outcomes after preterm labor are associated with tumor necrosis factor-α polymorphism−863, but not−308, in mother-infant pairs. Am J Obstet Gynec 191:1362-1367.
- Monden CW & Smits J (2009) Maternal height and child mortality in 42 developing countries. Am J Hum Biol 21: 305-31.
- Prasad M, Al-Taher H (2002) Maternal height and labour outcome. J Obstet Gynaecol 22: 513-515.
- DeKeyser N, Josefsson A, Bladh M, Carstensen J (2012) Premature Birth and Low Birthweight are Associated with a Lower Rate of Reproduction in Adulthood: A Swedish Population-Based Registry Study. Hum Reprod 27: 1170-1178.
- Tema T (2006) Prevalence and Determinants of Low Birth Weight in Jimma Zone, Southwest Ethiopia. East Afr Med J 83: 34-37.
- Black RE, Allen LH, Bhutta ZA (2008) Maternal and Child Undernutrition: Global and Regional Exposures and Health Consequences. The lancet 371: 243-260.
- Frederick IO, Williams AS, Sales AE (2008) Pre-Pregnancy Body Mass Index, Gestational Weight Gain, and Other Maternal Characteristics in Relation to Infant Birth Weight. Matern Child Health J 12: 557-567.
- Kumar VS, Jeyaseelan L, Sebastian T (2013) New Birth Weight Reference Standards Customised to Birth Order and Sex of Babies from South India. BMC preg and child 13: 1-8.
- Elshibly EM, Schmalisch G (2008) The Effect OF Maternal Anthropometric Characteristics and Social Factors On Gestational Age and Birth Weight In Sudanese New born Infants. BMC Public Health 8: 1-7.
- Ohlsson A, Shah P (2008) Determinants and Prevention of Low Birth Weight: a Synopsis of the Evidence. Appl Health Econ 5:45-48.
- Metgud CS, Naik VA, Mallapur MD (2012) Factors Affecting Birth Weight of a Newborn–a Community Based Study in Rural Karnataka, India. PloS one 7: e40040.
- Malhotra N, Upadhyay RP, Bhilwar M (2014) The Role of Maternal Diet and iron-folic acid supplements in influencing birth weight: evidence from India’s National Family Health Survey. J Trop Pediatr 60: 454-460.
- Shashikantha SK, Sheethal MP (2016) Prevalence of low birth weight and its associated factors: a community based cross sectional study in a rural area of Rohtak, Haryana, India. Int J Community Med Public Health 3: 1544-1546.
- Kumari N, Algur K, Chokhandre PK (2021) Low birth weight among tribal in India: evidence from National Family Health Survey-4. Clin Epidemiol Glob 9: 360-366.
- Godbole NB, Moberg MS, Patel P (2020) Paternal Involvement and Adverse Birth Outcomes in South Gujarat, India. Matern Child Health J 9: 161-162.
- UNDP (2020) Sustainable Development Goals – 2030, Department of Economic and Social Affairs, Sustainable Development, United Nations.
- Government of India (2017) National Health Policy, Ministry of Health and Family Welfare, Government of India.
- Bharati P, Pal M, Bandyopadhyay M, Bhakta A (2011) Prevalence and causes of low birth weight in India. Malays J Nutr 17:45-46
- Kader M, Perera NKP (2014) Socio-economic and nutritional determinants of low birth weight in India. N Am J Med Sci 6: 302.
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Google Scholar, Indexed at, Crossref
Citation: Ghosh K, Pandya SV, Desai GS, Panchal NV (2022) Prevalence of Low Birth Weight in Districts of Gujarat: A Temporal Comprehensive Study Based on Health Management Information System Data. Epidemiol Sci, 12: 444. DOI: 10.4172/2161-1165.1000444
Copyright: © 2022 Ghosh K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2028
- [From(publication date): 0-2022 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1658
- PDF downloads: 370