Prevalence and Factors Associated with Underweight, Overweight and Obesity among Students of the University of Lomé, Togo In 2018
Received: 02-Apr-2020 / Accepted Date: 27-Apr-2020 / Published Date: 04-May-2020 DOI: 10.4172/2165-7904.1000398
Abstract
Background: With the westernization of lifestyle, sub-Saharan Africa is facing a double burden of malnutrition with the coexistence of overnutrition and undernutrition. There is a lack of data among youth who represent a target population for early intervention. The objective of this study was to estimate the prevalence and factors associated with underweight, overweight and obesity among students of the University of Lomé in 2018. Methods: A cross-sectional study was conducted from September to December 2018 in the Department of Preventive Medicine of the University of Lomé. Students aged ≥ 18 years and who underwent routine medical examination at the time of registration were included. Information collected included socio-demographic characteristics, anthropometrics, clinical and biological data. Screening for overweight was carried out by calculating the body mass index and multinomial regression analyzes were performed. Results: A total of 37,682 students (32.9% of females) with median age 22 years, (Interquartile Range (IQR): 20- 24) were enrolled. The overall prevalence of excess weight condition (overweight/obesity) among students was 14.8% (95% Confidence Interval (95% CI): 14.4-15.1) and the prevalence of underweight was 8.7% (95%CI: 8.4-8.9). Factors associated with overweight/obesity were high blood pressure (Adjusted Odds Ratio (aOR)= 2.65; 95%CI: 2.40-2.91) and high blood sugar level (aOR= 1.54; 95%CI: 1.18-2.01). Female students not only (aOR= 3.64; 95%CI: 3.42-3.87) were more likely to be overweight and obese but also underweight (aOR= 1.74; 95%CI: 1.61-1.87). Increasing age was a protective factor for underweight (p<0.05). Conclusion: In view of these results, measures must be taken for the establishment of programs to fight overweight and obesity in Togo, especially among young people.
Keywords: Underweight; Overweight; Obesity; Prevalence and factors associated; Students; Lomé
Abbreviations
95%CI: 95% Confidence Interval; aOR: Adjusted Odds Ratio; BMI: Body Mass Index; BP: Blood Pressure; IQR: Interquartile Range
Introduction
The double burden of malnutrition is characterized by the coexistence of undernutrition and overnutrition. In 2014, approximately 462 million adults worldwide were underweight and in 2016, more than 1.9 billion adults were in excess weight condition with over 650 million of them being obese [1,2]. Before 2010, Africa region was the only continent where obesity was not a public health problem [3]. With the westernization of lifestyle, this region of the world is facing a double burden of malnutrition [4,5] and in some urban areas of Africa, the prevalence of obesity is close to 30% [6]. In West Africa, the number of people with overweight or obesity in 2018 was estimated to 52 million, of whom 35% were in urban areas with prevalence of overweight and obesity in adult population respectively 17.6% and 7.6% in 2018 [7]. Also, in Africa, undernutrition remains a concerning issue with 25 countries over 47 in that region of the world which have high (>30%) or very high (>40%) rates of stunting [8]. According to a study on child malnutrition in sub-Saharan Africa, the prevalence of malnutrition was highest in countries in East Africa and West Africa compared to the Millennium Development Goals target for 2015 [9].
Both undernutrition and overnutrition are linked with adverse health conditions. Underweight, overweight and obesity are linked to high mortality and morbidity rates [10]. Complications associated with overweight and obesity, especially diabetes and cardiovascular diseases result in the death of at least 2.8 million people each year [11]. These complications are often associated to elderly persons, but it has been reported that 15 million deaths attributed to non-communicable diseases occur between 30 and 69 years [12], hence the value of early detection and adequate management of risk factors such as overweight and obesity in school or students. Northern countries have become aware of the health impact of obesity and have implemented the policies necessary to manage it, unlike sub-Saharan African countries where there is lack of preventive and therapeutic policies [6]. Wasting, stunting and underweight are expressions of undernutrition and represent anthropometric indicators for the assessment of a child’s nutritional status [9]. According to a study by Wesenbeeck, nearly 110 million people in West Africa do not have adequate food to meet their nutritional needs. Main undernutrition-related adverse health outcomes include deficiencies in calories, protein and vitamins, and low immune response leading to vitamin-specific diseases, impaired physical and cognitive development, and increased risk of infection and death [13,14]. Moreover, undernutrition in early life has been found to be associated with chronic diseases such as diabetes mellitus, hypertension, and coronary heart disease in adulthood [14].
In Africa, few studies have described underweight, overweight and obesity among young people, especially students and children of school age. In Douala, Cameroon and Abidjan, Côte d’Ivoire the prevalence of obesity among University students was 4.1% and 1.1%, respectively, and the prevalence of overweight in Abidjan was 20.5% [15,16]. In Lubumbashi, Democratic Republic of Congo, among students surveyed in primary and high schools, 8% were overweight and 1% were obese [17]. In Nigeria, the prevalence of underweight, overweight and obesity among young adults was 10%, 14.8% and 1.3% respectively [18] while among students in Kumasi Metropolis, the prevalence of underweight, overweight, and obesity was 7.4%, 12.2%, and 0.8%, respectively [19].
In Togo, the prevalence of obesity and overweight in general population according to the STEPS survey in 2010 was respectively 6.2% (2.3% among men and 9.8% among women) and 15.4% (12.0% among men and 18.6% among women) respectively [20]. Some studies were conducted in primary schools in Togo in 2010 [21] and in 2018 [22]. There is a lack of data among young particularly university students who represent a target population for early intervention. A better understanding of risk factors for both under and overnutrition may help in providing better designed health interventions. The objective of this study was to assess the prevalence and factors associated with underweight, overweight and obesity among students of the University of Lomé in 2018.
Methods
Study design
A cross-sectional study was conducted from September to December 2018 in the Department of Preventive Medicine of the University of Lomé (Togo). The University of Lomé is the first public university in Togo and it has been created in 1975. It welcomes students from all regions of Togo as well as foreign students from over 20 countries. Nearly 58,000 students were regularly enrolled at the University of Lomé during the 2018-2019 academic year.
Study population
The study population was composed of students aged 18 and over, regularly enrolled for the current academic year and who had benefited from the routine medical examination at the time of registration. The medical examination is mandatory for first year students and recommended for other students before any registration at the University. Based on previous studies [22], the prevalence of overweight and obesity was 7.1% and with a precision of 1%, the minimum sample size required was estimated at 2,534 students.
This sample size was also adequate for the estimation of the prevalence of underweight among students based on the following assumptions: an expected prevalence of underweight in students of 25% based on the estimates reported in adolescents in sub-Saharan Africa [23] with a precision of 1%, a significance level set at 5%, and a non-response rate of 10%, yielding a minimum sample size of 7,924 students.
Data collection and measure
Data were collected from medical records provided during the medical examinations. Collected data were mainly: anthropometrics (weight and height), clinical (blood pressure) and biological data, socio-demographic characteristics (age, sex), treatment and medical history.
Height was measured without shoes using a stadiometer and weight was measured in light clothing using digital scales. The measurement of height was accurate to 0.1 cm and that of weight was accurate to 0.1 kg.
Blood pressure measurement: Blood pressure was measured using a sphygmomanometer. Blood pressure measurements for each respondent were taken three times with an interval of 5 mins between readings and we used the mean of the three values for each indicator. Respondents whose average systolic blood pressure was ≥ 140 mm Hg or average diastolic blood pressure was ≥ 90 mm Hg and/or were taking anti-hypertensive medication were considered to have high blood pressure.
Blood glucose testing: Random blood glucose (RBS) was measured using a finger-stick blood specimen using the Freestyle Optium H glucometer with glucose test strips.
Screening of forms of malnutrition
The primary outcomes of this study are being obese/overweight or underweight according to the WHO guidelines. These forms of malnutrition were estimated using the body mass index (BMI) defined as the weight in kg divided by the height in meter squared (kg/m²) [2]. According to WHO classification, 4 classes were identified: underweight (BMI<18.5), normal weight (18.5 ≤ BMI < 25), overweight (25 ≤ BMI < 30), and obesity (BMI ≥ 30).
Statistical analysis
Data were entered into an Epidata database in French version 3.1 and exported to R version 3.3.2 for statistical analysis. Quantitative variables were presented as medians with their interquartile range (IQR) and categorical variables were presented as frequencies and percentages. Comparison of medians and proportions was carried out using Wilcoxon’s test and Chi-square independence test or Fisher exact test, respectively. The prevalence (overweight for example) were estimated with corresponding 95% confidence interval (95%CI). Multinomial regression analyzes were performed to identify factors associated with overweight/obesity and underweight. Results were considered statistically significant for a p-value < 0.05.
Ethical consideration
This study was approved by the Department of Research and Innovation (DRI) of the University of Lomé. Survey staff ensured that the anonymity of participants was respected. All persons involved in the data collection have signed a confidentiality agreement and each participant was assigned an unique identification number.
Results
Out of nearly 58,000 students enrolled for the 2018-2019 academic year, 40,561 completed the medical examination. Among them, 37,682 (92.9%) met the inclusion criteria and they were enrolled in the study. There was no statistically difference in terms of age and sex between the students included in the final analysis and those who were not included (p>0.05)
Sociodemographic and clinical characteristics of study participants
Female students represented 32.9% of the study population and the median age was 22 years, (IQR: 20-24) years. Sickle cell disease and asthma were more prevalent in female (p<0.001). These results are presented in Table 1.
| Total (N = 37 682) |
Female Students (N = 25 259) |
Male Students (N = 12 423) |
P-value | |
|---|---|---|---|---|
| Age (years), Median (IQR) | 22 (20-24) | 21 (20-24) | 22 (20-25) | <0.001** |
| Age (years), n (%) | <0.001* | |||
| < 20 | 6233 (16.5) | 2699 (21.7) | 3534 (14.0) | |
| 20-22 | 9643 (25.6) | 3606 (29.1) | 6037 (23.9) | |
| 22-25 | 12691 (33.7) | 3917 (31.5) | 8774 (34.7) | |
| = 25 | 9115 (24.2) | 2201 (17.7) | 6914 (27.4) | |
| History of diseases | ||||
| Sickle cell disease, n (%) | <0.001* | |||
| No | 36891 (97.9) | 11989 (96.5) | 24902 (98.6) | |
| Yes | 791 (2.1) | 434 (3.5) | 357 (1.4) | |
| Asthma, n (%) | <0.001* | |||
| No | 36645 (97.2) | 11934 (96.1) | 24711 (97.8) | |
| Yes | 1037 (2.8) | 489 (3.9) | 548 (2.2) | |
| High Blood Pressure+, n (%) | <0.001* | |||
| No | 34826 (92.4) | 12071 (97.2) | 22755 (90.1) | |
| Yes | 2856 (7.6) | 352 (2.8) | 2504 (9.9) | |
| Blood sugar level, n (%) | 0.801* | |||
| Low† | 8194 (21.7) | 2681 (21.6) | 5513 (21.8) | |
| Normal | 29147 (77.3) | 9626 (77.5) | 19521 (77.3) | |
| High§ | 341 (1.0) | 116 (0.9) | 225 (0.9) | |
| *: Chi square’s test; **: Wilcoxon’s test; IQR: Inter Quartile Range; + Systolic (= 140 mmHg) or diastolic (= 90 mmHg); † : < 0.7 g/l; § : > 1.10 g/l | ||||
Table 1: Socio-demographic and clinical characteristics of students of the University of Lomé according to sex, Togo (N= 37 682).
Prevalence of underweight, overweight and obesity
The overall prevalence of excess weight condition (overweight or obesity) among students was 14.8% (95%CI: 14.4-15.1) and the prevalence of underweight was 8.7% (95%CI: 8.4-8.9). The prevalence of obesity and overweight was 3.4% (95%CI: 3.2-3.6) and 11.4% (95%CI: 11.1-11.7), respectively.
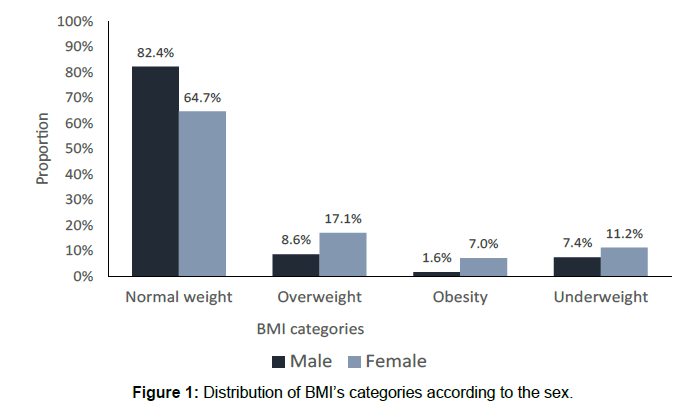
Malnutrition forms were more prevalent among women (p<0.001). As shown in Figure 1, 17.1% of women (vs 8.6% of men) were overweight, 7.0% of women (vs 1.6% of men) were obese, and 11.2% (against 7.4% of men) were underweight.
The percentage of overweight students ranged from 8.7% for students aged less than 20 years, 10.1% for 20-22 years, 11.2% for 22-25 years to 14.9% for over 25 years old. BMI distribution according to age and gender is presented in Table 2.
| Age (years) | Total | Normal weight | Overweight | Obesity | Underweight |
|---|---|---|---|---|---|
| All, n (%) | |||||
| < 20 | 6233 | 4678 (75.1) | 545 (8.7) | 196 (3.1) | 814 (13.1) |
| 20-22 | 9643 | 7436 (77.1) | 975 (10.1) | 280 (2.9) | 952 (9.9) |
| 22-25 | 12691 | 9942 (78.3) | 1425 (11.2) | 387 (3.1) | 937 (7.4) |
| = 25 | 9115 | 6784 (74.4) | 1357 (14.9) | 410 (4.5) | 564 (6.2) |
| Female, n (%) | |||||
| < 20 | 2699 | 1813 (67.2) | 365 (13.5) | 143 (5.3) | 378 (14.0) |
| 20-22 | 3606 | 2361 (65.5) | 564 (5.6) | 219 (6.1) | 462 (12.8) |
| 22-25 | 3917 | 2563 (65.4) | 680 (17.4) | 283 (7.2) | 391 (10.0) |
| = 25 | 2201 | 1299 (59.0) | 509 (23.1) | 229 (10.4) | 164 (7.5) |
| Male, n (%) | |||||
| < 20 | 3534 | 2865 (81.1) | 180 (5.1) | 53 (1.5) | 436 (12.3) |
| 20-22 | 6037 | 5075 (84.1) | 411 (6.8) | 61 (1.0) | 490 (8.1) |
| 22-25 | 8774 | 7379 (84.1) | 745 (8.5) | 104 (1.2) | 546 (6.2) |
| = 25 | 6914 | 5485 (79.3) | 848 (12.3) | 181 (2.6) | 400 (5.8) |
Table 2: Distribution of the BMI according to age and sex.
Factors associated with underweight, overweight and obesity
Multinomial regression analysis which showed factors associated with underweight and overweight/obesity is summarized in Table 3. Students with high blood pressure (aOR= 2.65; 95%CI: 2.40-2.91) and high blood sugar level (aOR= 1.54; 95%CI: 1.18-2.01) were more likely to be overweight or obese. Female students not only (aOR= 3.64; 95%CI: 3.42-3.87) were more likely to be overweight and obese but also underweight (aOR= 1.74; 95%CI: 1.61-1.87). Increasing age was a protective factor for underweight (p<0.05).
| Underweight | Overweight & Obesity | |||||
|---|---|---|---|---|---|---|
| aOR | 95%CI | P-value | aOR | 95%CI | P-value | |
| Age (years) | ||||||
| < 20 | 1 | - | - | 1 | - | - |
| 20-22 | 0.76 | 0.69-0.84 | <0.001 | 1.14 | 1.03-1.26 | 0.009 |
| 22-25 | 0.59 | 0.53-0.65 | <0.001 | 1.33 | 1.21-1.46 | <0.001 |
| = 25 | 0.55 | 0.48-0.61 | <0.001 | 2.07 | 1.88-2.29 | <0.001 |
| Sex | ||||||
| Male | 1 | - | - | 1 | - | - |
| Female | 1.74 | 1.61-1.87 | <0.001 | 3.64 | 3.42-3.87 | <0.001 |
| High Blood Pressure+ | ||||||
| No | 1 | - | - | 1 | - | - |
| Yes | 0.46 | 0.37-0.57 | <0.001 | 2.65 | 2.40-2.91 | <0.001 |
| Blood sugar level | ||||||
| Normal | 1 | - | - | 1 | - | - |
| Low† | 1.07 | 0.98-1.17 | 0.110 | 0.77 | 0.71-0.83 | <0.001 |
| High§ | 0.95 | 0.62-1.45 | 0.808 | 1.54 | 1.18-2.01 | 0.001 |
| # Reference category: Normal weight; aOR: adjusted Odds Ratio; 95%CI: 95% Confidence Interval; + Systolic (= 140 mmHg) or diastolic (= 90mmHg); † : <0.7 g/l; § : >1.10 g/l |
||||||
Table 3: Factors associated with underweight and overweight/obesity among students of the University of Lomé, Togo: Multinomial regression analysis.
Discussion
In this survey among students of the University of Lomé in Togo in 2018, the prevalence of underweight, obesity and overweight was 8.7%, 3.4% and 11.4% respectively. Female sex was associated with both underweight and overweight/obesity. Other factors associated with overweight and obesity were age, high blood pressure and high blood sugar level. Increasing age was a protective factor for underweight.
The prevalence of overweight and obesity in this study was 11.4% and 3.4% respectively. Previous studies conducted among primary school students in Democratic Republic of Congo and in Togo reported lower prevalence of overweight (8.0% and 2.9%, respectively) and obesity (1.0% and 1.7%, respectively) [17,21]. One possible reason for this difference could be the younger age of their study populations compared with participants in the present study. Indeed, there is considerable scientific evidence to support the thesis that overweight increases with age [24–26]. In a systematic review and meta-analysis conducted among children and adolescents in Ethiopia, the separate pooled prevalence of overweight and obesity were 8.92 and 2.39%, respectively [27]. The prevalence of underweight in current study (8.7%) was similar to that reported in South Africa (9.0%; 95%CI: 7.9- 10.2) [28].
Similar study was conducted in Africa among school going adolescents in seven African countries. The prevalence of underweight vary between 12.6% in Egypt to 31.9% in Djibouti. The prevalence of obesity was 0.6% in Benin, 1.0% in Ghana and 3.4% in Mauritania. The prevalence of overweight was 11.2% in Benin, 8.7% in Ghana and 24.3% in Mauritania [29].
Age was associated with overweight and obesity in our study. These results align with those reported in other studies, particularly in Uganda where the prevalence of overweight/obesity was more pronounced after 35 years [30] and Botswana where the prevalence of overweight/obesity among students was significantly associated with age (Odds Ratio [OR]: 1.72, 95% Confidence Interval [CI]: 1.06– 4.46) [31]. While these data support the hypothesis that overweight increases with age, it should also be noted that the trend is the same in all geographical contexts. This could be explained by the fact that the age of majority (18-21 years) often indicates the acquisition of a certain financial autonomy and especially of food choices. Indeed, in childhood, lifestyle and food choices are the responsibility of parents, who can make decisions to protect children’s health [32], but young adults, for societal reasons, very often make choices that are contrary to a healthy lifestyle [33]. There is an interest in targeting this age group in programs to fight against obesity and overweight.
In a multicentric study carried out in seven African countries, there was a tendency for the prevalence of being underweight to rise, starting in the early teens and then decrease between ages 15 and 16 [29].
Being female was associated with overweight and obesity. Many studies have reported similar results. This female predominance observed among obese or overweight people has been described in Senegal (OR=3; p=0.01), China (OR=2.75; p<0.001) and the United States (p=0.004) [34–36]. In addition to the socio-behavioral factors that may be involved, hormonal disturbances should also be considered to explain this female predominance. Studies have shown that women tend to have an increase in appetite and food intake in the second half of the menstrual cycle and during pregnancy, when progesterone levels are higher than usual [37]. Also, some forms of hormone replacement therapy (hormonal’ contraception) can lead to excessive progesterone levels that can increase the risk of insulin resistance, which promotes fat storage rather than its use as an energy source [37]. The initiation of hormone therapy in women should always be evaluated and monitored. We also uncovered in the present study that female students were more likely to be underweight. Our data align with studies conducted in Palestine and Ukraine where underweight was associated with female gender [38,39]. Also, a study carried out in China showed the prevalence of underweight was higher among female students [40]. In contrast, a study conducted among school-going adolescent in seven African countries revealed that males had a higher prevalence of being underweight than females for every country [29].
High blood pressure was associated with overweight and obesity. Studies in various populations around the world have shown the relationship between high BMI and high systolic and diastolic blood pressure [41,42]. One of the mechanisms explaining this link is the secretion by visceral adipose tissue of molecules and hormones such as adiponectin, leptin, resistin, Tumor Necrosis Factor (TNF) and interleukin 6 (IL-6) that exacerbate obesity-related cardiovascular disease [43]. The fight against high blood pressure and other cardiovascular diseases must implicitly induce the fight against obesity and overweight because maintaining a BMI <25 kg/m2 is effective in preventing primary high blood pressure and weight loss leads to a drop in blood pressure in most people with high blood pressure [44,45].
High blood sugar level was significantly associated with overweight and obesity. The link between type 2 diabetes (chronic hyperglycemia) and obesity is well known. Indeed, obese people develop insulin resistance, which is characterized by a reduction of glucose absorption by tissues with the result that blood sugar levels rise [46,47]. This underlines the importance of systematic screening for diabetes and rigorous biological monitoring of obese people.
The originality of this study lies in the size of the sample (N=37,682) and in the fact that it is the first among the student population in Togo. However, there are some limitations to this study. The study design (cross-sectional study) did not establish cause-and-effect relationships (temporality of events difficult to determine) between malnutrition forms and the independent variables studied. Indeed, some factors recognized in the literature as being associated with underweight, overweight, namely alcoholism, smoking, and physical inactivity [48–50], have not been measured because we used data a routine medical visit. Despite these shortcomings, the available data have provided relevant information on underweight, overweight and obesity in student settings in Togo and will help to implement specifics interventions.
Conclusion
The prevalence of both underweight and overweight demonstrated the double burden of malnutrition among students in Lomé. Sociodemographic and health variables risk factors were identified for both underweight and overweight/obesity.
The prevalence of overweight and obesity reported is a reminder that this cardiovascular risk factor is a reality among students at the University of Lomé in Togo, especially female students. Therefore, it is necessary to call for measures targeting this population. This would involve preventing obesity, in particular reducing the consumption of sweets, regular physical activity and awareness-raising actions for a healthy and balanced life. In addition, the management of other comorbidities such as asthma and regular blood pressure monitoring and regular blood glucose testing for diabetes should also be performed. Finally, more epidemiological studies such as this one are needed to have more data and to guide programs to fight the double burden of malnutrition in Togo.
Declaration of competing interest
There are no conflicts of interest to disclose.
Funding
This study was funded by the NGO CARESP, Lomé, Togo, University of Lomé, Togo and the National program for the control of non-communicable diseases of the Ministry of health, Togo.
Authors’ contribution
DKE, MB and FAGK conceived this study and participated in its design and coordination. EA and KNT, WICZC, AS and RYK participated in the study design and data collection. MKT and EKS performed statistical analyses. WICZC, AS and RYK wrote the first draft of the manuscript and FAGK, DKE, MB, EKS, MKT, EA and KNT subsequently revised the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank the national program for the control of non-communicable diseases of Togo, the staff of African Center for Research in Epidemiology and Public Health and its coordinator, and the Department of Preventive Medicine of the University of Lomé. We would also like to thank the students for their collaboration.
References
- NCD Risk Factor Collaboration (2016) Trends in adult body-mass index in 200 countries from 1975 to 2014: a pooled analysis of 1698 population-based measurement studies with 19·2 million participants. The Lancet 387: 1377-1396.
- Delisle H. Obesity is a problem for the wealthy in developing countries. In: Misconceptions in global health. Montreal: University of Montreal Press, pp: 165-168.
- Onyango AW, Jean-Baptiste J, Samburu B, Mahlangu TLM (2019) Regional Overview on the Double Burden of Malnutrition and Examples of Program and Policy Responses: African Region. Ann Nutr Metab 2019; 75: 127–130.
- Correia J, Pataky Z, Golay A (2014) Comprendre l’obésité en Afrique. Rev Med Suisse 10: 712–716.
- Sondji SH (2017) State of obesity in sub-Saharan Africa. Annales Africaines de Médecine; 11: e2753-e2754.
- Wesenbeeck CFA van (2018) Distinguish between urban and rural food security in West Africa. OECD Publishing.
- World Health Organization (2017) Nutrition in the WHO African Region. Brazzaville: WHO Regional Office for Africa.
- Akombi BJ, Agho KE, Merom D, Renzaho AM, Hall JJ (2017) Child malnutrition in sub-Saharan Africa: A meta-analysis of demographic and health surveys (2006-2016). Plos One 12: e0177338.
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity: An evaluation of potential bias. Vital Health Stat 3: 1-21.
- Mandengue SH, Bita AF, Epacka ME, Tamba SM, Kollo B. (2015) Epidemiology of obesity among university students in Douala, Cameroon. Med Sante Trop 25: 386-390.
- Kouakou AYF, Kamagate A, Yapo AP (2017) Prévalence de l’obésité en milieu jeune en Côte d’Ivoire. European Scientific Journal 2017; 13: 241.
- Musung JM, Muyumba EK, Nkulu DN, Kakoma PK, Mukuku O, et al. (2019) Prevalence of overweight and obesity among adolescents in schools in Lubumbashi, Democratic Republic of Congo.Pan Afr Med J 32: 49.
- Ogunlade O, Asafa MA.(2015) Pattern and prevalence of underweight, overweight and obesity among young adult Nigerians. Am J Biomed Life Sci 3: 12–15.
- Kumah DB, Akuffo KO, Abaka-Cann JE, Affram DE, Osae Ae (2015) Prevalence of overweight and obesity among students in the Kumasi metropolis. Journal of Nutrition and Metabolism. 2015.
- Agoudavi K, Adjoh KS, Afanvi K (2010) Final report of the investigation TOGO 2010. Togo: Ministry of Health, 2012.
- Djadou KE, Sadzo-Hetsu K, Koffi KS, Tsolenyanu E, Douti K, et al. (2010) Prevalence of obesity in urban scolar area (Togo). Journal de Pédiatrie et de Puériculture 23: 335-339.
- Sagbo H, Ekouevi DK, Ranjandriarison DT, Niangoran S, Bakai TA, et al. (2018) Prevalence and factors associated with overweight and obesity among children from primary schools in urban areas of Lomé, Togo. Public Health Nutrition 21: 1048-1056.
- Christian P, Smith ER (2018) Adolescent undernutrition: global burden, physiology, and nutritional risks. ANM 72: 316-328.
- Matta J, Czernichow S, Goldberg M, Ozguler A, Goldberg M, et al. (2016) Prevalence of overweight, obesity and cardio-metabolic risk factors in the Constances cohort. Bull Epidemiol Hebd 35: 640-646
- El-Hazmi M, Warsy A (2002) Relationship between age and the prevalence of obesity and overweight in Saudi population. Bahrain Medical Bulletin 24: 1-7.
- Gebrie A, Alebel A, Zegeye A (2018) Prevalence and associated factors of overweight/ obesity among children and adolescents in Ethiopia: A systematic review and meta-analysis. BMC Obesity 5: 19.
- Reddy SP, Resnicow K, James S, Kambaran N, Omardien R, et al. (2009) Underweight, overweight and obesity among South African adolescents: results of the 2002 National Youth Risk Behavior Survey. Public Health Nutrition 2009; 12: 203–207.
- Manyanga T, El-Sayed H, Doku DT, Randall JR (2014) The prevalence of underweight, overweight, obesity and associated risk factors among school-going adolescents in seven African countries. BMC Pub Health 14: 887.
- Kirunda BE, Fadnes LT, Wamani H, den Broeck JV, Tylleskar T (2015) Population-based survey of overweight and obesity and the associated factors in peri-urban and rural Eastern Uganda. BMC Pub Health 15: 1168.
- Tapera R, Merapelo MT, Tumoyagae T, Maswabi TM, Erick P, et al. Â (2017) The prevalence and factors associated with overweight and obesity among University of Botswana students. Cogent Medicine 4: 1357249.
- World Health Organization (2016) Consideration of the evidence on childhood obesity for the Commission on Ending Childhood Obesity: Report of the ad hoc working group on science and evidence for ending childhood obesity, Geneva, Switzerland.
- Timotijevic L, Acuna-Rivera M, Gemen R, Kugelberg S, McBarron K, et al. (2018) Adolescents’ perspectives on personal and societal responsibility for childhood obesity. The study of beliefs through ‘serious’ game (PlayDecide). Children & Society 32: 405-416.
- Ndiaye P, Leye MMM, Dia AT (2016) Overweight, obesity and associated factors among students of the 2 nd public education cycle Dakar. Sante Publique 28: 687-694.
- Hu L, Huang X, You C, Li J, Hong K, et al. (2017) Prevalence of overweight, obesity, abdominal obesity and obesity-related risk factors in southern China. Plos One 12: e0183934.
- Flegal KM, Carroll MD, Ogden CL, Curtin LR (2010) Prevalence and trends in obesity among US adults, 1999-2008. JAMA 303: 235-241.
- Al-Lahham S, Jaradat N, Altamimi M, Anabtawi O, Irshid A, et al. (2019) Prevalence of underweight, overweight and obesity among Palestinian school-age children and the associated risk factors: A cross sectional study. BMC Pediatr 19: 483.
- DereÅ„ K, Nyankovskyy S, Nyankovska O, Åuszczki E, WyszyÅ„ska J, et al. (2018) The prevalence of underweight, overweight and obesity in children and adolescents from Ukraine. Sci Rep 2018; 8: 1-7.
- Ren X, Chen Y, He L, Jin Y, Tian L, et al. (2015) Prevalence of underweight, overweight and obesity in university students from the region of Anhui (China). Nutr Hosp 2015; 31: 1089-1093.
- Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME (2015) Obesity-Induced Hypertension. Circulation Research 2015; 116: 991-1006.
- Aronow WS, Fleg JL, Pepine CJ (2011) Hypertension in the Elderly. J Am Coll Cardiol 57: 2037-2114.
- DeMarco VG, Aroor AR, Sowers JR (2014) The pathophysiology of hypertension in patients with obesity. Nat Rev Endocrinol 10: 364–376.
- Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, et al. (2001) Long-term weight loss and changes in blood pressure: Results of the trials of hypertension prevention, phase II. Ann Intern Med 134: 1-11.
- Jones DW, Miller ME, Wofford MR, Anderson DC Jr, Cameron ME, et al. (1999) The effect of weight loss intervention on antihypertensive medication requirements in the hypertension optimal treatment (HOT) study. Am J Hypertens 1999; 12: 1175-1180.
- Hribal ML, Oriente F, Accili D (2002) Mouse models of insulin resistance. American Journal of Physiology-Endocrinology and Metabolism 282: E977-E981.
- Saltiel AR, Kahn CR (2001) Insulin signalling and the regulation of glucose and lipid metabolism. Nature 414: 799-806.
- Grucza RA, Krueger RF, Racette SB, Norberg KE, Hipp PR, et al. (2010) The Emerging link between alcoholism risk and obesity in the United States. Arch Gen Psychiatry 67: 1301-1308.
- Clair C, Berlin I, Cornuz J (2011) Smoking, obesity and diabetes: a clinically important interaction. Revue Médicale Suisse 7: 2338-2342.
- Berthouze-Aranda SE, Reynes E (2011) Sedentary lifestyle: a physio-psychological process and an health risk factor for everyone. Science & Sports 26: 191-196.
Citation: Zida-Compaore WIC, Gbeasor-Komlanvi FA, Tchankoni MK, Sadio A, Konu YR, et al. (2020) Prevalence and Factors Associated with Underweight, Overweight and Obesity among Students of the University of Lomé, Togo In 2018. J Obes Weight Loss Ther 10: 398. DOI: 10.4172/2165-7904.1000398
Copyright: © 2020 Zida-Compaore WIC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2241
- [From(publication date): 0-2020 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 1485
- PDF downloads: 756