Prevalence and Factors Associated with Pressure Ulcer among Patients Admitted in Hawassa University Referral Hospital, South Ethiopia
Received: 24-May-2018 / Accepted Date: 12-Jul-2018 / Published Date: 19-Jul-2018
Keywords: Prevalence of pressure ulcer; Decubitus ulcer; Bed sore; Nursing care; Standard nursing care; Length of stay
Introduction
Pressure ulcers affect millions of people worldwide and nearly always occur over bony areas of the body where pressure and tissue distortion is greatest. Pressure ulcer is defined as a localized injury to the skin and/or underlying tissue usually over a boney prominence, as a result of pressure or pressure in combination with shear and/or friction (European Pressure Ulcer Advisory Panel (EPUAP)). Pressure applied to the skin over time determines the occurrence of pressure ulcers. Patients who have a lower capillary closure pressure are at greater risk for pressure ulcers [1]. Presence of pressure ulcer is considered as a measure of quality of nursing care provided by health care institutions [2].
It is largely preventable patient safety problem, recognized globally as one of the five most causes of harm to patients [3]. Patients with medical conditions that limit their ability to change position, those who requires wheel chair and those who confines to bed for a long time are at risk of pressure ulcers [4-8].
Patients confined to bed for long periods, patients with motor or sensory dysfunction, and patients who experience muscular atrophy and reduction of padding between the overlying skin and the underlying bone are prone to pressure ulcers [1].
The initial sign of pressure is erythema (redness of the skin) caused by reactive hyperemia, which normally resolves in less than 1 hour. Unrelieved pressure results in tissue ischemia or anoxia. The cutaneous tissues become broken or destroyed, leading to progressive destruction and necrosis of underlying soft tissue, and the resulting pressure ulcer is painful and slow to heal [1]. Once pressure ulcer is developed, proper wound care, and proper nutrition (protein) are indicated to facilitate healing process.
Pressure ulcers are serious health issue in health care settings. Common both in acute and chronic care facilities and impose a significant burden on patients, their relatives and care givers [9]. The pain and discomfort due to pressure ulcer leads to costly and physically debilitating complications which prolongs; duration of illness, time of discharge, and even contribute to disability and death. They are also described as an indicator of quality of care provided by health care organization [10].
Globally, exact magnitude of pressure ulcer varies with the type of illness and among specific clinical populations. Pressure ulcers remain a major health problem affecting approximately 3 million adults [11]. The magnitude is high (15 - 30%) in person with chronic spinal cord injury and is the second cause of re-hospitalization next to spinal cord injury [12]. The sacrum or coccyx areas and the heels are the most common sites (account 50%) for the development of pressure ulcers [2].
Pressure ulcer is expected to be more in developing countries due to inadequate pressure relieving devices, low commitment of nursing staff, and low level of awareness on prevention mechanisms. In Africa, the magnitude of pressure ulcers varies within a country and among countries. In south west Nigeria, the prevalence was between 0 to 6.9% and it is slightly more in male than females [2]. In northern Ethiopia, the identified prevalence of pressure ulcers so far was 16.8% and it affected males more than females [13].
Numerous studies in developed world identified that prolonged pressure, friction at the skin surface, loss of sensory perception and immobility are the main risk factors for the occurrence of pressure ulcers [14-17].
Another study revealed that Hypoalbuminemia, incontinence, and fractures are significantly associated to pressure sore [18]. More recent research has suggested that moisture and temperature may also contribute to occurrence of pressure Ulcer [19].
Pressure ulcers can be prevented by changing patient’s position every two hours, providing effective skin care and using pressure relieving mattress [11]. Use of Braden scale pressure ulcer risk assessment tool can also be used to prevent the development of pressure ulcer as the tool is important to identify those at risk and not at risk and to prepare ahead to provide quality and appropriate care based on risk analysis and level of severity [20].
According to one study conducted in Addis Ababa public hospitals, almost all nurses have adequate knowledge about pressure ulcer [21]. In study conducted at University of Gondar referral hospital, about 85% of nurses have knowledge. The study also concluded that, there was no refreshment or on the job training provided yet on pressure ulcer and no hospital specific guideline regarding pressure ulcers prevention [22]. It is unquestionable that quality care at health institutions is important to prevent pressure ulcer and related problems. For this to happen, health institutions are better have standard pressure ulcer prevention mechanisms. Despite the fact, there is limited evidence and insufficient published data about the magnitude of pressure ulcer in Ethiopia in general and in Hawassa in particular. Therefore, the aim of this study was to assess prevalence and factors associated with pressure ulcers among patients admitted in selected wards and care units of Hawassa University referral hospital.
The results of this study are of great importance as it may assist health professionals in preventing pressure ulcer as it is highly preventable suffering to the bedridden patients.
Method and Materials
Study design and period
Health institution based cross sectional study was conducted in April, 2016.
Study area
The study was conducted in Hawassa University referral hospital. The hospital was established in 2004 by collaboration of federal ministry of health, regional government and health bureau and Hawassa town community. The hospital is found in south western part of Hawassa town and is bordered to the east by Hawassa town, to the north by Tabor Mountain, to the west by Hawassa Lake and to the south by private local residents.
It provides diversity of both outpatient and inpatient services for about 15 million people from all over southern regional states (SNNPR) and neighboring Oromia region. Currently, it has 350 beds and provides patient care in a broad range of services to over 90, 200 outpatient, 18,116 hospitalized patients and 1,092 emergency cases annually. It offers services at general and specialty levels. The hospital has an average monthly admission of 572 patients in Intensive care unit and wards (Gyne/Obs, Surgical, Medical and Orthopedic). There is a chance for those admitted patients to develop pressure ulcers since the hospital provide diversity of care for acute and chronic illness.
Sample size determination
Sample size was determined by using single population proportion formula with 95% confidence interval, 5% margin of error and adding 5% for non-respondent rate. By using the proportion of pressure ulcer 16.8 %, obtained from previous cross sectional study conducted with sample size of 422 patients in Felegehiwot referral hospital, northern Ethiopia [13], the sample size was calculated as follow.
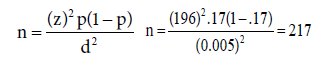
Therefore by adding 5 % for possible non response, the final sample size was =228.
Sampling technique
Average 572 patients admitted in four wards and adult intensive care unit of Hawassa University referral hospital (HURH) monthly of which 153, 171, 180, 30 and 38 admitted to medical ward, surgical ward, Gyn/ Obs ward, orthopedic ward, and adult intensive care unit respectively. Distribution of the calculated total sample to each selected wards is proportional to their monthly admission history with 61 samples from Medical ward, 68 from surgical ward, 72 from Gyne/Obs ward, 12 from orthopedic ward and 15 from adult intensive care unit. Then the study unit was selected based on bed number using systematic random sampling technique with K–value of 3 from each ward. Accordingly to begin interview, the first study unit was taken by lottery method.
Exclusion criteria
Patients with accidental injury on bony prominent areas.
Patients who are not willing to participate and critically sick during data collection time.
Data collection and analysis procedure
Data collection instruments: Data collection tool was adopted from previous studies [13] and also developed by investigators. The final approved tool were translated to local language (Amharic) with back translation to English for consistency and it was pretested prior to the actual data collection among 5% of the actual sample size at Adare, a nearby government hospital. Braden scale pressure sore risk assessment (a standard tool used to assess level of risk of pressure ulcer development among hospitalized patient) was also included in the data collection tool. Braden scale (6 items; total scores range from 6 to 23) include items related to activity, mobility, nutritional status, incontinence and cognition (12).
Data collection procedures: Data was collected by face to face interview using a structured and pretested questionnaires, prepared check lists and physical examination. Trained diploma nurses with previous data collection experience have collected the data. Before starting data collection, the data collectors hold detail discussion on each question to assure consistency and have the same level of understanding on how to collect and keep the quality of data. One data collector per selected ward of Hawassa University referral hospital was considered for data collection. Data collection process was conducted during working day and weekend time at bed sides. An average time spent to complete one questionnaire per patient was 15-20 minutes.
Data quality control measures: Questioners were pretested prior to the actual data collection and corrections and adaption of the tool was made including addition of certain important questions. The pretest was conducted in Adare general hospital located in Hawassa Ethiopia. The reliability test was checked by chrombach α and it was found to be 0.71. Data collectors and supervisor were trained on data collection process and procedures for half day. Filled questionnaires were checked on daily bases for completeness, clarity and accuracy. Data cleaning was undertaken before entry and analysis.
Data analysis: Data was coded and entered into Epi data version 3.1 and exported to SPSS version 20 statistical software for analysis. Descriptive statistics was made using frequency tables, graphs, pie chart and other narrative explanations. Association between dependent and independent variables were examined by using appropriate statistical tests such as 95% CI, Odds Ratio (OR), P-value with bivariate logistic regression. All variables which had p<0.25 during bivariate logistic regression, were made candidate for multivariate logistic regression. The relative contribution of each selected independent variable with the dependent variable was assessed by using multivariate logistic regressions.
Operational definitions
Pressure ulcer: a lesion of skin or underlying tissues by direct unrelieved pressure for more than 3 h on the skin.
Knowledge: Based on total score, knowledge level on pressure ulcer was categorized as good and poor knowledge. Higher points above or equal to mean score indicate good knowledge and points less than mean score indicate poor knowledge.
Ethical consideration
Ethical approval was obtained from Hawassa University College of medicine and health science Institutional Review Board. Permission was taken from Hawassa University referral hospital. All study participants were informed about the purpose of the study and verbal consent as well as written consent was sought from each patient prior to the beginning of data collection. Respondents had given the right to refuse participation and even terminate their involvement at any point during the study time. Nursing care was given for those patients who have developed pressure ulcer during study period.
Results
Socio demographic characteristics
Two hundred and twenty eight patients were surveyed, 53.9% were rural residents and 46.1% urban. 39.5% were Protestants and majorities (68%) were married. Female participants account more than half (56.6%) and 46.9% of respondents were found in the age range of 15-34 years. The mean age of the respondents were 37.02±15.2 year. Regarding the educational status, 15% of respondents were illiterate and 20.6% of study participants had educational level of grade 10 and above. (See Table 1 for detail on Socio-demographic characteristics of respondents).
| Variables | Frequency | % | |
|---|---|---|---|
| Sex | Male | 99 | 43.4 |
| Female | 129 | 56.6 | |
| Age | 15-34 | 107 | 46.9 |
| 35-54 | 82 | 36 | |
| ≥55 | 39 | 17.1 | |
| Residence | Urban | 106 | 46.5 |
| Rural | 122 | 53.5 | |
| Marital status | Single | 55 | 24.1 |
| Married | 155 | 68.0 | |
| Divorced | 7 | 3.1 | |
| Widowed | 11 | 4.8 | |
| Religion | Orthodox | 66 | 28.9 |
| Muslim | 66 | 28.5 | |
| Protestant | 90 | 39.9 | |
| Others | 6 | 2.7 | |
| Educational status | Illiterate | 34 | 14.9 |
| Read and write | 35 | 15.4 | |
| Grade 1-4 | 33 | 14.5 | |
| Grade 5-8 | 34 | 14.9 | |
| Grade 9-10 | 45 | 19.7 | |
| Grade 10 and above | 47 | 20.6 | |
*Others: (Catholic, Only Jesus, Jova witness)
Table 1: Socio demographic characteristics of respondents who were admitted to Hawassa University Referral Hospital, Hawassa, Ethiopia 2016 (n=228).
Prevalence of pressure ulcer
Pressure ulcer by anatomical location, age and educational status: Among study participants, 19(8.3%) developed pressure ulcer.
The major anatomical site observed with ulcer was sacral area (53%). Among the respondents who developed pressure ulcer, 45% were over 54 years and 20% were within the age range of 45 to 54 years (Figure 1).
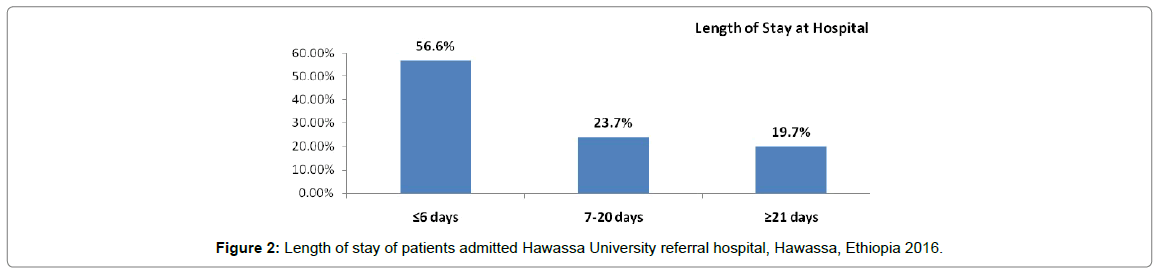
Pressure sore by Length of Stay and pressure relieving devices: According to this study, more than half (56.4%) of admitted patients in Hawassa referral hospital stayed ≤6 days and about 20% stayed for three weeks and more. Among patients who had hospital stay of more than 20 days after admission, 20% had developed ulcer. But, it was rare among patients who had hospital stay of ≤6 days (6.2%) and 7-20 days (3.7%) after admission. All individuals who developed pressure ulcer didn’t use pressure relieving device. There was even no pressure relieving devices in any included wards of Hawassa University referral hospital (Figure 2).
Pressure sore by frequency of Position change: Of the respondents, 21.5% changed their position from 2 to 4 times a day and 11.4% changed their position less than 4 times a day. The rest 35.5% changed their position every 2 hours and 31.6% changed their position every 4 hours. The magnitude of pressure ulcer was maximum (19.2%) among patients who turned their position less than 4 times a day and minimum (4.9%) among patients who changed their position every 2 hours. Of the respondents who developed pressure ulcer, 19% changed their position by the assistance of their relatives and 30.8% changed their position by the assistance of nurses (Table 2).
| Characteristics | Pressure sore | ||
|---|---|---|---|
| N | % | ||
| Frequency of Position change | Every 2 hours | 4 | 4.9 |
| Every 4 hours | 4 | 5.6 | |
| 2-4 times per day | 6 | 12.2 | |
| Less than 4 times per day | 5 | 19.2 | |
| Means of changing position | Self | 0 | 0 |
| Relative | 15 | 19.2 | |
| Nurse | 4 | 30.8 | |
Table 2: Frequency in position change among respondents who developed pressure ulcer at Hawassa University referral hospital, Hawassa, Ethiopia 2016.
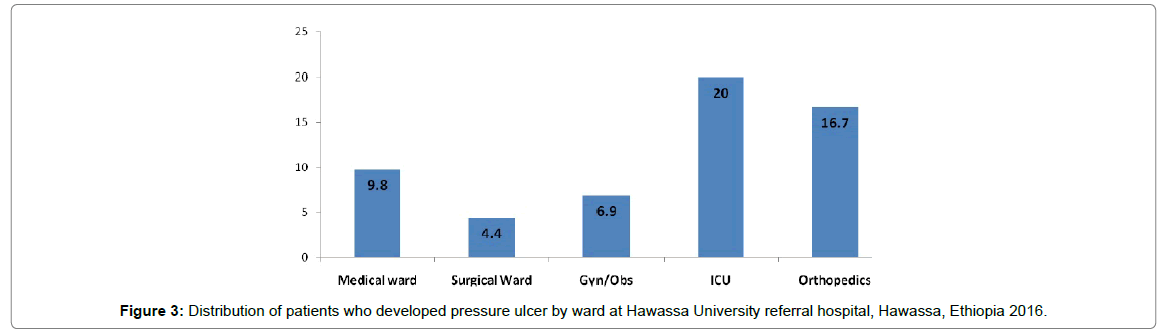
Pressure sore by department or wards: Patients from five selected wards of the hospital were included in the study with proportional distribution of total sample; medical ward (61), surgical ward (67), Gynecology ward (72), intensive care Unit (15) and orthopedics (13). Regarding pressure ulcer distribution among study participants in each ward, 4.4% were from surgical ward patients and 20% were from intensive care unit patients (detail shown in Figure 3) On the other hand prevalence of pressure ulcer as compared to each department was maximum in medical ward (31.6%), followed by Gyne/Obs ward (26.3%), surgical ward (15.8%), intensive care Unit (15.8%) and orthopedic ward (10.5%).
Braden scale pressure sore risk assessment: From the total respondents, around half (46.9%) had no impairment in their sensory perception and 33.3% had reported slightly limitation in their sensory perception. About 43% of the respondents had reported occasional moisture and only 14.9% of the respondents faced constant moisture. Some (11.8%) of the participants reported very poor in nutrition which was much less compared with probably inadequate (51.3%) and adequate (36.8%) nutrition (Table 3).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Sensory perception | Completely limited | 21 | 9.2 |
| Very Limited | 24 | 10.5 | |
| Slightly Limited | 76 | 33.3 | |
| No impairment | 107 | 46.9 | |
| Moisture | Constantly moist | 34 | 14.9 |
| Very moist | 17 | 7.5 | |
| Occasionally moist | 98 | 43.0 | |
| Rarely Moist | 79 | 34.6 | |
| Activity | Bedfast | 46 | 20.2 |
| Chair fast | 27 | 11.8 | |
| Walks occasionally | 90 | 39.5 | |
| Walks frequently | 65 | 28.5 | |
| Mobility | Completely immobile | 30 | 13.2 |
| Very Limited | 24 | 10.5 | |
| Slightly Limited | 98 | 43 | |
| No limitation | 76 | 33.3 | |
| Nutrition | Very poor | 27 | 11.8 |
| Probably inadequate | 117 | 51.3 | |
| Adequate | 84 | 36.8 | |
| Friction or shear | Problem | 22 | 9.6 |
| Potential problem | 95 | 41.7 | |
| No apparent problem | 111 | 48.7 | |
Table 3: Braden scale pressure sore risk assessment characteristics in Hawassa University Referral Hospital, Hawassa, Ethiopia 2016.
Factors associated with pressure sore
Independent variables were analyzed against one dependent variable (pressure ulcer) to assess if there is an association. Primarily, one independent variable with one dependent variable was checked to select the independent variables that were candidate for multivariate logistic regression. Then, those independent variables that had p<0.25 were made a candidate for multivariate logistic regression. After running multivariate logistic regression, we identified as length of stay in the hospital after admission had associated with the development of pressure ulcer. Those participants who have stayed in the hospital for ≥21 days had more than 6 times 6.27 (95% CI: 1.07, 36.76) at increased risk of developing pressure ulcer compared to those who had length of stay of ≤6 days after admission (Table 4).
| Variables | Pressure ulcer | Crude OR(95%CI) | Adjusted OR (95%) | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| N (%) | N (%) | ||||
| Age | 15-34 year | 5(4.7) | 102(95.3) | 1 | 1 |
| 35-54 year | 5(6.1) | 77(93.9) | 1.33(0.37-4.74) | 0.99(0.16-6.36) | |
| > 54 year | 9(23.1) | 30(76.9) | 6.12(1.91-19.65)* | 1.79(0.24-13.14) | |
| Sex | Male | 11(11.1) | 88(88.9) | 1.89(0.73-4.90) | 1.55(0.30-8.00) |
| Female | 8(6.2) | 121(93.8) | 1 | 1 | |
| Educational status | Illiterate | 5(14.7) | 29(85.3) | 3.88(0.71-21.34) | 4.01(0.30-52.89) |
| Read and write | 4(11.4) | 31(88.6) | 2.90(0.50-16.84) | 2.53(0.19-33.90) | |
| Grade 1-4 | 2(6.1) | 31(93.9)) | 1.45(0.19-10.86) | 1.33(0.09-19.19) | |
| Grade 5-8 | 3(8.8) | 31(91.2) | 2.18(0.34-13.80) | 1.67(0.15-19.12) | |
| Grade 9-10 | 3(6.7) | 42(93.3) | 1.61(0.26-10.10) | 1.71(0.14-20.67) | |
| Greater than grade 10 | 2(4.3) | 45(95.7) | 1 | 1 | |
| Position change | Every 2 hours | 4(4.9) | 77(95.1) | 1 | 1 |
| Every 4 hours | 4(5.6) | 68(94.4) | 1.13(0.27-4.70) | 0.40(0.04-4.18) | |
| 2-4 times per day | 6(12.2) | 43(87.8) | 2.69(0.72-10.05) | 0.71(0.08-6.26) | |
| Less than 4 times per day | 5(19.2) | 21(80.8) | 4.58(1.13-18.60)* | 0.84(0.11-6.31) | |
| Length of stay in hospital | ≤6 days | 8(6.2) | 121(93.8) | 1 | 1 |
| 7-20 days | 2(3.7) | 52(96.3) | 0.58(0.12-2.83) | 0.19(0.02-1.75) | |
| ≥21 days | 9(20) | 36(80) | 3.78(1.36-10.51)* | 6.27(1.07-36.76)* | |
| Sensory perception | Completely limited | 5(23.8) | 16(76.2) | 5.26(1.43-19.28)* | 3.03(0.33-27.90) |
| Very limited | 4(16.7) | 20983.3) | 3.37(0.87-13.03) | 1.45(0.15-14.08) | |
| Slightly limited | 4(5.3) | 72(94.7) | 0.94(0.26-3.43) | 0.36(0.04-3.20) | |
| No impairment | 6(5.6) | 101(94.7) | 1 | 1 | |
| Activity | Bedfast | 9(19.6) | 37(80.4) | 7.66(1.57-37.39)* | 2.72(0.21-35.32) |
| Chair fast | 4(14.8) | 23(85.2) | 5.48(0.94-31.95) | 2.42(0.21-27.81) | |
| Walks occasionally | 4(4.8) | 86(95.6) | 1.47(0.26-8.25) | 0.67(0.07-6.70) | |
| Walks frequently | 2(3.1) | 63(96.9) | 1 | 1 | |
| Mobility | Completely immobile | 3(10) | 27(90) | 2.00(0.42-9.53)) | 0.06(0.003-1.49) |
| Very limited | 5(20.8) | 19(79.2) | 4.74(1.16-19.38)* | 1.41(0.12-16.31) | |
| Slightly limited | 7(7.1) | 91(92.9) | 1.39(0.39-4.92) | 1.24(0.17-9.04) | |
| No limitation | 4(5.3) | 72(94.7) | 1 | 1 | |
| Nutrition | Very poor | 5(18.5) | 22(81.5) | 4.55(1.12-18.38)* | 2.27(0.23-22.71) |
| Probably inadequate | 10(8.5) | 107(91.5)) | 1.87(0.57-6.18) | 1.30(0.18-9.37) | |
| Adequate | 4(4.8) | 80(95.2) | 1 | 1 | |
| Friction and shear | Problem | 4(18.2) | 18(81.8) | 2.52(0.70-9.06) | 1.11(0.12-9.92) |
| Potential problem | 6(6.3) | 89(93.7) | 0.76(0.26-2.23) | 0.51(0.09-2.77) | |
| No problem | 9(8.1) | 102(91.9) | 1 | 1 | |
| Moisture | Constantly moist | 8(23.5) | 26(76.5) | 5.77(1.60-20.76)** | 5.49(0.54-56.19) |
| Very moist | 4(23.5) | 13(76.5) | 5.77(1.28-26.01)* | 5.29(0.57-49.34) | |
| Occasionally moist | 3(3.1) | 95(96.9) | 0.59(0.13-2.73) | 0.28(0.03-2.43) | |
| Rarely moist | 4(5.10 | 75(94.9) | 1 | 1 | |
| Knowledge | Good knowledge | 2(3.1) | 62(96.9) | 0.28(0.06-1.24) | 1.91(0.31-11.91) |
| Poor knowledge | 17(104) | 147(89.6) | 1 | 1 | |
| Note: • Model classification accuracy is = 91.7 , *P<0.05, ** p<0.01 and *** p<0.001 • The categorical reference is selected based on scientifically meaningful manner |
|||||
Table 4: Association between some selected independent variables and pressure ulcer at Hawassa University referral hospital, Hawassa, Ethiopia, 2016.
Discussion
Both the magnitude and associated factors of pressure ulcers among admitted patients in Medical, surgical, Gyne/Obs, orthopedics and adult intensive care unit of Hawassa University referral hospital were assessed. The overall prevalence of pressure ulcer was 8.3%. The result was higher than cross sectional study conducted in China, 1.58% [23]. This might be due to difference in quality of care provided, difference in socioeconomic characteristics, access to pressure relieving devices and use of standard pressure ulcers prevention protocols. Use of pressure relieving device in prevention or minimizing risk of pressure ulcer development by 76.9% among hospitalized patients was supported by findings from previous study conducted in England [24].
The finding of this study is slightly lower than the previous cross sectional study conducted in Ethiopia (16.8%) [13] and Norway (18.2%) [25]. It is also lower than previous prospective cohort study conducted in Switzerland (14.2%) [26]. This difference generally might be due to diversity of the study participant’s culture, disease condition of patients, difference in study design and also the variation of length of stay in hospital. This study employed cross sectional study design with no follow up and the sample size is minimal which was lower than sample used in the majority of a fore mentioned previous studies.
In this study, presence of pressure ulcer was significantly associated with increased length of stay in the hospital 6.27 (95% CI: 1.07, 36.76). The likely hood of developing pressure ulcer is around six (6) times more risk among patients who stayed ≥21 days in hospital than those stayed ≤6 days after admission in hospital. This finding was in line with previous prospective cohort study conducted in England [27] and population based retrospective cohort study conducted in Taiwan [28]. This could best explained as, increased length of stay in hospital might lead to prolonged pressure which in turn decreased blood circulation in particular area. More over increased patients stay in hospital for long period of time might expose individuals for hospital acquired infections and this in turn may raise vulnerability to the development of pressure ulcer. Another possible reason for the association between length of stay in hospital and occurrence of pressure ulcer was that patients may not get appropriate nursing care. Development of pressure ulcer among hospitalized patients is performance indicator of quality of nursing care which may reduce with increased length of stay in hospital.
Limitation Of The Study
From the recommendation of various studies, Cohort or follow up study design is more preferable for the study of pressure ulcer.
Conclusion and Recommendation
The overall prevalence of pressure ulcer was 8.3% among hospitalized patients. Prolonged length of stay more than twenty days in hospital was significantly associated with the presence of pressure ulcer. Use of Braden scale pressure ulcer risk assessment tool for early action and prevention of pressure ulcer and work to minimize length of stay of admitted patients in hospitals is needed.
Practice of appropriate nursing care standard and application of pressure relieving devices in hospital wards is believed to minimize risk of developing pressure ulcer and related complications. As presence of pressure ulcer indicates quality of care, health institutions should design on the job refresher trainings for nurses on pressure ulcer facts including prevention.
Further follow up study involving different institutions and high sample is required to investigate the incidence and associated factors of pressure ulcer for hospitalized patients.
Authors’ contribution
TF, JE, WJ and BD designed the study, developed proposal, collected data, participated on data analysis and report writing and participated on manuscript preparation. WJ and BD assisted in study design and proposal development, participated on data collection, analysis and report writing. WJ designed and prepared manuscript. All the authors revised and approved the final manuscript.
Acknowledgment
We would like to thank Hawassa University referral hospital and school of nursing and midwifery for material support. The authors are also grateful to supervisors, and data collectors who showed the greatest effort in acquiring appropriate information. Finally, we would like to extend heartfelt thanks to the study subjects who have kindly cooperated in providing the required information.
Conflict Of Interest
The authors declare that they have no conflict of interests.
Source of funding
No specific grant from any funding agency in the public, commercial or not for profit organization had received for this research.
References
- Suzzane C, Smeltzer BGB, Janice l. Hinkle, Kerry H. Cheever. 2012. Brunner and suddarth’s text book of medical-surgical nursing. 12th ed, london.
- Adegoke BOA, Odole AC, Akindele LO, Akinpelu AO (2013) Pressure ulcer prevalence among hospitalised adults in university hospitals in south-west nigeria. Wound practice and research 21: 128-134.
- Robinson M (2005) Australian council on healthcare standards. Primary Intention 13: 104-117.
- European pressure ulcer advisory panel and national pressure ulcer advisory panel 2014. Treatment of pressure ulcers: quick reference guide.
- Barrois B, Labalette C, Rousseau P, Corbin A, Colin D, et al. (2008) A national prevalence study of pressure ulcers in french hospital inpatients. J Wound Care 17: 373-376.
- Baumgarten M, Margolis D, Gruber-Baldini AL, Zimmerman S, German P, et al. (2003) Pressure ulcers and the transition to long-term care. Adv Skin Wound Care 16: 299-304.
- Capon A, Pavoni N, Mastromattei A, Di Lallo D (2007) Pressure ulcer risk in long-term units: prevalence and associated factors. J Adv Nurs 58: 263-272.
- Chacon JM, Blanes L, Hochman B, Ferreira LM (2009) Prevalence of pressure ulcers among the elderly living in long-stay institutions in São Paulo. Sao Paulo Med J 127: 211-215.
- Bours GJ, Halfens RJ, Candel MJ, Grol RT, Abu-Saad HH (2004) A pressure ulcer audit and feedback project across multi-hospital settings in the netherlands. Int J Qual Health Care 16: 211-218.
- Fogerty M, Guy J, Barbul A, Nanney LB, Abumrad NN (2009) African Americans show increased risk for pressure ulcers: a retrospective analysis of acute care hospitals in America. Wound Repair Regen 17: 678-684.
- Lyderch AE (2008) Patient safety and quality: An evidence-based handbook for nurses.
- Gélis A, Dupeyron A, Legros P, Benaïm C, Pelissier J, et al. (2009) Pressure ulcer risk factors in persons with spinal cord injury part 2: the chronic stage. Spinal Cord 47: 651-61.
- Gedamu H, Hailu M, Amano A (2014) Prevalence and associated factors of pressure ulcers among hospitalized patients at felegehiwot referral hospital, Bahir dar, Ethiopia. Adv Nur.
- Anders J, Heinemann A, Leffmann C, Leutenegger M, Pröfener F, et al. (2010) Decubitus ulcers: pathophysiology and primary prevention. Dtsch Arztebl Int 107: 371-381.
- Bates-Jensen BM, McCreath HE, Pongquan V (2009) Subepidermal moisture is associated with early pressure ulcer damage in nursing home residents with dark skin tones: pilot findings. J Wound Ostomy Continence Nurs 36: 277-284.
- Lowthian P (2007) The distinction between superficial pressure ulcers and moisture lesions. Skinmed 6: 111-112.
- Fisher AR, Wells G, Harrison MB (2004) Factors associated with pressure ulcers in adults in acute care hospitals. Adv Skin Wound Care 17: 80-90.
- Allman RM, Laprade CA, Noel LB, Walker JM, Moorer CA, et al. (1986) Pressure sores among hospitalized patients. Ann Intern Med 105: 337-342.
- Baharestani MM, Black JM, Carville K, Clark M, Cuddigan JE, et al. (2009) Dilemmas in measuring and using pressure ulcer prevalence and incidence: an international consensus. Int Wound J 6: 97-104.
- de Araújo TM1, de Araújo MF, Caetano Jà (2012) Using the braden scale and photographs to assess pressure ulcer risk. Rev Esc Enferm USP 46: 858-864.
- Dilie A, Mengistu D (2015) Assessment of nurses’ knowledge, attitude, and perceived barriers to expressed pressure ulcer prevention practice in addis ababa government hospitals, addis ababa, ethiopia, 2015. Adv Nurs 11.
- Nuru N, Zewdu F, Amsalu S, Mehretie Y (2015) Knowledge and practice of nurses towards prevention of pressure ulcer and associated factors in gondar university hospital, northwest ethiopia. BMC Nurs 14: 34.
- Jiang Q, Li X, Qu X, Liu Y, Zhang L, et al. (2014) The incidence, risk factors and characteristics of pressure ulcers in hospitalized patients in China. Int J Clin Exp Pathol 7: 2587-2594.
- Bots TC, Apotheker BF (2004) The prevention of heel pressure ulcers using a hydropolymer dressing in surgical patients. J Wound Care 13: 375-378.
- Bredesen IM, Bjøro K, Gunningberg L, Hofoss D (2015) The prevalence, prevention and multilevel variance of pressure ulcers in norwegian hospitals: a cross-sectional study. Int J Nurs Stud 52: 149-156.
- Tsaousi G, Stavrou G, Ioannidis A, Salonikidis S, Kotzampassi K (2015) Pressure ulcers and malnutrition: results from a snapshot sampling in a university hospital. Med Princ Pract 24: 11-16.
- Petzold T, Eberlein-Gonska M, Schmitt J (2014) Which factors predict incident pressure ulcers in hospitalized patients? A prospective cohort study. Br J Dermatol 170: 1285-1290.
- Chou CL, Lee WR, Yeh CC, Shih CC, Chen TL, et al. (2015) Adverse outcomes after major surgery in patients with pressure ulcer: a nationwide population-based retrospective cohort study. PLoS One 10: e0127731.
Citation: Ebrahim J, Deribe B, Biru WJ, Feleke T (2018) Prevalence and Factors Associated with Pressure Ulcer among Patients Admitted in Hawassa University Referral Hospital, South Ethiopia. J Health Care Prev 1: 105.
Copyright: © 2018 Ebrahim J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 6095
- [From(publication date): 0-2018 - Apr 01, 2025]
- Breakdown by view type
- HTML page views: 5017
- PDF downloads: 1078