Prevalence and Characteristics of Hypertension and Other Cardiovascular Risk Factors in Native People in Argentine Patagonia
Received: 30-Oct-2017 / Accepted Date: 09-Nov-2017 / Published Date: 14-Nov-2017
Abstract
Objectives: Recent studies reveal that hypertension and cardiovascular risk factors have increased in natives in the entire American continent. Their prevalence in the native inhabitants of Argentine Patagonia (Tehuelches and Mapuches) is unknown. The aim of the present work was to assess that prevalence in a group of mixed Tehuelche and Mapuche people in the plateaus of the northern-central region of the province of Chubut, Argentine Patagonia.
Methods: We measured blood pressure in 181 native individuals in six villages. Subsequently they underwent fasting laboratory tests (glucose, cholesterol and triglycerides), assessment of body mass index, abdominal circumference and investigation for target organ damage.
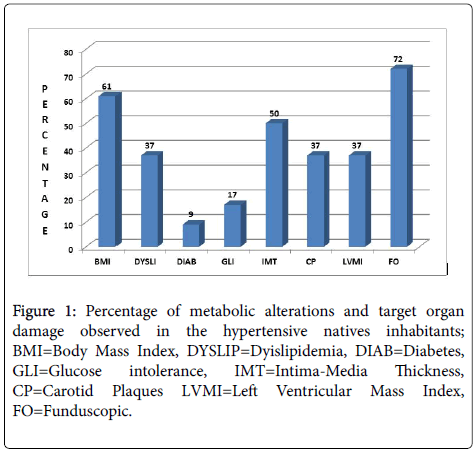
Results: The outcomes showed a prevalence of 25.4% of hypertension among them. In 60.9% of those who were hypertensive, we observed a body mass index over 30 Kg/m2, while different prevalence of dyslipidemia (36.9%), diabetes (3.3%), glucose intolerance (17.4%), increased left ventricular mass index (37%), carotid plaques (37%), an intima-media thickness over 9 mm (50%) and an abnormal fundus (71.7%) were also found. Hypertension was more common in males, and in unemployed, widowed and divorced people, but we did not observe a significant association between hypertension and diet, alcoholism or smoking or the lack of medical insurance.
Conclusion: We concluded that the prevalence of hypertension in Mapuche and Tehuelche inhabitants of Chubut is not significantly different from that of general populations of our country, nor those of other ethnic groups of the American continent, but the impact on target organ is seemingly greater for them.
Keywords: Hypertension; Blood pressure; Native inhabitants; Metabolic disorders; Argentine Patagonia; Aboriginal typical diet; Observational data
Introduction
High blood pressure (HBP) is a major cause of cardiovascular morbidity and mortality, both in developed and in developing countries [1]. In today’s world, there are still groups of people living in a relative isolation, keeping to a certain extent their ancestral customs, in which HBP barely prevails or does not exist [2]. Although previous studies showed a low prevalence of cardiovascular risk factors (CRF) in natives of the American continent, over the last decades they have increased, sometimes overcoming that of white people [3,4].
Argentine Patagonia is an immense phyto-geographical region, conventionally extended from the Colorado river in the Province of Río Negro to the southern end of the continent in Tierra del Fuego. The province of Chubut is located in the center of that region.
The native inhabitants (NI) of Chubut belong to two ethnic groups, the Tehuelches and the Mapuches. Their communities are relatively isolated, as a result of which they keep certain habits and traditions of their ancestral culture. Their typical diet is mainly based on sheep meat. An unpublished research work showed that Chubut NI, who eats large amounts of such meat, had normal plasma cholesterol levels and absence of coronary artery disease. The authors suggest the existence of a particular genetic condition regarding their lipidic metabolism, or that sheep fat could not increase cholesterol as beef fat does [5].
Although some research has already been done concerning other native groups in the American continent [3,6,7], including those in our country [8], and despite the realization of some works on Chilean Mapuches [9,10], to date, the prevalence of hypertension and other CRF in Tehuelches and Argentine Mapuches has remained unknown. The aim of our study was to evaluate the prevalence of hypertension and other CRF and potential target organ damage (TOD) produced by HBP in these ethnic groups, and to determine whether their diet or some other factors had influence on such conditions.
Methods
A group of seven doctors-two cardiologists, two clinicians and three ophthalmologists and a biochemical technician moved to the central and western areas of the Patagonian plateau in Chubut, specifically, to the small villages of Gastre, GanGan, Lagunita Salada, Yalalaubat and Blancuntre. According to demographic records, those places were important NI settlements. Thirty days before the start of the research study, we paid a visit to each of the selected villages, interviewing the doctors and nurses either in the local rural hospitals or health centers, in order to assess the context, inform them on the scope of our work, and prepare the logistics. Besides, with the intention of ensuring a substantial attendance of NI, considering their natural refusal to spontaneous collaboration with outcomes, we held a meeting with the chief of each settlement, so as to inform him on the scope of our study and obtain his group’s support.
The study protocol was submitted to and approved by the Ethics Committee of our Institution.
A month later we proceeded to the study, with the result that 181 persons out of an estimated population of 860 belonging to either of the two aforementioned ethnic groups were evaluated, 26% of the total regional NI, 118 of them being women (65%).
The inclusion criteria were: patients over 18 years of age, of both sexes, self-proclaimed as belonging to native ethnic groups and whose grandparents or parents had at least one Tehuelche or Mapuche family name. They were asked to come to the rural hospitals or health centers in fasting conditions. After being read aloud the written consent, they were asked to sign it. Then they answered a questionnaire on habits and socioeconomic conditions. Blood samples were obtained after a 12 h fast. Then, the following tests were performed: laboratory tests including total cholesterol (CHO), triglycerides (TGL) and glucose (GL), which were measured using automated enzymatic assays; assessment of body mass index (BMI); waist circumference (WHR) and measurement of blood pressure (BP). At the same time, the intima-media thickness (IMT), the presence of carotid plaques (CP) and left ventricular mass index (LVMI) were assessed using ultrasonography. Finally, they underwent a funduscopic examination (FE).
Glucose values between 110 and 125 mg/dl were considered as glucose intolerance (GLI) and a value of ≥ 126 mg/dl [11] as diabetes. An abnormal CHO and TGL concentration was considered if values were ≥ 200 mg/dl and ≥ TGL 150 mg/dl respectively [12]. For BMI the usual formula weight (kg) divided by height squared (m2) was used. The WHR was measured with a tape meter at umbilical level with the patient in maximal expiration, using the ATP III criteria for classification according to the waist-to-hip ratio, with cut-off points of ≥ 82 mm for women and ≥ 102 mm for men [12]. The BP was measured three times, using a calibrated mercury sphygmomanometer and in accordance with accepted international standardized protocols (sitting position, arm at heart level, feet flat on the floor, back against the backrest and the proper cuff size). The valid BP value resulted from the average of the three measurements [13]. Phases I and V of the Korotkoff sounds were used as an expression of systolic BP (SBP) and diastolic (DBP), respectively. HBP was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg or intake of antihypertensive medications. A portable echocardiograph MyLab 30 (Esaote, Genoa) was used for the measurement of LVMI and IMT. The LVMI was obtained by measuring the inter-ventricular septum and posterior wall of the left ventricle in diastole, from an average of three cardiac cycles with Bmode echocardiography in the short and long axes, corrected for body surface as recommended by the American Society of Echocardiography [14] (LVMI increased: men>125 and women>110 g/m2). The IM thickness was analyzed through bilateral measures of the distal third of the common carotid posterior wall at 1 cm from the bifurcation, performing at least 6 measurements, and taking as valid the highest average obtained on either side, considering>0.9 mm values as elevated ones [15]. For FE, the pupils were dilated and the findings were evaluated according to the recommendations of the American Academy of Ophthalmology [16].
Statistical analysis
Univariate analysis was performed in each variable studied. For the continuous variables, mean and standard deviation were assessed, and for the categorical variables, frequency tables were introduced. Hypertension was the response variable studied. To analyze the association of the response with the different variables, we used the ttest in the case of continuous variables and the chi-square test for categorical variables.
A logistic regression model was adjusted in multivariate analysis to altogether examine the variables IM, LVMI and FO. Through the use of the Hosmer and Lemeshow tests, we found that the models fitted the data significantly well. A P level
Results
Of the 181 NI studied, 46 (25.4%) had hypertension, 27 (58.7%) isolated systolic hypertension (ISH), 17 (37%) had systo-diastolic hypertension (SDH) and 2 (4.3%) had isolated diastolic hypertension (IDH). Hypertensive (HT) subjects were significantly older, 61.2 ± 13.9 years vs. 42.3 ± 18.7 in non-hypertensive subjects (p<0.001). Besides, hypertension was more frequent in men than in women (33% vs. 21%), although this association was not significant (p=0.115). In turn, HBP was considerably less frequent among individuals who had a job as compared to those who did not (18% vs. 33%), (p=0.019). Also, we found a significant relationship between hypertension and marital status, being it more prevalent among widowed and separated subjects (p=0.01). No significant association was observed between hypertension and the facts of having or not a medical insurance, (p=0.765), type of diet (p=0.074), alcohol consumption (p=0.124), or smoking (p=0.097) (Table 1).
| Characteristics | Total | High Blood Pressure | P Value | |
|---|---|---|---|---|
| (N=181) | No | Yes | ||
| (N=135) | (N=46) | |||
| Age (years) | 47.1 ± 19 | 42.3 ± 18.7 | 61.2 ±13.9 | <0.001* |
| Gender – N (%) | ||||
| Male | 63 | 42 (67) | 21 (33) | 0.115 |
| Female | 118 | 93 (79) | 25 (21) | |
| Work – N (%) | ||||
| Yes | 94 | 77 (82) | 17 (18) | |
| No | 87 | 58 (67) | 29 (33) | 0.019* |
| Medical Insurance – N (%) | ||||
| Yes | 64 | 46 (72) | 18 (28) | 0.765 |
| No | 117 | 89 (76) | 28 (24) | |
| Marital Status – N (%) | ||||
| Married | 33 | 20 (61) | 13 (39) | 0.01 |
| Single | 57 | 45 (79) | 12 (21) | 0.01 |
| Divorced | 9 | 7 (75) | 2 (25) | 0.01* |
| Widowed | 24 | 14 (52) | 10 (48) | 0.01* |
| Concubine | 58 | 49 (84) | 9 (16) | 0.01 |
| Diet – N (%) | ||||
| Only meat | 131 | 92 (70) | 39 (30) | 0.074 |
| Only vegetables | 3 | 3 (100) | 0 (0) | |
| Meat, vegetables, fruit | 47 | 40 (85) | 7 (15) | |
| Alcohol – N (%) | ||||
| Yes | 23 | 14 (59) | 9 (41) | 0.124 |
| No | 158 | 120 (77) | 36 (23) | |
| Smoking – N (%) | ||||
| Yes | 57 | 45 (79) | 12 (21) | 0.097 |
| No | 124 | 88 (71) | 36 (29) |
Table 1: Demographic characteristics, habits and socioeconomic conditions of the native inhabitants according to presence of hypertension.
Hypertension was considerably related to BMI (p=0.001), higher levels of CHO (p=0.005) and TGL (p<0.001), WHR (p<0.001), plasma levels of GL (p<0.001), IMT, LVMI (p=<0.001), presence of CP (p=0.015) and of FE abnormalities (p<0.001) (Table 2).
| Variables | Total | High Blood Pressure | P Value | |
|---|---|---|---|---|
| (N=181) | No | Yes | ||
| (N=135) | (N=46) | |||
| SBP | 127 (± 22.3) | 116.4 (± 11.4) | 158.2 (± 16.2) | <0.001 |
| DBP | 75.7 (± 12.1) | 71.8 (± 8.9) | 87.3 (± 12.6) | <0.001 |
| CHOL | 173.7 (± 24.4) | 170.7 (± 24.2) | 182.8 (± 22.7) | 0.005 |
| TGL | 97.9 (± 70.8) | 86.9 (± 55.8) | 130.9 (± 97.3) | <0.001 |
| GLU | 95.8 (± 29.8) | 94.1 (± 32.5) | 101.2 (± 18.3) | <0.001 |
| BMI | 29 (± 6.2) | 27.9 (± 5.8) | 32 (± 6.1) | <0.001 |
| WHR | 95 (± 13.3) | 93.2 (± 12.9) | 100.7 (± 13.1) | <0.001 |
| IMT | 0.8 (± 0.1) | 0.8 (± 0.1) | 0.9 (± 0.2) | <0.001 |
| LVMI | 94.9 (± 28.2) | 89.6 (± 24.5) | 111.2 (± 32.3) | <0.001 |
| DIAB | 6 (3.3%) | 2 (1.48%) | 4 (8.7%) | <0.001 |
| GLI | 11 (6.7%) | 3 (2.2%) | 8 (17.4%) | <0.001 |
| CP | 54 | 31 (23%) | 23 (50%) | 0.015 |
| Abnormal FO | 54 | 19 (14%) | 35 (76%) | <0.001 |
Table 2: Values of blood pressure and other variables studied, observed in the native inhabitants; SBP=Systolic BP; DBP=Diastolic BP; CHOL=Cholesterol; TGL=Triglycerides; GLU=Glucose; BMI=Body Mass Index; WHR=Waist Circumference; IMT=Intima-Media Thickness; LVMI=Left Ventricular Mass Index; DIAB=Diabetes; GLI=Glucose intolerance; CP=Carotid Plaques; FO=Funduscopic.
A percentage of 60.9% of HT BMI over 30 Kg/m2 (p=<0.001) was observed, while 36.9% had dyslipidemia (p=0.005), 17.4% had GLI (p=<0.001), 8.7 % were diabetic (p ≤ 0.001), 37% showed increased LVMI, 37% CP presence, 50% had a IMT over 9 mm and 71.7% showed abnormal FE (Figure 1). With regard to their diet, 72.4% reported to eat just sheep meat, 26% consumed beef, vegetables and/or fruit and 1.6% reported to be vegetarians.
Discussion
Despite the fact that earlier studies showed a low prevalence of cardiovascular risk factors, including hypertension, in natives of the American continent, over the last decades, they have increased, and even overcame, those observed in white individuals. For instance, In the United States of America, the Second National Health and Nutrition Examination Survey (NHANES II) [17], 226 subjects identified themselves as Native Americans. The outcomes showed no significant differences in the prevalence of hypertension with respect to that found in white people, nor in the incidence of deaths from strokes in individuals under the age of 65. These results were attributed to changes in lifestyle. In a similar population, Wang et al. studied 4.549 individuals, 1.760 of whom were identified as hypertensive (38.7%) and other 1.283 (28.2%) as pre-hypertensive, finding that the latter had 3.2 times higher risk of developing hypertension and 1.74 times of developing cardiovascular disease [6].
Two studies of hypertension prevalence were conducted in Chile. In one of them, studying 1,948 individuals out of 28 Mapuche communities, the outcomes showed that 13% of men and 16% of women were hypertensive. In the other one, out of 345 Mapuche individuals, a hypertension prevalence of 20.4% in men and 18.8% in women was found [10,18]. In Argentina, a study on 522 individuals in a Wichi-chorote community showed that 37% were pre-hypertensive and 28% suffered hypertension [8]. Our study showed a hypertension prevalence of 25.4% in Tehuelche and Mapuche ethnic groups with marked target organ damage. Although total percentages were lower than those observed in different epidemiological studies conducted on general population of our country [19-21], they were similar to those obtained in other NI communities in the southern end of the continent [9,10].
The type of HBP more frequently found was isolated systolic hypertension, with high BP average values, in accordance with the highest prevalence of this type of HBP in this age group. This result could also be connected to a higher mean age of the hypertensive subjects in our sample and possibly to the greater target organ damage found. In our subjects, hypertension was positively associated with age and unemployment both variables are often related with it and it was also connected to the fact of being the subjects widowed or singles, which might suggest a degree of chronic stress resulting from loneliness and some degree of social isolation. These groups of people have easy access to free public health care-the only option in the areawhich may explain the lack of relationship between hypertension and the fact of having or not a medical insurance. To our surprise, we found a weak connection between two variables traditionally related to the presence of hypertension: the consumption of tobacco and alcohol. This may reflect the underreport of those conditions, especially in the case of alcohol, probably due to denial of the habit. With regard to smoking, however, there have been conflicting results in the different populations studied, since in some studies, for unclear reasons, authors could not find a relation between smoking and hypertension. [6,22]
In the analyzed NI we observed a remarkable target organ damage. As far as we know, unlike most regional studies, ours is one of the few ones-if not the only one-in which TOD has been evaluated in this kind of ethnic groups. Over one-third of the hypertensive NI presented structural cardiovascular damage: a significant IMT increase, presence of CP and LVMI as well as alterations in FE. On the other hand, in these subjects we found a consistent association between hypertension and metabolic disorders, with significant prevalence of obesity, overweight, TGL and abnormal fasting glucose values. Sedentary lifestyle, poor socioeconomic conditions and racial genetic mechanisms could be possible reasons explaining these alterations.
In our region, sheep meat is considered healthier than beef and it is thought that its intake does not produce the known lipid disorders of the latter. Even though we have not found any research studies assessing the potential differences between the cardiovascular effects of these two types of meat, sheep meat has a high unsaturated fatty acid to saturated fatty acids ratio. One of its components, conjugated linoleic acid, is found only in ruminants’ meat and dairy products and it is produced out of linoleic acid by their gastrointestinal flora. In human beings, some studies suggest that linoleic acid would have a protective role in certain types of cancers, such as colorectal and breast cancer [23-25], and administered in supplements, it reduces the body fat, especially the abdominal one [26]. However, it could also have cardiovascular adverse effects since it could enhance insulin resistance as well as oxidative stress [27], and it could decrease the docosahexaenoic acid [28]. Although 73% of the population we studied claimed that they only ate sheep meat and little or none of other kinds of food, multivariate analysis showed no association between this diet and hypertension.
Limitations
Today we know that racial purity cannot be established among human beings, but our country is a special case of mixture of people of different origins. In the case of the subjects of our study, having an European surname does not imply having an ancestor of that origin, since in the past many aborigines used to adopt an European name, which implied prestige. This circumstance implies that some persons actually belonging to the Tehuelche or Mapuche ethnic groups might have been discarded.
Notwithstanding the fact of the small number of subjects entering the study (N=181), they represent a significant part of the 700 person in the area that are registered as belonging to either the Tehuelche or Mapuche ethnias, according to the censuses.
On the other hand, even though the subjects involved were encouraged to answer all the epidemiological questions truthfully, some responses such as the low consumption of tobacco and alcoholwhich do not coincide with the known habits of these native inhabitants- make us infer a misleading data collection. Probably, the consumption of tobacco and alcohol is not as low as they claimed. If so, conclusions regarding the connection between such habits and the presence of hypertension would have been different.
We conclude that the prevalence of high blood pressure in native inhabitants of the province of Chubut (Tehuelche and Mapuche ethnic groups), although being a little lower that known in some other populations of our country or in other ethnic groups of the American continent, does not differ significantly. But it has a great impact on target organ damage. Besides, the massive consumption of sheep meat could not have an impact in developing hypertension. On the other hand, taking in account the metabolic alterations we found, it could not have any metabolic preventive benefits with respect to the consumption of cow meat. Sedentary lifestyle, racial-genetic characteristics, poor socioeconomic conditions, or perhaps some other unknown or not evaluated factors could explain the marked organ damage and metabolic disorders observed in this people.
Acknowledgements
For their help in recollection of data and participation in clinical work: Dr. Ana M Carletti, Dr. Lidia Carrizo, Dr. Ana Daroca, Dr. Mario Del Poppolo, Dr. Gabriela Guevara, Dr. Juan Kasaiñuk, Dr. Fernando Suarez, and Dr. Sergio Zambianchi.
References
- Flack J, Nasser S, O'Connor S (2008) Ethnicity and socioeconomic status in hypertension. Hypertension Primer Fourth Edition. Lippincott Williams & Wilkins Chapter B84: 276-280.
- Oliver WJ, Cohen EL, Neel JV (1975) Blood pressure, sodium intake, and sodium related hormones in the Yanomamo Indians, a "no-salt" culture. Circulation 52: 146-151.
- Galloway JM (2002) The epidemiology of atherosclerosis and its risk factors among native americans. Curr Diab Rep 2: 274-281.
- Gillum RF (1995) The Epidemiology of Stroke in Native Americans. Stroke 26: 514-521.
- Quiroga A, Onzari M (1993) Aboriginal Community Chubut. Comunidad AborÃgen del Chubut. Salud y Enfermedad Genética o Nutrición Resumen de los Trabajos presentados en el XX Congreso Argentino de CardiologÃa. Rev Arg Of Cardiol 6: 40.
- Wang W, Lee E, Fabsitz R, Devereux R, Best L et al. (1993) A Longitudinal Study of Hypertension Risk Factors and Their Relation to Cardiovascular Disease: The Strong Heart Study. Hypertension 47: 403-409.
- Gizlice ZS (2004) Huston Health Risks and conditions Among American Indians in North Carolina. State Center for Health Statistics. SCHS Studies. 146.
- Coghlan E, Bella Quero L, Schwab M, Pellegrini D, Trimarchi H (2005) Prevalence of hypertension in an Aboriginal community in northern Argentina. Medicine 65: 108-112.
- Stockins B, Larenas G, Charles M, Standen ID, Espinoza O, et al. (1998) Serum lipids and blood pressure levels in the +Mapuche population living in the Chilean region of AraucanÃa. Rev Méd Chil 126: 1291-1299.
- Pérez F, Carrasco E, Santos JL, Calvillán M, Albala C (1999) Prevalence of obesity, hypertension and dyslipidemia in rural aboriginal groups in Chile. Rev Méd Chil 127: 1169-1175.
- American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 34: S62-S69.
- Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 285: 2486-2497.
- European Society of Hypertension-European Society of Cardiology (2003) Guidelines for the management of arterial hypertension. J Hypertens 21: 1011-1053.
- Schiller NB, Shah PM, Crawford M, De Maria A, Devereux R, et al. (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2: 358-367.
- Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R (1986) Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 74: 1399-1406.
- Scheie HG (1953) Evaluation of ophthalmoscopic Changes of hypertension and arteriolar sclerosis. AMA Arch Ophthalmol 49: 117-138.
- US Department of Health and Human Services, Centers for Disease Control and Prevention. The Second National Health and Nutrition Examination Survey (1976-1980).
- Santos JL, Pérez-Bravo F, Carrasco E, Calvillán M, Albala C (2001) Low prevalence of type 2 diabetes despite a high average body mass index in the Aymara natives from Chile. Nutrition 17: 305-309.
- Lena SM, Cingolani HE, MA Almiron Echeverria R (1995) Prevalence of arterial hypertension in a rural population of Buenos Aires. Medicina 55: 225-230.
- Carbajal HA, Salazar MR, Riondet B, Rodrigo H, Quaini S, Rechifort V, et al. (2001) Variables asociadas a hipertensión arterial en una región de la Argentina. Medicina 61: 801-809.
- Encuesta Nacional de Nutricion y Salud (2007) Ministerio de Salud y Bienestar Social de la República Argentina.
- Rywik SL, Williams OD, Pajak A, Broda G, Davis CE, et al. (2000) Incidence and Correlates of hypertension in the Atherosclerosis Risk in Communities (ARIC) study and the Monitoring Trends and Determinants of Cardiovascular Disease (POL-MONICA) project. J Hypertens 18: 999-1006.
- McGuire MA, McGuire MK (2000) Conjugated linoleic acid (CLA): A ruminant fatty Acid with beneficial effects on human health. J Anim Sci 77: 1-8.
- Belury MA (2002) Inhibition of carcinogenesis by conjugated linoleic acid: potential-mechanisms of action. J Nutr 132: 2995-2998.
- Wang LS, Huang YW, Sugimoto Y, Liu S, Chang HL, et al. (2006) Conjugated linoleic acid (CLA) up-regulates the estrogen-regulated cancer suppressor gene, protein tyrosine phosphatase gamma (PTPgama) in human breast cells. Anticancer Res 26: 27-34.
- Blankson H, Stakkestad J, Fagertun H, Thom E, Wadstein J, et al. (2000) Conjugated Linoleic Acid reduces body fat in overweight and obese humans. J Nutr 130: 2943-2948.
- Risérus U, Basu S, Jovinge S,  Fredrikson GN, Arnlöv J, et al. (2002) Conjugated Linoleic Acid Supplementation With Causes Isomer-Dependent Oxidative Stress and Elevated C-Reactive Protein. A Potential Link to Fatty Acid-Induced Insulin Resistance. Circulation 106 : 1925-1929.
- Kelley D, Bartolini G, Newman J, Vemuri M, Mackey B (2006) Influence of dietary fatty acids on human health with emphasis on immune and inflammatory responses. Prostaglandins Leukot Essent Fatty Acids. 74: 331-338.
Citation: Ingaramo RA, Williams D (2017) Prevalence and Characteristics of Hypertension and Other Cardiovascular Risk Factors in Native People in Argentine Patagonia. Atheroscler Open Access 2: 117.
Copyright: ©2017 Ingaramo RA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 4488
- [From(publication date): 0-2017 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 3640
- PDF downloads: 848