Prevalence and Associated Factors of Low Birth Weight among Newborns Delivered at Public Hospital, in Hadiya Zone, Ethiopia
Received: 16-Dec-2019 / Accepted Date: 17-Feb-2020 / Published Date: 24-Feb-2020 DOI: 10.4172/2376-127X.1000427
Abstract
Back ground: Low birth weight (LBW) has been defined by the World Health Organization (WHO) as weight at birth of less than 2,500 grams including 2,499 grams irrespective of gestational age. LBW is a sensitive indicator for predicting the chance of infant healthy growth and development and a primary determinant of infant mortality risk. LBW is either the result of preterm birth or due to restricted fetal growth.
Objective: To assess the prevalence of Low Birth Weight and associated factors among newborns delivered in public hospital facilities, in Hadiya Zone, Ethiopia from March 30-June 30, 2010 E.C.
Method and materials: A hospital-based cross sectional study design was conducted on 282 mothers who give birth in three Hospitals in Hadiya Zone March 30 to April 30, 2018. Data was collected using pre-tested structured questionnaire. Data was entered in to Epi data version 3.1, then export to SPSS version 20 for data cleaning and analysis. Binary logistic regression was used to see the association between the outcome variable and explanatory variables. The candidate variable for association (PV<=0.5) was inter by backward multivariate logistic regression and
predictors was determined.
Result: Among the total 282 respondents, 277.16(5.7%) were MUAC<17 cm, 205(72.7%) respondents took less than four feedings per day and 127(45%) feed irregularly during pregnancy. Respondents who were not supplied by additional feeding during pregnancy were 69(24.5%). Thirty seven (13%) had Less than 37 week of gestational age during delivery of mothers and 81(28.7%) respondents had unknown gestational age. The new born babies mean birth weight was 2981.4 gm (SD ± 607.5). In this particular study the prevalence of low birth weight was 49(17.4%). In the
bivariate &multivariate logistic regression model mother had less than 37 weeks (AOR, 14.978 (4.685, 47.887), mother without additional food (AOR, 3.226(1.556, 6.686), mother had irregular meal pattern (AOR, 2.078 (1.034, 5.634), were identified independent predictor of low birth weight.
Conclusion and recommendation: The prevalence of low birth weight in this study was high. Absence of nutritional counselling at ANC, irregular pattern of meal, low additional food during pregnancy and preterm gestational age were predictor of low birth weight. Advising on additional food and regular meal pattern are mandatory for decreasing low birth weight.
Keywords: Prevalence; Predictors; Low birth weight; Antenatal care; Delivery; Birth outcome
Keywords
Prevalence; Predictors; Low birth weight; Antenatal care; Delivery; Birth outcome
Introduction
Background
Low birth weight (LBW) has been defined by the World Health Organization (WHO) as weight at birth of less than 2,500 gm including 2,499 gm irrespective of gestational age [1,2]. LBW is a sensitive indicator for predicting the chance of infant healthy growth and development and a primary determinant of infant mortality risk. LBW is either the result of preterm birth or due to restricted fetal growth. LBW is a sensitive indicator for predicting the chance of infant healthy growth and development and a primary determinant of infant mortality risk [3,4]. LBW is either the result of preterm birth or due to restricted fetal growth. It is closely associated with fetal and neonatal mortality and morbidity, inhibited growth and cognitive development and chronic diseases later in life. Worldwide, about 16% of live births or some 20 million infants per year are born with less than 2500 gm of weight and 90% of them are born in developing countries [5]. LBW is a leading cause of neonatal mortality [6]. It is now also incriminated in the occurrence of many chronic diseases in adult life time, these include adult-onset diabetes, coronary heart disease and high blood pressure, intellectual, physical and sensory disabilities. However, little attention is paid to birth weight improvement as a means of reducing child mortality [7]. In most developing countries, it was approximated that every ten seconds an infant dies from a disease or infection that can be attributed to LBW [5]. Those who had a history of Very Low Birth Weight (VLBW) are 2.6 times at risk of respiratory failure requiring mechanical ventilation [8]. Although about one-half of all LBW infants in industrialized countries are born preterm (<37 weeks of gestation), most LBW infants in developing countries are born at term and are affected by intrauterine growth restriction that may begin early during pregnancy [9]. As children, LBW infants are more likely to have disabilities, hospitalizations, brain damage and poorer language development, be placed in special education classes and display more intellectual impairments [10]. Across the world neonatal mortality is 20 times more likely for LBW babies compared to heavier babies (>2500 gm) and it increases sharply as birth weight (BW) decreases [11].
WHO shows that factors contributing to LBW in developing countries include, in order of importance, inadequate weight gain during pregnancy, low pre pregnancy weight, short stature, malaria and female sex of the fetus [12]. Other factors which are associated with LBW include hard physical work during pregnancy and illness, especially infections, social factors such as lower status of women, malnutrition, lack of antenatal care (ANC) etc. [3,5]. Mothers who had multiple gestations had a higher risk of delivering LBW babies [13].
In Ethiopia, studies showed that the prevalence of LBW varies from 6-10% [10]. Another retrospective study conducted to establish BW changes at Tikur Anbessa Hospital showed that LBW has increased trend between 1976 and 1996. According to the 2005/06 annual activity report of the Addis Ababa City Administration, Health Bureau, the rate of LBW among all deliveries attended from health institutions reporting to the city health bureau is 11% [5]. In another paper, more than 60% of all LBW are preterm. Some are both premature and growth retarded while others may be full term, but underweight (small for gestational age) [14]. Hence, LBW is still a challenging problem for the child’s health and affecting the health cost of the government and the society. Therefore, the overall work of this study assessed the determinant factors of low birth weight among newborns delivered at Hadiya Zone Hospitals. Thus, it was provide valuable information to the health professionals, researchers, regional health bureau and other stakeholders act upon it.
Statement of the problem
Globally, World Health Organization (WHO) estimates that 26 million low birth weight infants are born each year, constituting 17% of all births. It is nearly 95% of them are in the developing world [15]. But the prevalence estimate greatly varies across regions and even within country. Prevalence varies from 9% in Latin America, 13% in sub-Saharan Africa to 28% in south Asia. It continues to be a significant public health problem globally affecting about 15% to 20% (more than 20 million births) of all births worldwide [12].
LBW remains a significant public health problem in many developing countries with preconception and pregnancy nutrition is important factors. LBW infant in turn are at higher risk of perinatal death, adult hood stunting and the intergenerational effect of malnutrition continues. Intrauterine growth and development is one of the most vulnerable periods in the human life cycle, which accounts for about 50% of causes of LBW. Poor maternal nutrition is a known cause of LBW accounting for about 50% of cases of LBW in many developing countries. Those with poor nutrition have higher chance of giving LBW baby [9].
It is also powerful predictor of infant growth and survival. It is estimated that infants weighing less than 2,500 gm are approximately 20 times more likely to die than heavier babies and contributes to a range of poor health outcomes [1]. LBW has been recognized as one of the most important factors affecting child morbidity and mortality, accounting about 28 and 30% of neonatal deaths [10]. Similarly LBW found to be important secondary factor in 40%-80% of neonatal deaths. It has great economic burden to health institution for postpartum hospitalization and treatment. It is also associated with both short term increased morbidity, mortality and at increased risk of adulthood chronic disease like diabetics, hypertension and others [12]. LBW infants are also at elevated risk for developing psychiatric problems in childhood and adolescence, particularly attention-deficit, anxiety disorders and social difficulties. In addition they are also increased risk of infection, malnutrition and children who survive LBW have a higher incidence of diseases, mental retardation and chronic disease [13]. In most developing countries it was approximated that every ten seconds an infant dies from a disease or infection that can be attributed to low birth weight. Many of those infants who survive suffer cognitive and neurological disability in later life [5].
Educational status of mothers, mother’s age at first birth, wealth index, sex of child, type of birth, anemia status of mothers, maternal nutrition status and number of antenatal care during pregnancy were important determinants of baby’s size at birth in Ethiopia [16].
In Ethiopia the LBW estimate has risen from 2000 to 2005 from 15.0 % to 20.3% with 1.1% increase per year [17]. In Ethiopia, having one of the highest neonatal mortality rate in the world, recent estimates shows that the median prevalence of low birth weight is around 11% and ranges high up as 23%. Mother’s height, mother’s weight, anemia, physical work, tobacco chewing and history of abortion are significant determinants of LBW [18].
Similarly LBW is associated with low socio-economic status, multiparty, low weight gain during pregnancy, short maternal stature and anemia. Additionally Economic, social and cultural factors further make it difficult for mothers not to get appropriate nutrition and health care [19].
Low birth weight is public health problem, caused by factors that are potentially modifiable and the costs of preventing them are well within reach, even in poor countries like Ethiopia. It is therefore imperative to identify risk factors for LBW in various communities in the country in order to come up with feasible intervention strategies to minimize the problem. Identification of maternal risk factors associated with LBW is essential in order to guide program planning and organizing care for mothers and their newborns. It is expected that identifying those risk factors were unable to reverse the increasing trend of LBW in Ethiopia and thereby it is immediate and long term consequences [19].
The study was conducted by directly measuring newborns weight within 2 h of delivery in randomly selected one general hospitals and two primary hospitals which was to fill the gap of many studies conducted in Ethiopia that uses maternal subjective evaluation of the babies size at birth that is difficult for most of the mothers to recall and some other studies merely base their estimates from major medical centers that makes difficult for generalization because most of the delivering mothers in this facilities most referral
In Ethiopia, studies done on determinant factors of LBW were very limited and in Hadiya Zone Hospitals as well. This paper was examine LBW and associated factors among pregnant women delivering in public health facilities in Hadiya Zone.
Significance of the study
This study could provide useful information that would inform hospital facilities prepare special care plan for LBW neonates, most dies within 24 h of delivery due to absence of adequate and special care. As limited in the study area, the findings from this study were providing baseline data for further researches and interventions.
Also contributed for Hadiya Zone health department, administrators and other concerned organizations and stakeholders to give great emphasis to the problem and take appropriate measures towards the initiation of a suitable nutrition and health promotion programs for pregnant women, which contribute its great share for decreasing the prevalence of LBW neonates.
In addition, the study may be useful to other researchers as reference material while conducting further studies on similar problems. Identification of maternal risk factors associated with LBW is also essential in order to guide program planning and organizing care for mothers and their newborns. It is expected that identifying those risk factors will enable to reverse the increasing trend of LBW in Ethiopia particularly in Hadiya and there by its immediate and longterm consequences.
Literature Review
Prevalence of low birth weight
An institution based comparative cross-sectional study using consecutive sampling technique to assess the prevalence and associated factors of Low Birth Weight in Axum (urban) and Laelay Maichew (rural) districts, Tigray, north Ethiopia on 520 live birth neonates from both urban and rural district shows a low birth weight prevalence of 9.9% and 6.3% in Axum and Laelay Maichew districts, respectively [20,21].
A cross-sectional study in Jimma Ethiopia shows 22.5% LBW prevalence. Mothers residing in the urban setting had higher risk of delivering LBW babies (p=0.001) [13]. While study conducted in Kersa Demographic Surveillance and Health Research Center (KDS-HRC) field site shows an incidence of LBW as 28.3% which may underestimate the actual prevalence (21).
In contrary Ghana study on 1200 samples showed 21.1% prevalence. A nationally representative, cross-sectional surveys in India shows the prevalence of LBW was 20.5% (95% CI: 19.5%, 21.4%) in 2005/2006 (P=0.079). The prevalence of LBW was higher among younger mothers and those with a lower BMI [19].
Factors associated with low birth weight
Demographic and socio-economic factors: Socio-Economic Status (SES) indicators, including maternal education, on birth weight and IUGR, maternal illiteracy and low SES are found to be associated with LBW and IUGR [22]. A study conducted in three hospitals in Mexico City shows women in low SES double burden (AOR, 2.19, 95% CI, 1.18-4.07) than those in the medium and high SES [23]. Similarly other study shows male have lower odds of being LBW [24]. In contrary cross-sectional study, conducted on 305 live births in Northwest Ethiopia shows female newborns have higher odds of LBW than males [7]. Also being female neonate is associated with four and six more odds of being LBW [20].
Objectives
General objective
To assess the prevalence of low birth weight and associated factors among newborns delivered in public hospital facilities, in Hadiya Zone, Ethiopia from March 18-June 18, 2010 E.C.
Specific objectives
1. To assess the prevalence of low birth weight among newborns delivered in public hospital facilities in Hadiya Zone.
2. To identify factors associated with low birth weight among newborns delivered in public hospital facilities in Hadiya Zone.
Methods and Materials
Study area and period
Hadiya Zone was one of the Fourteen Zones and 5 special districts in South regions. It shared borders with the Gurage in North Silte in East, Kembata tembaro & Wolaita in South, Alaba special districts in South East, in west Oromiya and South West Dawuro zone, Yem special district in North. The elevation was 2,000-2500 m above sea level. The Zone of Hadiya drives its name from Arabic language: Hadiya "Gift". The dominant economic sector is primarily agriculture. Hadiya zone administration divided into 2 urban administrations and 10 rural administrations. It has 329 kebele, from this 303 are rural and 29 urban kebeles. The total population was 1,705,902 (male 848,695 and female 857,225). Male to Female sex ratio is 1:1.01(2010 E.C). Reproductive age group (15-49 years) were (397,475)23.3% from total population. The study was conducted from March 30-April 30, 2010 E.C in three public hospitals in Hadiya Zone.
Study design
Facility based cross sectional study was conducted.
Population
Source population: All mothers who delivered newborn at Hadiya Zone public Hospitals during data collection period.
Study population: All randomly selected mothers who delivered newborn at Hadiya Zone public Hospitals during data collection period
Eligibility criteria
Inclusion criteria: Mothers who delivered newborn at Hadiya Zone public Hospitals during the study period.
Exclusion criteria: Multiple birth, mother who had known chronic disease, preterm/premature birth, critically ill, newborns weighed after 1 h of delivery and still birth
Sample size determination
The sample size was calculated using a single proportion population formula. Proportion of low birth weight 22.5% from previous study conducted at Jimma Ethiopia 95% CI, 5% non-response and 5% marginal error were used [18]. The total sample was 282.
Sampling procedure
All three hospitals were selected namely Nigisteleni Mohamed memorial general hospital, Shone primary and Homacho primary hospitals was included in the study.
The calculated sample size (282) was proportionally allocated to these hospitals based on delivery case load of each hospital facility. Finally the respondents were selected systematically by skipping every third neonate until the needed sample size was met.
Data collection methods and tools
The data was collected using structured, pretested interviewer administered questionnaire. Six BSc senior mid wives were employed to collect the data as well as one supervisor (head of delivery case team) was assigned to follow data collection. The data collectors were trained for one day on how to collect the data, how to select respondents systematically in every third mother by neonate. Data was collected through interviewing the mother and measuring the weight of the newborn, height, weight and MUAC of the mother and the measurement was held twice. Maternal weight and MUAC was taken after the mother arrived and became stable after delivery. The main outcome variable was collected through a beam balance for newborn weighting. Immediately after delivery and within 1 h newborn was placed in weight measuring beam balance and the measurements was rounded to nearest 100 gm. Maternal MUAC was measured using non stretchable MUAC tape by data collectors. Standardization was done for maternal MUAC by using TEM and Relative TEM.
Variables
Dependent variable: The weight of the newborn
Independent variables: Age of mother, Educational status, Residence, Income, Chat chewing, Sex of newborn ANC follow up, Time of initiation of ANC, Number of ANC, Iron and foliate supplementation, Dietary advice during ANC, Parity, Birth Interval, Maternal nutritional status, Anemia, Additional dietary, Intake during pregnancy, Gestational Age at birth and Mothers work condition.
Operational definitions
BMI (body mass index): It was nutritional assessment based maternal weight after birth in Kg divided by height in cm squared. BMI less than 18.5 kg/cm2 was considered as low while above 18.5 kg/cm2 is considered as normal.
Birth interval: It was defined as the length of time between two successive live births [1].
Birth weight: It was the first weight of the fetus or newborn obtained after birth [1].
Low birth weight (LBW): It was defined as weight of child at birth less than 2500 gm measured within 1 h of birth.
Public hospitals: Governmental Hospitals in Hadiya zone.
Educated: Respondents who can read and write and above.
Uneducated: Respondents who cannot read and write.
Data processing and analysis
The data were entered in to Epi-data software version 3.1. Then data was checked through double entry of 10% (28 respondent questioners used for both upper and lower entry to keep data quality) and validated via Epi-data software version 3.1. Then the data was exported to SPSS Version 20 for analysis. Descriptive statistic including Proportion, frequency distribution, Mean (SD) and Median was used to describe the data on the sample population in relation to relevant variables. In bivariate analysis cross tabulations was done to see the association between the explanatory and outcome variables. Multivariable logistic regression was employed by selecting only variables that appeared to be statistically significant at (P<=0.05) in the bivariate analysis. Model fitness was checked by Hosmer-Lemeshow goodness-offit test. Finally the data was presented with appropriate tables, diagrams and figures.
Adjusted odd ratio was calculated to check strength of association at P<=0.05 was taken as significant association.
Data quality control
The questionnaire was prepared in English and translated in to Amharic and “Hadiyisaa” language and translated back to English to keep the consistency of the questions and increase understanding with respondents. To ensure quality of data, data collectors was trained for one day on the proper collection of data and accurate measurement of birth weight of child and Height, weight and MUAC of mother and standardization was made for MUAC by calculating Relative TEM for all data collectors which was less than 3%. The instrument was pretested in Durame General hospital facilities on 5% of the Sample size before the actual data being collected [14]. Then it was checked for wording, way of asking and Chronbach's Alpha of questionnaire reliability scale was 0.7083. Supervisors daily checked data collectors and collected data for consistency. Appropriate correction was made accordingly. Before analysis data editing, coding and cleaning were employed.
Ethical consideration
First the research was approved by Wachamo University ethical review committee for the ethical issues in conducted study. Then ethically approval letter was taken to the respective Hospital facility managers and the finding was disseminated.
Dissemination of the study results
The final finding of this study was presented and disseminated on Wachamo University. Also it was disseminated to the respective Hospitals in Hadiya zone and Zonal health department as it was guide for their implementation.
Results
Socio demographic characteristics of the respondents
Data were collected from 282 mothers and neonates with a 100% response rate. The mean age of the mother was 26.7 years (SD ± 4.6). The majority of mothers 182(64.5%) were aged 19-28 years followed by 29-38 years 93(33%). Most of the respondents were married 265(94%), the majority 200(70.9%) were protestants. Majority of the participants were Hadiya 225(79.8%). Educational status 87 (30.9%) of mothers completed secondary and 55(19.5%) were not read and write. Majority of mothers 264 (93.6%) were working during last pregnancy.
More than half 194 (68.8%) and 52 (18.4%) of the respondents were residing in urban areas and not known birth space, respectively (Table 1).
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Age | 19-28 years | 182 | 64.50% |
| 29-38 years | 93 | 33% | |
| >38 years | 7 | 2.50% | |
| Residence | Urban | 194 | 68.80% |
| Rural | 88 | 31.20% | |
| Ethinicity | Hadiya | 225 | 79.80% |
| Gurage | 25 | 8.90% | |
| Silte | 17 | 6% | |
| Kambata | 12 | 4.30% | |
| Amhara | 2 | 0.70% | |
| Others | 1 | 0.40% | |
| Protestant | 200 | 70.90% | |
| Religion | Orthodox | 62 | 22% |
| Muslim | 18 | 6.40% | |
| Others | 2 | 0.70% | |
| Educational status | Not read and write | 51 | 18% |
| Read and write | 80 | 28% | |
| Primary | 64 | 23% | |
| Secondary and above | 87 | 31% | |
| Marital status | Married | 265 | 94% |
| Single | 5 | 5.30% | |
| Divorced | 2 | 0.70% | |
| 7)Monthly income | <500 EBR | 46 | 16.3 |
| 500-1000 EBR | 21 | 7.4 | |
| >1000 EBR | 215 | 76.2 |
Table 1: Demographic and Socio economic characteristics of the respondents, Hadiya zone, South Ethiopia, 2010 EC.
Obstetric health care related maternal characteristics
Two hundred twenty seven mothers (80.5%) were MUAC>21 cm and 55(19.5%) were <21 cm. About 205(72.7%) respondents took less than four feedings per day and 127(45%) feed irregularly.
Hemoglobin level of less than 12 g/dl was seen among 46(16.3%) respondents before delivery. Less than 37 week of gestational age during delivery was found among 37(13%) of mothers and 81(28.7%) were by unknown gestational age. Among the new born about 154(54.6%) were females. Birth weight of less than 2500 gm or low birth weight was found among 49(17.4%) of new born babies with a mean birth weight of 2981.4 gm (SD ± 607.5)
About 265(94%) of respondents had accessed ANC follow up during their pregnancy and 202(71.6%) respondents were supplemented with iron folic acid tablet during their Antenatal follow up, but 80(28.4%) were not. About 46(16.3%) of the respondents were anemic during their pregnancy and respondents who were not supplied by additional feeding during pregnancy was 69(24.5%). Mothers about 55(19.5%) were MUAC<21 cm (Table 2).
| Variables | Categories | Frequency | Percent (%) |
|---|---|---|---|
| MUAC | <17 | 16 | 5.7 |
| 17-21 | 95 | 33.7 | |
| >21 | 171 | 60.6 | |
| Iron intake | Yes | 199 | 70.6 |
| No | 83 | 29.4 | |
| ANC follow | Yes | 265 | 94 |
| No | 17 | 6 | |
| ANC visit | 01 Feb | 51 | 19.25 |
| 03 Apr | 212 | 80 | |
| >4 | 2 | 0.75 | |
| Maternal Hgb status | <12 | 46 | 16.3 |
| Dec 14 | 205 | 72.7 | |
| >14 | 31 | 11 | |
| Maternal gestational age | less than 37 weeks | 36 | 12.8 |
| 37-42 weeks | 161 | 57.1 | |
| above 42 weeks | 1 | 0.4 | |
| Unknown | 84 | 29.8 | |
| Hypertension | Yes | 8 | 2.8 |
| No | 274 | 97.2 | |
| Smoking | Yes | 2 | 0.7 |
| No | 280 | 99.3 | |
| Additional meal | Yes | 202 | 71.6 |
| No | 80 | 28.4 | |
| Meal per day | 01 Feb | 9 | 3.2 |
| 02 Mar | 19 | 6.7 | |
| 3 | 184 | 65.2 | |
| 4 and above | 70 | 24.8 | |
| Birth weight | <2500 gm | 49 | 17.4 |
| >=2500 gm | 232 | 82.3 | |
| Birth interval | less than 2 years | 167 | 59.2 |
| greater than 2 years | 115 | 40.8 |
Table 2: Distribution of maternal and child health status Hadiya zone health facility, Oct 2018.
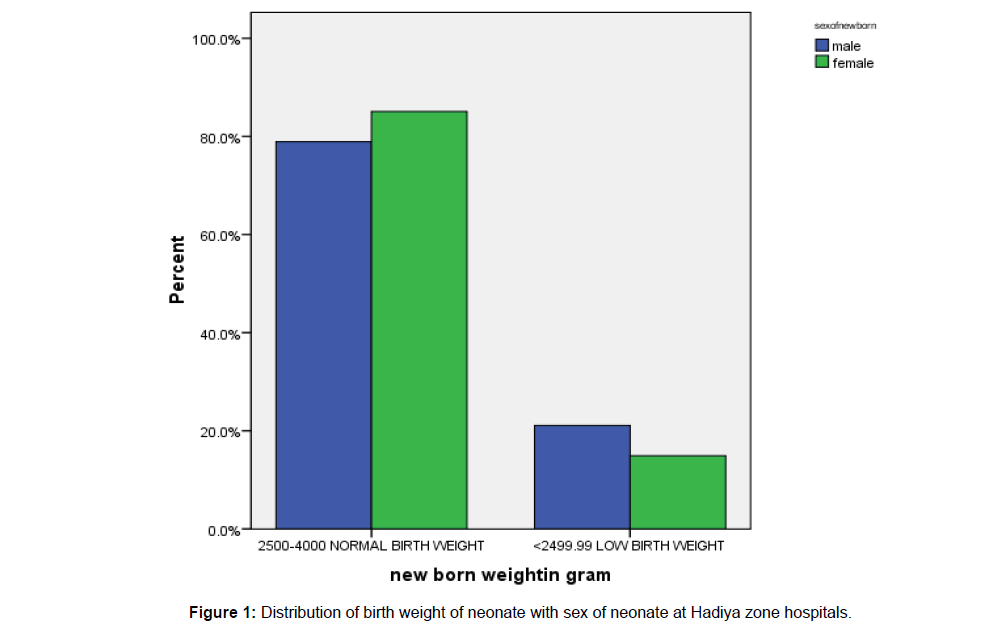
Among the total low birth weight neonate, female neonates had normal birth weight than male neonate (Figure 1).
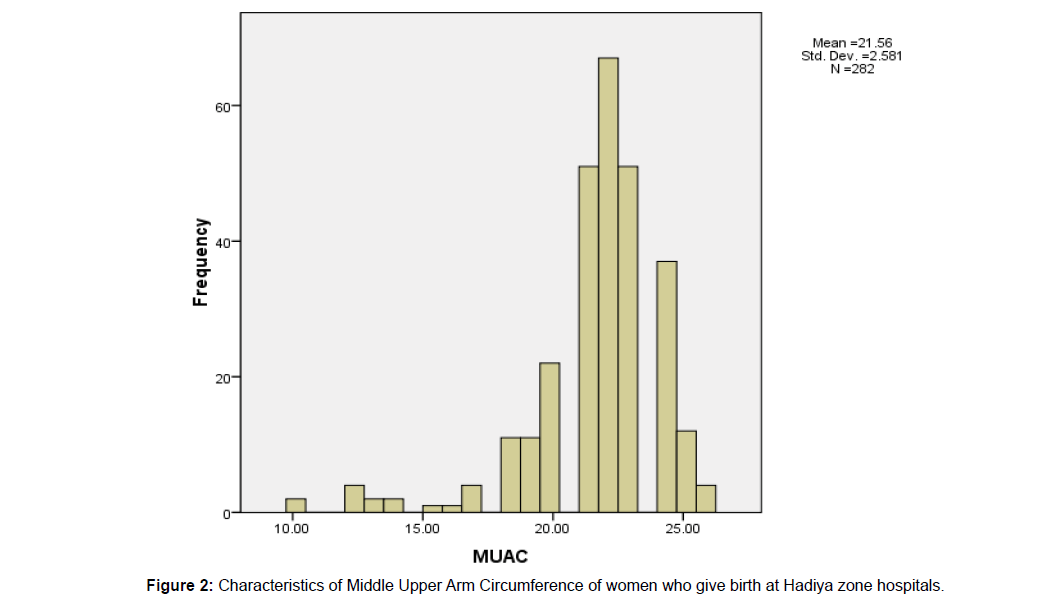
The mean and STD of MUAC of women who hand the neonate were 22.56 and 2.581, respectively (Figure 2).
Factors associated with low birth weight
Independent variables were identified during bivariate logistic regression analysis, which have p-value less than 0.05. Among these variable educational status, residence, ANC follow, iron intake, meal per day, additional meal, maternal gestational age and dietary diversity during pregnancy were crudely association with low birth weight (Table 3).
| Variables | Categories | Birth Weight | COR (95% CI) | P-value | |
|---|---|---|---|---|---|
| Normal Birth weight | Low birth weight | ||||
| Educational status | Not read and write | 36(65.5%) | 19(34.5%) | 4.105(1.687, 9.988) | 0.002 |
| Read and write | 67(82.7%) | 14(17.3%) | 1.625(0.660, 4.005) | 0.291 | |
| Primary | 59(88.1%) | 8(11.9%) | 1.055(0.383, 2.905) | 0.918 | |
| Secondary and above | 70(88.6%) | 9(11.4%) | 1 | - | |
| Residence | Urban | 77(77.8%) | 22(22.2%) | 1 | - |
| Rural | 155(84.7%) | 28(15.3%) | 1.582(0.849,2.945) | 0.148 | |
| ANC follow | Yes | 221(83.4%) | 44(16.6%) | 0.365(0.128, 1.039) | 0.059 |
| No | 11(64.7%) | 6(35.3%) | 1 | - | |
| Iron intake | Yes | 159(81.1%) | 37(18.9%) | 1 | - |
| No | 71(88.8%) | 9(11.2%) | 0.545(0.250, 1.189) | 0.127 | |
| Meal per day | 01 Feb | 3(33.3%) | 6(66.7%) | 15.500(3.227, 74.455) | 0.001 |
| 02 Mar | 13(68.4%) | 6(31.6%) | 3.577(1.061, 12.064) | 0.04 | |
| 3 | 154(83.7%) | 30(16.3%) | 1.510(0.656, 3.475) | 0.333 | |
| 4 and above | 62(88.6%) | 8(11.4%) | 1 | - | |
| Additional meal | Yes | 177(87.6%) | 25(12.4%) | 1 | - |
| No | 55(68.8%) | 25(31.2%) | 3.218 (1.711, 6.052) | 0 | |
| Maternal gestational age | less than 37 weeks | 17(47.2%) | 19(52.8%) | 17.882(5.861, 54.564) | 0 |
| 37-42 weeks | 135(83.9%) | 26(16.1%) | 3.081(1.138, 8.345) | 0.027 | |
| above 42 weeks | 80(94.1%) | 5(5.9%) | 1 | - | |
| Dietary advice during pregnancy | Yes | 215(84.3%) | 40(15.7%) | 0.316(0.135, 0.741) | 0.008 |
| No | 17(63.0%) | 10(37.0%) | 1 | - | |
Table 3: Bivariate analysis of LBW and associated factors in Hadiya Zone public hospitals.
Predictors of low birth weight
All variables with p-value less than 0.05 during bivariate analysis were entered into multiple logistic regression analysis. The variables with p- value less than 0.05 in multivariate analysis were considered as statistically significant in the study. The variables, which significantly predict low birth weight, were maternal gestational age, meal pattern and additional food during pregnancy.
The result showed that the likelihood of low birth weight was nearly 15 times higher in maternal gestational age less than 37 weeks as compared to maternal gestational age above 42 weeks (AOR: 14.978 95%, CI 4.685, 47.887). Those pregnant mothers who not eat additional meals during pregnancy were 3.226 times more likely to have low birth weight than those who eat additional meals during pregnancy (AOR: 3.226 95%, CI 1.556, 6.686). Those mothers who had irregular meal pattern were 2 times more likely to have low birth weight compared to regular meal pattern (AOR: 2.078 (1.034, 5.634) (Table 4).
| Variables | Categories | COR(95% CI) | AOR(95% CI) | P-value |
|---|---|---|---|---|
| Maternal gestational age | less than 37 weeks | 17.882(5.861, 54.564) | 14.978(4.685, 47.887) | <0.001** |
| 37-42 weeks | 3.081(1.138, 8.345) | 2.463(0.889, 6.826) | 0.083 | |
| above 42 weeks | 1 | 1 | - | |
| Additional meal | Yes | 1 | 1 | - |
| No | 3.218(1.711, 6.052) | 3.226(1.556, 6.686) | 0.002* | |
| Educational status | Not educated | 1 | 1 | 1 |
| Educated | 1.055(0.383, 2.905) | 1.162(0.631,3.734) | 0.802 | |
| Residence | Rural | 1.582(0.849,2.945) | 1.004(0.449,2.247) | 0.992 |
| Urban | 1 | 1 | - | |
| ANC | Yes | 0.365(0.128, 1.039) | 0.399(0.037,4.28) | 0.448 |
| No | 1 | - | - | |
| Iron intake | Yes | 0.365(0.128, 1.039) | 0.538(0.212,1.369) | 0.193 |
| No | 1 | - | - | |
| Dietary advice | Yes | 0.316(0.135, 0.741) | 0.728(0.146,3.631) | 0.699 |
| No | 1 | - | - | |
| Pattern of meal | Regular | 1 | - | - |
| Irregular | 3.218(1.711, 6.052) | 2.078(1.034,5.634) | 0.052* |
Note: * statistically significant association in multivariate analysis, ** highly statistically significant and “1” reference group.
Table 4: Multivariable analysis to factors associated with low birth weight in public hospitals in Hadiya zone, 2019.
Discussion
In this particular study the prevalence of low birth weight was 17.4% and in the multivariate logistic regression model mother without additional food, preterm gestational age and meal pattern were characteristics to predict for low birth weight.
Low birth weight observed in this study was highest than studies conducted in Jimma which was 11.02 % and 2011 EDHS report in which country level LBW was 11% and study done in Laelay Maichew and Axum district in Tigray which was 6.6% and 9.9% respectively [18,23]. This study finding is also higher than, Eastern & South Africa 11%, West and Central Africa 14%, East Asia 6%, Latin America 9%, least developed Countries 13%, East Africa 6%, Sub Sahara Africa 13% [12]. In the same way the prevalence of low birth weight is twofold higher than the study conducted in Jima medical Center. As well as the prevalence of low birth weight in Hadiya Zone was little bit higher than EDHS 2016(CSA, 2017) of national low birth survey result of 14%. In the way my research low birth weight prevalence was higher than the study done in Keniya of 12.3%.
The possible explanation highest might be the difference in geographical variation, food security and self-sufficiency, nutritional status mother, health service utilization. But it had relatively lower prevalence when compared with study finding done in India, Uttar Pradesh which was about 40% and study conducted in Kersa Demographic And Surveillance And Health Research Center (KDSHRC) which showed an incidence of 28.3% [22,24]. The possible explanation for the decrement in LBW in the current study might be the study done in Kersa was done in rural area. The other explanation might be due to variation in characteristics of study population like nutritional status and maternal feeding habit. This study indicated a significant difference among urban and rural resident mothers with regard to delivering low birth weight baby. Mothers who reside in rural were 1.6 times higher odds of delivering low birth weight baby compared to urban residents COR: 1.6, 95%CI (0.849,2.945).
This result is in line with studies done at three zonal hospitals in central Tigiray [18]. A possible reason would be, people in rural live a life characterized by greater hardship due to low infrastructures, information and nutritional awareness, harder physical work and less access to basic services were more prominent than the urban once.
A study conducted in three hospitals in Mexico City shows that SES (AOR, 2.19, 95% CI, 1.18-4.07) and Northwest Ethiopia shows female newborns higher odds of LBW than males [23]. However in may study meal pattern (AOR: 2.078 (1.034, 5.634), additional meal (AOR: 3.226 95%, CI 1.556, 6.686), preterm gestational age (AOR: 14.978 95%, CI 4.685, 47.887) were statistical associated. This indicate still other variable can be risk factor for low birth weight.
Conclusion and Recommendations
Conclusion
The prevalence of low birth weight in this study was high. Being rural resident, absence of nutritional counseling at ANC, low frequency of meal, low additional food during pregnancy, incomplete ANC follow, preterm gestational age and meal pattern were statistical associated with low birth weight?
Recommendations
• Based on the study finding the following recommendations go to health professionals working Antenatal care unites and to the Hospital facilities, Zonal health department and regional health bureau. As seen on this study the prevalence of low birth weight is high.
• Health service providers need to provide health information and counselling for all pregnant women attending for antenatal care.
• All health facilities in addition to nutritional counselling should provide and strengthen strategy of nutritional assessment of women during ANC and providing interventions accordingly.
• The Zone hospitals and office should strengthening efforts on availability of basic health services and promoting education on nutrition during pregnancy especially at rural areas. Regional health office and country at large should avail and strengthen appropriate neonatal, post- neonatal Intensive Care Unit and nutritional rehabilitation unit.
To sum up there should be integrated approach in fulfilling the gap of food self-sufficiency and security in house hold level, accessible and quality of health care. And also especial attention should be given on malnutrition management among pregnant mothers, intrauterine growth monitoring and management approach to mitigate premature at all health facilities.
References
- WHO/UNICEF (2014) Low birth weight: Country, regional and global estimates. UNICEF, New York.
- Gagan A, Kapil G, Vijay K, Parul G, Garg M, et al. (2012) Maternal risk factors associated with low birth weight neonates in a tertiary care hospital, Northern India. J Commun Med Health Educ 2: 177-180.
- Nekatibeb G (2007) Analysis of birth weight in Metu Karl hospital: South West Ethiopia. Ethiop Med J 45: 195-202.
- Collins JWDR, Handler A, Wall S, Andes S (2004) Very low birth weight in African American infants. The role of maternal exposure to interpersonal racial discrimination. Am J Public Health 94: 2132-2138.
- Siza J (2008) Risk factors associated with low birth weight of neonates among pregnant women attending a referral hospital in northern Tanzania. Tanzan J Health Res 10: 1-8.
- Stein RE, Siegel MJ, Bauman LJ (2006) Are children of moderately low birth weight at increased risk for poor health? A new look at an old question. Pediatrics 118: 217-223.
- Zeleke BM, Zelalem M, Mohammed N (2012) Incidence and correlates of low birth weight at a referral hospital in Northwest Ethiopia. Pan Afr Med J 12: 4.
- Walter EC, Ehlenbach WJ, Hotchkin DL, Chien JW, Koepsell TD (2009) Low birth weight and respiratory disease in adulthood: A population-based case-control study. Am J Respir Crit Care Med 180: 176-180.
- Ramakrishnan U (2004) Nutrition and low birth weight: From research to practice. Am J Clin Nutr 79: 17-21.
- Andersson R, Bergström S (1997) Maternal nutrition and socioâ€economic status as determinants of birthweight in chronically malnourished African women. Trop Med Int Health 2: 1080-1087.
- Badshah S, Mason L, McKelvie K, Payne R, Lisboa PJ (2008) Risk factors for low birthweight in the public-hospitals at Peshawar, NWFP-Pakistan. BMC Public Health 8: 197.
- WHSQ (1980) The incidence of low birth weight. World Health Stat Q 33: 197-224.
- Tema T (2006) Prevalence and determinants of low birth weight in Jimma Zone, Southwest Ethiopia. East Afr Med J 83: 366-371.
- Assefa BT, Enquoslassie F, Yusuf L (2010) Birth to pregnancy interval and its effect on perinatal outcomes in Addis Ababa, Ethiopia. Ethiopian J Reprod Health 4: 17.
- Gebremariam A (2005) Factors predisposing to low birth weight in Jimma Hospital south western Ethiopia. East Afr Med J 82: 554-558.
- Betew W, Muluneh EK (2014) Determinants of low birth weight among children aged 0 to 59 months in Ethiopia. Int J Pure Appl Sci Technol 25: 14-25.
- UNSSCN (2013) The Sixth report on the world nutrition situation: Incidence of low birth weight: Results from repeated national estimates (1997-2007). Pp: 54-57.
- Alemu T, Umeta M (2015) Prevalence and determinants of small size babies in Ethiopia: Results from in-depth analyses of the Ethiopian demographic and health survey-2011. Fam Med Med Sci Res 4: 243-250.
- Francis MR, Rakesh P, Mohan VR, Balraj V, George K (2012) Examining spatial patterns in the distribution of Low Birth Weight babies in Southern India-the role of maternal, socio-economic and environmental factors. Int J Biol Med Res 3: 1255-1259.
- Teklehaimanot N, Hailu T, Assefa H (2014) Prevalence and factors associated with low birth weight in axum and laelay maichew districts, North Ethiopia: A comparative cross sectional study. Int J Nutr Food Sci 3: 560-566.
- Assefa N, Berhane Y, Worku A (2012) Wealth status, Mid Upper Arm Circumference (MUAC) and Antenatal Care (ANC) are determinants for low birth weight in Kersa, Ethiopia. PloS one 7: e39957.
- Bugssa G, Dessalegn B, Dimtsu B, Berhane Y (2015) Prevalence and factors associated with HIV and hepatitis B virus infections among female commercial sex workers in Mekelle, Ethiopia: Cross sectional study. Int J Pharm Sci Res 6: 135.
- Torres-Arreola LP, Constantino-Casas P, Flores-Hernández S, Villa-Barragán JP, Rendón-MacÃas E (2005) Socioeconomic factors and low birth weight in Mexico. BMC Public Health 5: 20.
- Kader M, Perera NKP (2014) Socio-economic and nutritional determinants of low birth weight in India. N Am J Med Sci 6: 302-308.
Citation: Mengistu N, Daniel D, Gudina E (2020) Prevalence and Associated Factors of Low Birth Weight among Newborns Delivered at Public Hospital, in Hadiya Zone, Ethiopia. J Preg Child Health 7: 427. DOI: 10.4172/2376-127X.1000427
Copyright: © 2020 Mengistu N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2773
- [From(publication date): 0-2020 - Apr 05, 2025]
- Breakdown by view type
- HTML page views: 1823
- PDF downloads: 950