Prevalence and Associated Factors of Hepatitis B Virus Infection among Blood Donors in Debre Markos Blood Bank Centre, Northwest Ethiopia, 2018
Received: 19-Nov-2018 / Accepted Date: 10-Dec-2018 / Published Date: 18-Dec-2018 DOI: 10.4172/2161-1165.1000363
Abstract
Background: Despite the fact that Hepatitis B Virus infection has been a major problem associated with blood transfusion in developing countries like Ethiopia, data on magnitude of Hepatitis B Virus seropositivity among blood donors is scarce. This study aimed to assess the prevalence and associated factors of Hepatitis B Virus infection among blood donors at Debre Markos blood bank centre.
Methods: The study followed a facility based cross sectional study design among 403 consecutively selected volunteer blood donors. After having informed consent, from each donor, 5 ml venous blood samples were collected. Samples were tested for hepatitis B virus antigen with Enzyme Linked Immuno Sorbent Assay. The data entered in Epi-info version 7 and analyzed in SPSS Version 22. The proportions and averages of the study variables were calculated. Odds Ratios, 95% confidence intervals, and p-value of 0.05 in multiple variable logistic regressions used to identify significantly associated factors with Hepatitis B virus infection.
Results: About 403 volunteer blood donors with a mean age of 20 ± 2.35 years were included in the study. About 4.7% (n=19) were positive for hepatitis B surface antigen. The odds of hepatitis B virus infection among blood donors who had sharp materials sharing experience were 3 times higher than those who had no such experience [AOR =3; 95% CI: 1.07-8.3]. Blood donors who had history of tooth extraction were 5.2 times more likely acquire hepatitis B virus infection than those who had no such history [AOR=5.2; 95% CI: 1.54-17.47].
Conclusion: This study found that blood donors had intermediate prevalence of hepatitis B virus infections. In addition, sharing sharp materials and tooth extraction were identified the most important risk factors for hepatitis B virus infection. Before donation, volunteers must be strictly screened and health education about its modes of transmission must be given.
Keywords: Hepatitis B virus; Infection; Prevalence; Associated factors; Blood donors; Ethiopia
Background
Viral hepatitis is an inflammation of the liver a major health problem worldwide and cause acute or chronic hepatitis, which can leads to the development of extensive liver scarring (cirrhosis), liver failure, liver cancer, and death. It is the tenth leading cause of death and the leading cause of liver cancer worldwide. Chronic hepatitis B accounts for 60-80% of the world cases of primary liver cancer [1].
The World Health Organization (WHO) and the United States (U.S) Centers for Disease Control (CDC) estimate that over 500 million people are currently living with chronic viral hepatitis. Every year, nearly one million die from hepatitis. An estimated 57% of liver cirrhosis and 78% primary liver cancer cases are due to hepatitis B or C virus infections. In Africa, the burden of viral hepatitis is significantly high [2].
The world’s one-third population had HBV infection, of which a 360 million people are chronic carriers and 5-7 hundred thousand people die every year. Africa with the second largest number of chronic carriers next to Asia, considered a high endemic region. In Kenya and Ethiopia more than 60% of chronic liver diseases and up to 80% of hepatocellular cancers are due to chronic HBV infections [3]. The prevalence of HBV is 8% in West Africa and 5-7% in other parts of Africa. Nearly 70–95% of the adult population in Africa had past exposure to HBV infection with seroprevalence of 6–20% [4].
Hepatitis B virus infection is a public health problem and a major cause of morbidity and mortality particularly in developing countries. The world can be divided into three areas where the prevalence of chronic HBV infection is: high (>8%), intermediate (2-8%), and low (<2%). Most countries are still considered intermediate to high endemicity for HBV infection [5].
Evidences showed that blood transfusion saved millions of lives each year. It is an important therapy during maternal bleeding, surgery and a lifesaving procedure for anemic patients. However, it has associated major problems including transfusion transmitted infections since a number of viruses, bacteria and parasites can be transmitted through blood or its products like hepatitis B virus (HBV) [6]. Hence, a safe blood is a critical component of health care to prevent the spread of blood borne infectious diseases, despite the fact, general lack of quality systems, poor laboratory procedures, inadequate donated blood testing, inappropriate use of blood and blood components contribute for unsafe blood transfusion services [7].
The hepatitis B virus infection is 50–100 times more contagious than HIV. Many of the carriers do not realize that they have infected with the virus rendering it as a “silent killer” [8]. The infection can transmitted vertically at birth, horizontally through unprotected sex, sharing of injecting equipment and close contact to infants and neonates. Transmission through unscreened blood products is another route of transmission since blood remains infectious for several weeks even when dried [9]. In Sub-Saharan Africa, 12.5% of patients who receive blood transfusion are at risk of post-transfusion hepatitis [10]. The World Health Organization (WHO) estimated that transfusion of unsafe blood accounted for 8 to 16 million hepatitis B virus infections each year. In sub-Saharan Africa, more than 45,000 hepatitis B virus infections are due to contaminated transfusions annually [11]. A study conducted among migrants in Italy reported 6% prevalence of HBV infection [12]. Another study from Pakistan reported 3.17% prevalence among high risk groups [13] and 1.9% in Karachi [14]. It was 0.58% in Bahrain with blood transfusion, dental procedures and surgical operations accounted for 24.6%, 37.2% and 35.6% route sources of infection respectively [15]. Similarly, it was 0.58% in Tiruchirappalli among voluntary blood donors [16], 3.51% in Gwilar, India [17] and 0.11% among blood donors in Mexico [18]. Another study conducted in Brazil showed that male gender, schooling <4 years, no stable relationships, and previous acupuncture therapy were risk factors of HBV infection [19]. A study conducted in Delhi reported that injection was a highly significant risk factor for HBV [20].
A study from Kenya reported 3.8% prevalence of HBV infection among pregnant women and 4.3% among 20-24 years old [21]. In Libya the prevalence was 2.2% with a significantly higher rate among males (2.6%) than females (1.8%) and 44% lower risk of infection among vaccinated [22]. In Burkina Faso, it was 13.4% and 2.4% for first-time and repeat donors respectively [23]. The prevalence of HBV infection was 10.79% in voluntary blood donors and 11.59% in replacement blood donors in Ghana [24] and 4.2% in Sudan among blood donors [25]. In Kenya patients who had undergone dental surgery had 3.3 times more risk than patients who had not [26]. A study done in Morocco reported that age, male gender, Dental procedure history, use of glass syringes, history of jaundice and sexual risk behaviors were risk factors of HBV infection [27]. Another study done in Nigeria showed that Circumcision, scarification/tattooing/ and past surgeries were risk factors of hepatitis B virus infection [28].
In Ethiopia, a study from Addis Ababa reported that the prevalence of HBV infection was 5.4% among pregnant women, 40.1% of which were in 25-29 years age group and the HBV infection prevalence was higher above 20 years of age, history of abortion, Surgery and family history of hepatitis [29]. It was 3.05% in Southwest Ethiopia, Jimma [30], 6.9% among adults attending ART clinic in Hawassa University Referral Hospital. It also indicated that the prevalence was 7.5% in age group of 18-24, 8.2% in 25-34 and 4.8% for above 34 years old [31]. It was reported to be 10.9% among blood donors in Jijiga [32], 9.5% among voluntary blood donors in Wolaita Sodo [33], 4.7% among blood donors in Arba Minch blood bank [34] and 3.6% in North Gondar district blood bank indicating farmer, employed, and unemployed donors were at a higher risk of HBV infection compared to student donors [35]. A study done in Dire Dawa among blood donors showed that the most important risk factors of HBV infections were male sex and age group 33-40 [36]. Another study from Mekelle hospital among HIV positive individuals reported that male, multiple sexual partner and CD4 count <200 cells/μl were significantly associated with HBsAg positivity [37]. A study from Bahir Dar among pregnant women showed that history of blood transfusion, body tattooing, previous history of surgery and unsafe injection were risk factors for HBV infections [38]. Sharing of sharp materials was significantly associated with HBV infection [39] and tooth extraction was the other strong predictor of Hepatitis B infection [40,41]. Many researchers have investigated prevalence rates of HBV infections in various groups. However, most studies conducted in Ethiopia among blood donors are retrospective and does not include all personal factors. Therefore, this study tried to determine the prevalence and identify associated factors of HBV infection among blood donors.
Methods
Study design
A facility based cross-sectional survey design was employed to assess the prevalence and associated factors of Hepatitis B virus infection among blood donors at Debre Markos blood bank center, Northwest Ethiopia 2018. This study design considered appropriate for the objective, as its main intention was to determine the prevalence of HBV infection and identify its associated factors simultaneously at single-point data collection period of March to April 2018 for the study.
Study setting
The study was conducted in Amhara Region, Ethiopia, at Debre Markos blood bank center. Debre Markos blood bank center, which is located in “Debre Markos city”, 299 km North West of Addis Ababa. The study blood bank centre screens HIV, HBV, HCV, and syphilis. The blood bank mainly provides services for 10 hospitals found under East Gojjam Zone. The blood bank collected 4524 unit of blood from voluntary blood donors in 2017/18. The study was conducted from March- April 2018.
Population and sample
The source population was all potential donors who visited Debre Markos blood bank centre, while all blood donors who attended the blood bank during the study period and who were eligible to donate blood were the study population. Sample size was determined using single population proportion formula considering 9.5% prevalence of hepatitis B virus infection in Wolaita Sodo University Teaching Referral Hospital with a 95% level of confidence and 3% margin of error and 10% nonresponse rate as follows:
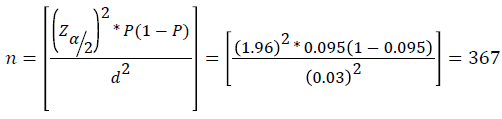
By adding 10% non-response rate to the larger sample size (367), the final sample size was 403.
Eligibility criteria
All individuals who fulfilled the national and regional blood bank criteria were included. Some of these criteria’s include:
• Age 18-65 years
• Weight; at least 45 Kg, Pulse 60-100 per minute, Blood pressure systolic 120-129 mmHg and diastolic 80-89 mmHg, Hemoglobin 12.5 g/dl for females and 13.5 g/dl for males
• Frequency of donation: For whole blood donors 12 weeks for males and 16 weeks for females, For platelet donors four weeks and For plasma donors two weeks
• Fluid intake and food; donors should maintain their usual food and fluid intake
• Pregnancy, lactation and menstruation: Donors defer during pregnancy and up to six months after delivery
• Donor’s medical history: assessed and free of Non-communicable disease and for Medical and surgical interventions.
Sampling procedure
All donors prospectively recruited in the study and samples were selected consecutively during the data collection period to take the first 403 blood donors which were eligible for donation.
Study variables
The dependent variable was HBV infection (Yes/No). The independent variables includes: Socio-demographic factors (Age, Sex, Marital status, Type of Blood group, Occupation, Educational status); Behavioral factors (Have multiple sex partners, Intravenous drug use, Tattooing practice, Alcohol use, Condom use, Sharing sharp materials, Sharing tooth brush, Smoking history) and Clinical factors (Previous transfusion, Type of donation, Previous surgery, Tooth extraction, Hospital admission).
Operational definitions
• Hepatitis B Surface Antigen (HBsAg) - is an antigen on the surface of the virus. Its presence indicates either acute or chronic infection.
• Hepatitis B surface antigen seropositivity- the detection of HBsAg in serum or plasma using a gold standard method Enzyme Linked Immuno Sorbent Assay (ELISA).
Data collection procedures
Prior to blood collection, the donors were requested to answer a questionnaire to determine whether they are eligible for donation per the criteria set by the National Red Cross Society (NRCS) and by study area blood bank. Pre-tested semi structured Standard data collection tool was prepared for both independent and dependent variables. Two trained and oriented blood bank workers collected the data.
Specimen collection and processing
After obtaining informed consent, 5 ml of venous blood was collected in plane tubes under aseptic conditions from peripheral vein by experienced laboratory personnel from all consenting blood donors consecutively. These tubes were labeled with unique identification number and processed at the time of collection. The blood samples taken from the individuals were centrifuged at 3000 revolution per minute (RPM) for at least 20 minutes at room temperature and the serum was separated and placed in nun tubes and kept frozen at -20°C until to be tested.
Laboratory testing
All the serum samples were tested for HBsAg by using a gold standard method ELISA following standard operating procedures [42]. The subjects’ positive for HBsAg were referred to the attending physician for further diagnosis and treatment. The HBsAg EIA is a solid-phase simultaneous sandwich immunoassay, which employs monoclonal antibodies and polyclonal antibodies specific for HBsAg. Micro titters well were coated with monoclonal antibodies specific for HBsAg. A Serum specimen was added to the antibody coated micro titter wells together with Enzyme conjugated polyclonal antibodies. HBsAg, if present, would form an antibody-HBs Ag-antibody-enzyme complex. The plate was then washed to remove unbound material. Finally, a solution of substrate was added to the wells and incubated. A blue color was developed in proportion to the amount of HBsAg present in the specimen. The enzyme-substrate reaction was stopped and the result visualized by naked eye or read by EIA plate reader for absorbance at the wavelength of 450 nm.
Data quality control
The questionnaire was prepared in English and translated back to Amharic, translating back to English to ensure consistency of the questions. Pre-testing of 5% the questionnaire was done prior to the study. The clarity, understand ability and flow of each question and the time to fill the questionnaire were assessed and found satisfactory. Daily all the collected data were checked for completeness by the principal investigator. Quality control of serological test, Known positive and negative controls were run in parallel with test samples. All laboratory procedures were carried out following standard operating procedures (SOPs). The quality assurances of pre-analytical, analytical, and post-analytical stages were applied.
Pre-analytical stage
Blood samples were collected aseptically from blood donors and properly labeled with the patient identification number. Trained Laboratory personnel collected the specimen. The samples were centrifuged; the serum was evaluated and separated; appropriately and stored until transported to the laboratory. The transported samples were stored at the optimum temperature until they were processed.
Analytical stage
Trained laboratory personnel in Hema diagnosis laboratory performed the test with Huma reader and Washer (Human, Germany). The reagents and the test method were assessed with a known positive and negative control materials, the standard laboratory procedures were also followed, and the supervisors checked the results.
Post-analytical stage
The results were recorded with the patients’ identification number, in order to avoid the errors in the results of the test, repeatedly checked before reporting.
Data processing and analysis
The collected data from the questionnaire were entered and cleaned using Epi-info version 7 and analyzed by SPSS version 22. Frequency, percentage, and mean were used for data description. Tables and figures were used to present the data. Both bivariable and multivariable binary logistic regression were used to identify possible factors associated with the outcome. Adjusted odds ratio with its 95% confidence interval and p-value less than or equal to 0.05 were used to report the statically significant explanatory variables.
Results
Socio-demographic characteristics
About 403 blood donors were screened during the study period of which 67% (n=270) were males and 33% (n=133) were females. The minimum participant’s age was 18 and maximum was 42 years old with a range of 24 years. The majority (75.9%, n=306) of donors were in the age group of 18-20 years and all were voluntary donors.
Regarding the types of blood group profile of the participants, about 40.9% (n=165) had blood group O, 31.5% (n=127) A, 20.6% (n=83) B and 6.9% (n=28) had AB. With respect to the Rh factor, most (95.1%, n=383) participants were found RH positive. The majority (66.7 %, n=269) of the study participants had a Secondary level of educational status, the rest 30.8% (n=124) and 2.5% (n=10) had either a College/ above and a Primary level of educational status respectively (Table 1).
| Characteristics | Frequency | Percent |
|---|---|---|
| Age Group | ||
| 18-20 | 306 | 75.9 |
| 21-25 | 88 | 21.8 |
| ≥ 26 | 9 | 2.2 |
| Sex | ||
| Male | 270 | 67 |
| Female | 133 | 33 |
| Marital status | ||
| Single | 371 | 92.1 |
| Married | 31 | 7.7 |
| Divorced | 1 | 0.2 |
| Educational status | ||
| Primary | 10 | 2.5 |
| Secondary | 269 | 66.7 |
| College and above | 124 | 30.8 |
| ABO (blood group) | ||
| A | 127 | 31.5 |
| B | 83 | 20.6 |
| AB | 28 | 6.9 |
| O | 165 | 40.9 |
| RH | ||
| Positive | 383 | 95.1 |
| Negative | 20 | 4.9 |
Table 1: Socio demographic characteristics of study participants in Debremarkos Blood Bank Center, East Gojjam Zone, Amhara Regional State, Ethiopia 2018.
Prevalence of hepatitis B virus infection
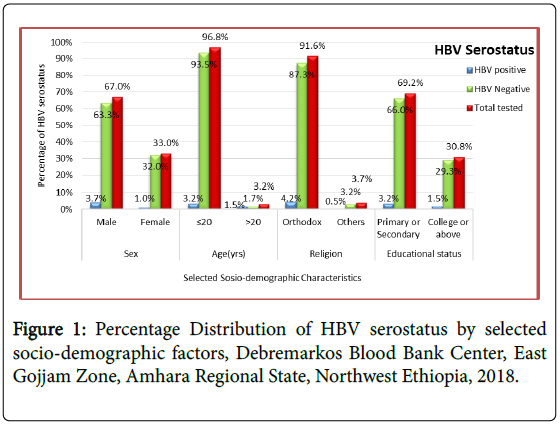
About 4.7% (n=19) study participants were found positive for HBV infection. The males seropositivity was 3.7% (n=15) and females was 1% (n=4). About 3.2% (n=13) of positive results for HBV infection were in the age group of 18-20 years. About 3.2% (n=13) HBV seropositive was found in those participants who had primary or secondary level of education (Figure 1).
Factors associated with Hepatitis B virus infection
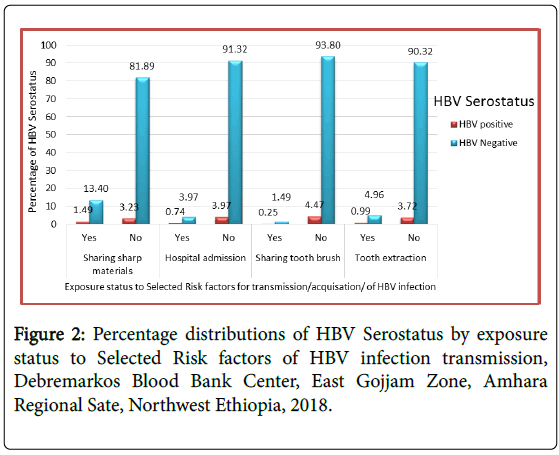
About 2.7% (n=11) of the study participants had history of contact with Jaundice patient, none of them however, were positive for hepatitis B virus infection. About 9.43% (n=38) of the study participants had the experience of cigarette smoking, of which 0.74%) (n=3) were positive for HBV and the rest 3.97% (n=16) of the blood donors who were seropositive for HBV infection had no such experience. About 5.96% (n=24) blood donors had history of tooth extraction, of which 1% (n=4) were seropositive for HBV infection.
About 14.89% (n=60) had history of sharing sharp materials, of which 1.49% (n=6) were HBV positive. Around 14.64% (n=59) of the study participants had a history of unsafe injection, of which 1.49% (n=6) were positive for hepatitis B virus infection. Similarly, 23.6% (n=95) of the study participants had awareness on HBV transmission, prevention and treatment, of which 1.24% (n=5) were positive for HBV infection and the rest 3.47% (n=14) who were seropositive had no the awareness on HBV transmission, prevention and treatment (Figure 2 and Table 2).
| Risk factors of HBV infection | HBV positive | HBV Negative | Total tested | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Vaccination | Yes | 0 | 0 | 13 | 3.23 | 13 | 3.23 |
| No | 19 | 4.71 | 371 | 92.06 | 390 | 96.77 | |
| Contact with Jaundice patient | Yes | 0 | 0 | 11 | 2.73 | 11 | 2.73 |
| No | 19 | 4.71 | 373 | 92.56 | 392 | 97.27 | |
| Unsafe injection | Yes | 6 | 1.49 | 53 | 13.15 | 59 | 14.64 |
| No | 13 | 3.23 | 331 | 82.13 | 344 | 85.36 | |
| Body tattoo | Yes | 7 | 1.74 | 65 | 16.13 | 72 | 17.87 |
| No | 12 | 2.98 | 319 | 79.16 | 331 | 82.13 | |
| More than one sexual partner | Yes | 0 | 0 | 11 | 2.73 | 11 | 2.73 |
| No | 19 | 4.71 | 373 | 92.56 | 392 | 97.27 | |
| Smoking | Yes | 3 | 0.74 | 35 | 8.68 | 38 | 9.43 |
| No | 16 | 3.97 | 349 | 86.6 | 365 | 90.57 | |
| Know about disease transmission & prevention | Yes | 5 | 1.24 | 90 | 22.33 | 95 | 23.57 |
| No | 14 | 3.47 | 294 | 72.95 | 308 | 76.43 | |
Table 2: Distribution of factors associated with Hepatitis B virus infection among study participants, Debre Markos Blood Bank Center, East Gojjam Zone, Amhara, March-April 2018.
Bivariate and multivariate analysis of HBV infection determinant factors
Socio demographic and other determinants in relation to hepatitis B virus infection of the blood donors were evaluate by bivariate and multivariate binary logistic regression analysis model. In the bivariate models, almost no socio-demographic variables and majority of the assumed risk factors were significantly associated with hepatitis B virus infection. In this model unsafe injection, sharing of sharp materials, history of tooth extraction, body tattooing and hospital admission were determinants, which were found significantly associated with hepatitis B virus infection. The factors were then transferred to the final models to see the effect of each factor on the dependent variable. Those blood donors who had an experience of sharing sharp materials were about 3 times (AOR=3; 95% CI: 1.07-8.3) at higher risk of hepatitis B seropositive compared to blood donors who had no such experience. Further blood donors who had history of tooth extractions were also about 5.2 times (AOR=5.2; 95% CI: 1.54-17.47) more risk compared to those who had no such experience (Table 3).
| Variables | HVB Serostatus | Total N (%) | COR (95%CI) | AOR (95%CI) | P-Value | |
|---|---|---|---|---|---|---|
| Positive n (%) | Negative n (%) | |||||
| Sex | ||||||
| Male | 15(78.95) | 255(66.41) | 270 (67) | 1 | - | - |
| Female | 4(21.05) | 129(33.59) | 133 (33) | 0.52(0.17-1.6) | ||
| Unsafe injection | ||||||
| Yes | 6(31.58) | 53(13.80) | 59(14.6) | 2.8(1.05-7.9) | 2.1(0.74-6.50) | 0.15 |
| No | 13(68.42) | 331(86.20) | 344(85.4) | 1 | ||
| Body tattoo | ||||||
| Yes | 7(36.84) | 65(16.93) | 72(17.9) | 2.86(1.08-7.54) | 2.4(0.84-7.08) | 0.09 |
| No | 12(63.16) | 319(83.07) | 331(82.1) | 1 | ||
| Smoking | ||||||
| Yes | 3(15.79) | 35(9.11) | 38(9.4) | 1.87(0.51-6.73) | - | - |
| No | 16(84.21) | 349(90.89) | 365(90.6) | 1 | ||
| Sharing sharp materials | ||||||
| Yes | 6(31.58) | 54(14.06) | 60(14.9) | 2.82(1.02-7.73) | 3(1.07-8.3) | 0.03 |
| No | 13(68.42) | 330(85.94) | 343(85.1) | 1 | ||
| Hospital admission | ||||||
| Yes | 3(15.79) | 16(4.17) | 19(4.7) | 4.3(1.14-16.3) | 3.9(0.86-17.83) | 0.07 |
| No | 16(84.21) | 368(95.83) | 384(95.3) | 1 | ||
| Sharing tooth brush | ||||||
| Yes | 1(5.26) | 6(1.56) | 7(1.7) | 3.5(0.4-30.6) | - | - |
| No | 18(94.74) | 378(98.44) | 396(98.3) | 1 | ||
| Tooth extraction | ||||||
| Yes | 4(21.05) | 20(5.21) | 24(6) | 4.8(1.47-15.97) | 5.2(1.54-17.47) | 0.009 |
| No | 15(78.95) | 364(94.79) | 379(94) | 1 | ||
Table 3: Bivariate and multivariate analysis results of associated factors of Hepatitis B virus infection at Debre Markos Blood Bank Center, East Gojjam Zone, Amhara, March-April 2018.
Discussion
Prevalence of hepatitis B virus infection
In this Facility based cross-sectional study, the prevalence of HBV among voluntary blood donors was determined. In this study, the overall prevalence of hepatitis B virus was found to be 4.7%. It was discussed that the world could be divided into three areas where the prevalence of chronic HBV infection is: high (>8%), intermediate (2-8%), and low (<2%). Most countries in the world are still considered intermediate to high endemicity for HBV infection [5]. This finding ensures that in the study setting epidemiology of HBV infection was intermediate level.
This, 4.7% prevalence of hepatitis B virus infection, finding was similar with a study done in Arba Minch blood bank centre (4.7%) [34]. However, it was lower than a study done in Jijiga blood bank centre (10.9%) [32] and Wolaita Sodo University Teaching Referral Hospital (9.5%) [33]. It was also lower than other countries’ reported prevalence; 10.79% in Ghana [24], 13.4% in Burkina Faso [23], 6% in Italy [12] and 5.6% in Kenya [21]. The inconsistencies might be due to the difference in the socio-demographic characteristics related to geographic area, study population considered, blood banks strategy focusing on voluntary blood donors and time when these studies were conducted.
On the other hand, our report is higher than the results of studies conducted in different parts of Ethiopia; 3.6% in Gondar blood bank [35], 3.73% in Dire Dawa blood bank [36] and 3.05% in Jimma blood bank [30]. Our data also indicate the higher prevalence of hepatitis B infection compared to the results from counties like Libya 2.2% [22], Sudan 4.2% [25], India 3.51% [17], Mexico 0.11% [18], Pakistan 1.9% [14] and Bahrain 0.58% [15]. These variations could also be due to actual changes in population risks or effectiveness of donor screening measures.
In this study, majority of the participants 67% (n=270) were males. This is always the case as far as blood donation is concerned and in similar studies earlier, males were majority of the donors [23,33]. This is again because women generally have low hemoglobin levels hence are mostly disqualified as blood donors. The prevalence of HBV based on sex was 5.6% in males and 3% in females. This difference might be due to Males dominated as blood donors compared to females in the study area. This finding of gender variation in prevalence was in line to the study conducted in Libya with a significantly higher rate of HBV infection among males (2.6%) than females (1.8%) [22].
In this study majority of the participants 75.9% (n=306) were in the age group of 18-20 years and 21.8% (n=88) were in the age group of 21-25 years old. The prevalence was lowest in the age group of 21-25 years, (1.5%). This finding was lower than a study done in Kenya 4.3% [21] and in Addis Ababa, Bishoftu General Hospital 5.6% [29]. This difference might be due to changes in population risks, as in this study majority of volunteer donors were high school and university students. Even though it is possible to find HBsAg test positivity in all age groups, this finding strongly supports the role of sexual transmission of HBV infection since high prevalence were at sexually active (fire stage) age group of 18-20 (3.2%).
From the bivariable and multivariable analysis, none of the sociodemographic variable was significantly associated with HBV infection. Sharing of sharp materials was significantly associated with HBV infection. Those having shared any sharp material were three times more likely to be infected with HBV infection than those who never share sharp materials. Consistent result was reported from Woldiya prison [41]. This may be related the fact that in our study since majority of the study participants 395 (98%) were students, where sharing of sharp materials with family members might be common.
Tooth extraction was the other strong predictor of Hepatitis B infection where blood donors who had history of tooth extraction were at increased risk of hepatitis infection [AOR=5.2, 95%CI: 1.54-17.47]. This is supported by bulk of literatures as indicated review by Mahboobi, et al. [42] and current report by Suliman M. Al Humayed [43]. As it had already mentioned on these study the increased risk of infection in individual who had the experience of tooth extraction might related to the fact that dental procedures often result in bleeding and exposure to infected body fluids that are known vehicles of infectious disease transmission.
Conclusion and Recommendations
This study showed that the prevalence of HBV infections among volunteer blood donors in Debre Markos Blood Bank center was 4.7%. History of tooth extraction and sharing of sharp materials were found to increase the risk of hepatitis B virus infection. We recommend that all volunteer blood donors must be strictly screened before donation. Since High schools and universities were a large pool of volunteer donors, health education about the disease and its modes of transmission must be given in these sites. In addition, health education must be specifically given to seropositive individuals to halt the transmission. Efforts are also required for introducing free vaccination against HBV to high-risk groups. Further, there is a need for community based HBV infection study for further investigate the risk factors, which are crucial to implement effective prevention program of HBV infection.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from ethical review committee of Bahir Dar University, College of Medicine and Health Sciences, School of Public Health and Department of Biostatistics and Epidemiology. During data collection, brief explanation was given about the objective and significance of the study to each participant in order to obtain verbal consent. Respondents were not identified by their name and the participant had the right to discontinue the participation at any time. Official letter was given for concerned bodies and Permission letter was taken from Debre Markos blood bank center administration office. Confidentiality of the information was assured from all the data collectors and principal investigators side. Participants having positive result were referred to nearby health facilities for further diagnosis and treatment.
Consent for publication
Consent for publication is not applicable- this study did not take individual person’s detail such as name, images, or videos.
Availability of data and material
All the data generated or analyzed during this study are included in this published article.
Competing interests
The authors declare that we have no competing interests.
Funding
There was no external funding for this paper.
Authors' contributions
Yeneanchalem Bialfew wrote the proposal, participated in data collection, and analyzed the data. Getachew Hailu and Tsion Samuel approved the proposal with some revisions, and participated in data analysis. Getachew Hailu wrote the manuscript. We revised drafts of the paper. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledged to all selected study sites officials whom we have contacted and allowed us to conduct this project on their customers. Likewise, we are really thankful to all our respondents for their willingness for the interview. The authors also extend their special thanks for both data collectors and supervisors.
References
- Mekonnen A, Dasta K, Damtew E (2015) Prevalence of HBV, HCV and Associated Risk Factors Among Cleaners at Selected Public Health Centers in Addis Ababa, Ethiopia. International Journal of Basic and Applied Virology 4: 35-40.
- Bane A, Patil A, Khatib M (2014) Healthcare cost and access to care for viral hepatitis in Ethiopia. International Journal of Innovation and Applied Studies 9: 1718-1723.
- Girma A (2016) Assessment of Hepatitis B Seroprevalence and Associated Factors in Kality Prison Addis Ababa Ethiopia. AAU Institutional Repository.
- WHO (2017) Prevention & Control of Viral Hepatitis Infection: Framework for global action. World Health Organisation.
- Â Hou J, Liu Z, Gu F (2005) Epidemiology and Prevention of Hepatitis B Virus Infection. Int J Med Sci 2: 50-57.
- Bonja F, Hussein M, Alemu J, Gemechu D, Birhaneselassie M (2017) The prevalence of transfusion transmitted infections: A focus on hepatitis B virus among blood donors at Hawassa blood bankcenter, Southern Ethiopia. Int J Blood Transfus Immunohematol 7: 7-14.
- Bommanahalli B, Javali R, Swamy CMM, Gouda K, Siddartha K, et al. (2014) Seroprevalence of Hepatitis B and Hepatitis C viral infections among blood donors of central Karnataka, India. Int J Med Sci and Public Health 3: 272-275.
- Umare A, Seyoum B, Gobena T, Haile Mariyam T (2016) Hepatitis B Virus Infections and Associated Factors among Pregnant Women Attending Antenatal Care Clinic at Deder Hospital, Eastern Ethiopia. PLoS ONE 11: e0166936.
- Balew M, Moges F, Yismaw G, Chandrashekhar U (2014) Assessment of hepatitis B virus and hepatitis C virus infections and associated risk factors in HIV infected patients at Debretabor hospital, South Gondar, Northwest Ethiopia. Asian Pac J Trop Dis 4: 1-7.
- Bartonjo G (2013) Prevalence and factors associated with transfusion transmissible infections among blood donors at Regional blood transfusion center Nakuru and Tenwek Mission Hospital, Kenya.
- Mihertie H (2017) Hepatitis B is increasing in Ethiopian Blood Banks: A Mini Review. Adv Res Gastroentero Hepatol 6: 3.
- El-Hamad I, Pezzoli MC, Chiari E, Scarcella C, Vassallo F, et al. (2015) Point-of-Care Screening, Prevalence, and Risk Factors for Hepatitis B Infection Among 3,728 Mainly Undocumented Migrants From Non-EU Countries in Northern Italy. J Travel Med 22: 78-86.
- Memon AR, Shafique K, Memon A, Draz AU, Rauf MU, et al. (2012) Hepatitis B and C prevalence among the high risk groups of Pakistani population. A cross sectional study. Arch Public Health 70: 9.
- Irfan SM, Uddin J, Zaheer HA, Sultan S, Baig A (2013) Trends in Transfusion Transmitted Infections Among Re-placement Blood Donors in Karachi, Pakistan. Turk J Hematol 30: 163-167.
- Janahi EM (2014) Prevalence and Risk Factors of Hepatitis B Virus Infection in Bahrain, 2000 through 2010. PLoS ONE 9: 1-5.
- Bagiyalakshmi V, Elangovan RS (2017) Prevalence of Hepatitis B Virus Infection among Voluntary Blood Donors at a Tertiary Care Hospital Blood Bank -Tiruchirappalli. International Journal of Scientific Study 4: 10.
- Raietal S (2014) Transfusion Transmissible Infections among Blood Donors at the Blood Bank of Medical College of Gwalior: A 5 Year Study. International Blood Research 2: 235-246.
- Lopez-Balderas N, Bravo E, Camara M, Hernandez-Romano P (2015) Seroprevalence of hepatitis viruses and risk factors in blood donors of Veracruz, Mexico. J Infect Dev Ctries 9: 274-282.
- Machado DF, Martins T, Trevisol DJ (2013) Prevalence and Factors Associated with Hepatitis B Virus Infection among Senior Citizens in a Southern Brazilian City. Hepat Mon 13: e7874.
- Suryam V, Kathuria SR, Karunakaran S (2011) A study of seroprevalence of hepatitis B and hepatitis C among troops in Armed Forces. Med J Armed Forces India 67: 257-259.
- Ngaira JAM, Kimotho J, Mirigi I, Osman S, Ng’ang’a Z, et al. (2016) Prevalence, awareness and risk factors associated with Hepatitis B infection among pregnant women attending the antenatal clinic at Mbagathi District Hospital in Nairobi, Kenya. Pan Afr Med J 24: 315.
- Elzouki AN, Smeo MN, Sammud M, Elahmer O, Daw M, et al. (2013) Prevalence of hepatitis B and C virus infections and their related risk factors in Libya: a national seroepidemiological survey. East Mediterr Health J 19: 589-599.
- Nagalo BM, Bisseye C, Sanou M, Kienou K, Nebié YK (2012) Seroprevalence and incidence of transfusion-transmitted infectious diseases among blood donors from regional blood transfusion centers in Burkina Faso, West Africa. Trop Med Int Health 17: 247-253.
- Dongdem JT, Kampo S, Soyiri IN, Asebga PN, Ziem JB, et al. (2012) Prevalence of hepatitis B virus infection among blood donors at the Tamale Teaching Hospital, Ghana. BMC Res Notes 5: 115.
- Abdo AE, Mohammed DA, Satti M (2015) Prevalence of hepatitis B virus among blood donors and assessment of blood donor’s knowledge about HBV in Sudan. HIV/AIDS. Res Treat Open J 2: 76-80.
- Kang’ethe JM, Waihenya R, Gachuno O, Mutai K, Otieno M, et al. (2017) Prevalence and Associated Factors of HBV Infections among HI Infected HAART Receiving Mothers and their Exposed Infants in Nairobi, Kenya. J Hum Virol Retrovirol 5: 00167.
- Baha W, Foullous A, Dersi N, They-they TP, El alaoui K, et al. (2013) Prevalence and risk factors of hepatitis B and C virus infections among the general population and blood donors in Morocco. BMC Public Health 13: 50.
- Eke CB, Ogbodo SO, Ukoha OM. Ibekwe RC, Asinobi IN, et al. (2015) Seroprevalence and Risk Factors of Hepatitis B Virus Infection among Adolescents in Enugu. Journal of Tropical Pediatrics 61: 407-413.
- Desalegn Z, Mihret A, Beyene HB, Yilma M, Seid Y, et al. (2016) Survey of Hepatitis B virus infection and risk factors among pregnant women at public hospital in Ethiopia. International Journal of Biomedical Research 7: 450-456.
- Kebede W, Mekonnen Z, Abebe C, Mekonnen Z (2017) Transfusion transmissible infection surveillance among blood donors in Southwest Ethiopia: A six years retrospective study Asian Pac J Trop Dis 7: 156-161.
- Belayneh F (2015) Prevalence of Hepatitis B Virus Infection and Associated Factors among HIV Positive Adults Attending ART Clinic at Hawassa Referral Hospital, SNNPR, Ethiopia. Open Access Library Journal 2:1-7.
- Mohammed Y, Bekele A (2016) Seroprevalence of transfusion transmitted infection among blood donors at Jijiga blood bank, Eastern Ethiopia: retrospective 4 years study. BMC Res Notes 9: 129.
- Bisetegen FS, Bekele FB, Ageru TA, Wada FW (2016) Transfusion-Transmissible Infections among Voluntary Blood Donors at Wolaita Sodo University Teaching Referral Hospital, South Ethiopia. Canadian Journal of Infectious Diseases and Medical Microbiology 2016: 8254343.
- Kabato AA (2016) Prevalence and associated risk factors of Hepatitis B and Hepatitis C virus among volunteer blood donors in Arba Minch Blood Bank SNNPR, Ethiopia. Journal of Medical Laboratory and Diagnosis 7: 20-27.
- Belete B, Shiferaw E, Berhanu W, Kefyalew A, Melku M (2017) Transfusion-transmissible viral infections among blood donors at the North Gondar district blood bank, northwest Ethiopia A three year retrospective study. PLoS ONE 12: 7.
- Habte Y, Seyoum B, Alemayehu T (2016) Hepatitis B Virus Infection and Associated Factors among Blood Donors at Dire Dawa, Eastern Ethiopia. J Antivir Antiretrovir 8: 103-106.
- Weldemhret L, Asmelash T, Belodu R, Gebreegziabiher D (2016) Sero-prevalence of HBV and associated risk factors among HIV positive individuals attending ART clinic at Mekelle hospital, Tigray, Northern Ethiopia. AIDS Res Ther 13: 6.
- Zenebe Y, Mulu W, Yimer M, Abera B (2014) Sero-prevalence and risk factors of hepatitis B virus and human immunodeficiency virus infection among pregnant women in Bahir Dar city, Northwest Ethiopia: a cross sectional study. BMC Infect Dis 14:118.
- Berhe HYG, Addis Z, Slassie H, Anagaw B, Unakal C (2013) Seroprevalence and Associated Risk Factors of Human Immunodeficiency Virus and Hepatitis B Virus Infections among Prison Inmates. J Pharm Biomed Sci 30: 1035-1045.
- Mahboobi N, Porter SR, Karayiannis P, Alavian SM (2013) Dental Treatment as a Risk Factor for Hepatitis B and C Viral Infection. A Review of the Recent Literature. J Gastrointestin Liver Dis 22: 79-86.
- Humayed SMA (2016) The risk of acquiring hepatitis B and C viral infections following tooth extraction in Al Farsha area, south-western Saudi Arabia. The Saudi Journal for Dental Research 7: 127-131.
- No authors (2017) Enzyme-linked immunosorbent assay for the detection of HBsAg in serum or plasma. HBsAg ELISA kit. Biocare.
Citation: Bialfew Y, Hailu G, Samuel T (2018) Prevalence and Associated Factors of Hepatitis B Virus Infection among Blood Donors in Debre Markos Blood Bank Centre, Northwest Ethiopia, 2018. Epidemiology (Sunnyvale) 8: 363. DOI: 10.4172/2161-1165.1000363
Copyright: © 2018 Bialfew Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4541
- [From(publication date): 0-2018 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 3529
- PDF downloads: 1012