Case Report Open Access
Presurgical Treatment of Cleft Lip and Palate Babies with a PNAM Appliance: A Series of Four Case Reports
Beste Kamiloglu*Near East University, Nicosia, Cyprus
- Corresponding Author:
- Beste Kamiloglu DDS PhD
Near East University
Cyprus
Tel: 0090392 6802030, 0090392 6802615
E-mail: 59beste@gmail.com
Received date: July 22, 2014; Accepted date: September 02, 2014; Published date: Septemebr 09, 2014
Citation: Kamiloglu B (2014) Presurgical Treatment of Cleft Lip and Palate Babies with a PNAM Appliance: A Series of Four Case Reports. J Interdiscipl Med Dent Sci 2:148. doi:10.4172/2376-032X.1000148
Copyright: © 2014 Kamiloglu B. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Embryonic development of the head and face are among the most complex prenatal developmental events. Any disturbance during the developmental stage can result in craniofacial abnormalities, and the timing of the disturbance and intensity of the interruption affect the severity and type of the anomaly. Cleft lip and palate are relatively common congenital malformations and are readily diagnosed. Treating cleft lip and palate defects is important because of the severe aesthetic, functional, and serious psychological problems faced by both patients and their parents. It is recommended that cleft lip and palate patients from 0 to 18 years old undergo treatment with a multidisciplinary team. In this series of clinical reports, we describe clinical orthodontic treatment approaches using a presurgical nasoalveolar moulding (PNAM) in newly born unilateral and bilateral cleft lip and palate babies. Three boys and one girl were selected from among other cleft lip and palate patients because some information about the possible aetiology of the clefts was observed and the parents were cooperative during treatment. The objectives of PNAM use in unilateral and bilateral cleft lip and palate patients are to presurgically decrease the severity of the cleft size, maintain a narrower cleft palate, and increase the length of the columella and height of the nostrils. With parental cooperation, the treatment goals were achieved in these cases.
Keywords
Cleft lip and palate; Developmental craniofacial anomalies; Multidisciplinary treatment approach; PNAM appliance
Introduction
Craniofacial development is one of the most complex events during embryonic development, and craniofacial abnormalities are among the most common of all birth defects. Compared to many other birth anomalies, cleft lip and palate (CLP) are readily diagnosed. The primary palate is the keystone to the upper lip and the anterior portion of the definitive palate, and embryological maldevelopment can affect breathing, sucking, swallowing, mastication, osculation, speech, and facial physiognomy. The secondary palate constitutes the floor of the nasal cavity and the roof of the mouth, which includes the anterior hard palate and posterior soft palate. It is an essential component of normal respiration, mastication, deglutition, and speech [1].
Cleft lip and/or cleft palate are structural abnormalities that occur in the embryonal period of life between the 4th and 10th weeks. Any interruption in this tightly controlled processing chain can result in a facial cleft, among which orofacial clefts and cleft lip and palate are most frequent [2]. The lip and primary palate have distinct developmental origins from the secondary palate [3]. Cleft lip defects are usually considered a single entity, and an accompanying cleft palate represents a more severe form [4].
The aetiology of cleft lip and palate is still unknown, but both genetic and environmental factors may be responsible for many congenital malformations that can result from the developmental process failing to reach some developmental end point or threshold [5]. Cleft lip with cleft palate occurs twice as often as cleft lip alone. The cause of the familial aggregation of the disease may be genetic, environmental, or both [6]. A population- and family-based analysis demonstrated a positive association between TGFB3 and nonsyndromic cleft lip and palate. Also, a novel mutation of PAX9 may contribute to the development of cleft lip and palate [7]. Recently, evidence for the involvement of a major gene in the aetiology of cleft lip and palate has been reported [8]. Poor nutrition, tobacco smoke, alcohol, viral infection, and medicinal drugs are among the lifestyle and environmental risk factors believed to be involved. Interactions between maternal and foetal genes are possible in the aetiology of the disease. Foetal alcohol syndrome, in which the mother consumes too much alcohol during pregnancy, plus maternal smoking increases the risk of orofacial clefts; the effect was observed more consistently and strongly for cleft lip and palate than cleft lip palate [9].
Clefts, which can be syndromic or non-syndromic, are the most common of all birth defects worldwide and a serious malformation; most are non-syndromic. Cleft lip and palate affects 1 out of 1000 liveborn Caucasians and 1 out of 500–1000 live-born children worldwide. An epidemiological study of nearly 6 million births in 23 EUROCAT registries showed that 70.80% of clefts occurred in isolation, whereas 29.20% were associated with other defects. Associated anomalies in multi-malformed cleft lip and palate patients in European countries, according to frequency, are musculoskeletal defects, cardiovascular defects, and defects of the central nervous system. The most frequent chromosomal anomaly was trisomy 13 [10]. Tunçbilek et al. examined 1229 cleft lip and palate patients and found that 151 had 206 additional malformations. In total, 55 were syndromic: Pierre Robin syndrome was the most common group [11].
Children born with cleft lip and palate may have severe difficulties in feeding, speaking, and hearing and have to cope with severe psychological problems at school and in their social lives. The management of this developmental malformation is multidisciplinary and involves surgical, dental, and orthodontic treatment; speech training; audiological treatment; and psychological therapy throughout childhood.
The cleft lip and palate -type deformity presents one of the most complex surgical challenges. The presurgical nasoalveolar moulding (PNAM) technique, developed by Grayson, aims to properly align the alveolus, lip, and nose; reduce the severity of the nasal deformity; and lengthen the columella without surgery [12]. In patients with both unilateral and bilateral clefts, the PNAM appliance helps to reduce the severity of the cleft, allowing the surgeon to achieve a better and more predictable stable result after surgery [13].
Case Series
Methods
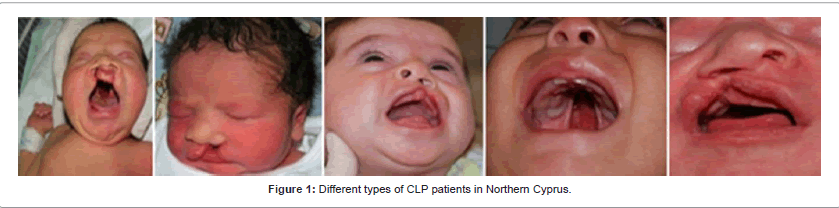
Patient profile: Cleft lip and palate patients of all classifications come to our clinic at the Near East University Faculty of Dentistry (Figure 1). Among them, cleft lip and palate babies, three males and one female, were selected for this case series. Of the three boys, one had non-syndromic unilateral cleft lip and palate, one had non-syndromic bilateral cleft lip and palate, and one had syndromic bilateral cleft lip and palate. The girl had a non-syndromic unilateral cleft lip and palate.
History and clinical examination, motivation of the parents: A general intraoral–extraoral examination was performed on each patient. All examinations were performed by an orthodontic consultant (BK). Before treatment, a medical history was taken and written informed consent for the treatment of the cleft lip and palate was obtained from the parents. Before starting the treatment procedure, parents were motivated by showing the treatment stages and photos of previously treated cleft lip and palate patients at our clinic. Three of the patients were first examined at 24–72 h of age. One male patient presented at our clinic at 54 days of age wearing a feeding plate applied at another orthodontic treatment centre abroad.
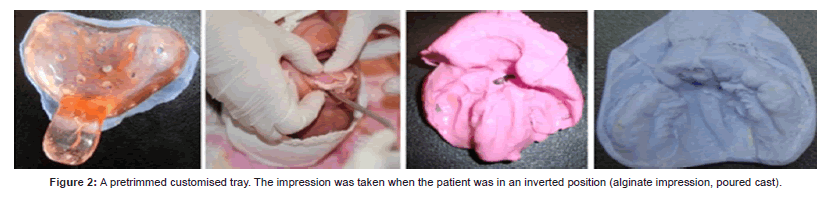
Impression tray, impression technique, and stone model: An initial impression of the cleft lip and palate from the newborn baby was obtained within 72 h of postnatal life. Although a heavy-bodied silicone impression material is commonly preferred, we used a thickened alginate impression material. The alginate mixture was mixed manually using a mixing bowl and spatula. The infants were held in an inverted position to prevent the tongue from moving backward and to allow saliva to drain out of the oral cavity (Figure 2). A surgeon and general anaesthetist were present in case of any airway emergency.
Preliminary impressions were made using self-made acrylic trays or fabricated impression trays and orthodontic alginate was used. Custom trays were fabricated in the orthodontic laboratory and secondary impressions were made again using alginate impression material. After the impression, a dental stone cast was made by filling the impression with a mixture of dental stone and allowing it to set. The dental stone model was made to obtain measurements, to follow improvements, and to fabricate the appliance. The cleft region of the palate and alveolus was filled with modelling wax. Later the moulding prosthesis was finished and polished to be ready for use.
Feeding plate, PNAM appliance, and parent education: The first stage of treatment was for a feeding and alveolar moulding appliance. A soft denture liner was added in the area that required moulding, and selective grinding of the hard acrylic was done where movement was expected. The second stage occurred when in unilateral clefts the intraalveolar gap had been reduced to 5–6 mm and in bilateral clefts the premaxilla and prolabium were located mostly on the alveolar ridge. The PNAM targets the nasal cartilage moulding by incorporating a nasal stent component. The acrylic at the active tip of the nasal stent was covered with a thin layer of soft denture lining material to help prevent tissue irritation. An extraoral retentive button was fabricated with a ~40° downward angle. Betafix Surgical Hypoallergenic Flexible Tape, 2.5 × 5 cm, and orthodontic elastics were used for retentive taping. Postinsertion instructions were given to the parents regarding the wear and hygiene of both the feeding appliance and the PNAM. The parents were asked to disinfect the appliance daily by cleaning it first with a toothbrush, soaking it in lukewarm water containing one quarter of an effervescent Steradent denture-cleansing tablet for 2 min, and later washing the appliance with drinking water. The nasal stent was kept out of the disinfecting solution because of the soft acrylic at the tip of the stent. The parents were asked to bring the cleft lip and palate babies in for weekly follow-up.
Surgical Procedure: All patients then underwent surgical procedures after the effects of the PNAM were sufficient. The PNAM appliance was constructed when the babies were 6 weeks old and was used until the primary surgical closure of the cleft lip and nose, which was performed at ~5 months of age. Thus, all of the patients underwent operations after 2–3 months of PNAM use.
Case Report 1
Case 1 was a male baby with non-syndromic complete bilateral cleft lip and palate. His medical history was taken. His parents’ marriage was non-consanguineous and both parents were middle aged. They had another healthy son age 10 with no health problems. The baby had previously had a feeding and alveolar moulding plate applied at another treatment centre abroad, and the cleft of the alveolus had been reduced to ~6 mm in width, which was the indication to add the nasal stent for the nasal moulding. The appliance was converted into a PNAM by adding a 0.9-mm stainless steel kidney-shaped wire with hard self-curing acrylic covered at the tip with semi-soft acrylic to prevent soft tissue irritation. The effectiveness of the moulding was increased by lip taping. The parents were asked to bring the baby in for weekly follow-up to adjust the PNAM appliance. A soft denture liner was added in the area that required moulding, and selective grinding of the hard acrylic was done where movement was expected. The nasal stent was also relocated. Parental cooperation in keeping the appliance in the mouth was quite good; the parents’ attitude toward their son was loving and caring, and they did not show concern about the appearance of their child. The lip and nose operation was performed successfully at 4 months of age at the initial treatment centre, which was the family’s choice. At the age of 3, a conversation was had with the child to check for speech problems. His pronunciation of words was clear and rhinolalia speech was not observed (Figure 3).
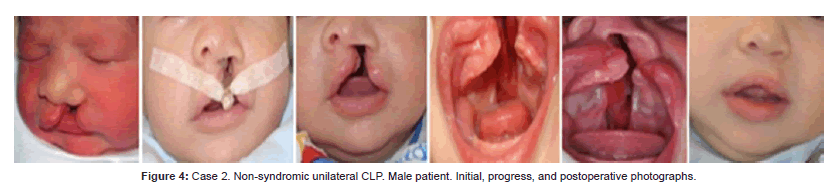
Case Report 2
This baby boy with unilateral cleft lip and palate was born at a private hospital in Nicosia, and we examined him the next day. The young mother refused to look at or hug the baby because of the cleft. At the 20th week of intrauterine life, her gynaecologist had shown her the cleft on ultrasound. The grandmother and father took care of the child. At the first visit, an anamnesis was taken. The baby’s parents were young, healthy, and non-consanguineous. The mother was a day school secretary and commonly used a photocopier at work. The father was an official employee. She had not drunk alcohol, smoked, or used any medication during pregnancy. The initial alginate impression was obtained and a dental stone model was made. A conventional feeding plate was prepared to maintain bottle feeding. The parents brought the baby for weekly follow-up and modification of the conventional feeding appliance. At 6 weeks of age, a secondary impression was made to prepare a PNAM. A retention button and 0.9-mm stainless steel wire were added outside the appliance. A nasal stent, covered first with selfcuring clear acrylic and the tip covered with a soft liner, was adjusted in the nostril aperture, pushing the nasal dome outward. The PNAM appliance was supported with orthodontic elastics incorporated into loops of thin hypoallergenic tapes. Instructions about the PNAM appliance were given, and the parents were told to keep it in the baby’s mouth almost 24 h per day. The parents were called at weekly intervals to gradually change the direction of the nasal stent. By the age of 4 months, the lip and nose operation was performed by the reconstructive surgery team. No speech problem was observed at age 4 (Figure 4).
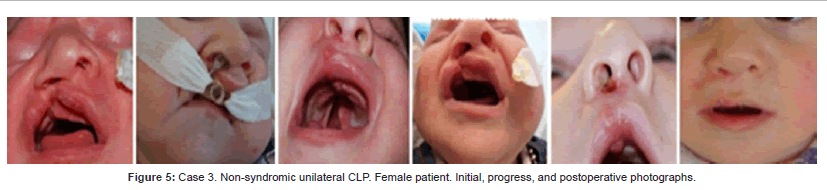
Case Report 3
This female baby had a non-syndromic unilateral cleft lip and palate. She was the second daughter in the family. The family had no previous history of any congenital anomaly. Her parents were healthy and young; her mother was a housewife and her father was a farmer living in a small village. They had another healthy 5-year-old daughter. The baby was being kept at the neonatal intensive care unit of a public hospital and was undergoing gavage feeding through a nasogastric tube. The primary aim was to enable mouth feeding of the baby with the help of a feeding plate and to discharge her from the hospital. A preliminary intraoral impression was taken and a simple feeding appliance was prepared. The parents were asked to bring her in for weekly follow-up. Soft denture liner was added in the area that required alveolar moulding, and selective grinding of hard acrylic was done where movement was expected in narrowing the cleft alveolus. At 8 weeks of age, a secondary impression was made to prepare the presurgical PNAM appliance. At 5 months of age, the operation was performed successfully by the reconstructive surgery team. Later no speech problem was detected. Her pronunciation of words was clear, the quality of her voice was normal, and no rhinolalia speech was observed (Figure 5).
Case Report 4
Case 4 was a male syndromic complete bilateral cleft lip and palate baby. His first visit to our clinic was at 6 days of age. His medical history was taken. The parents’ marriage was non-consanguineous. His mother was 36 years old and his father was a younger man. They had another healthy son, age 3. The mother was a croupier at a casino and was a heavy cigarette smoker. The father was unemployed. The mother mentioned that she had suffered serious stress during pregnancy because of serious financial problems. Additional features of the syndromic bilateral cleft lip and palate involved one kidney and a malformed ear. All treatment procedures were performed in a planned order but the treatment schedule for the PNAM appliance could not be completed because the baby had to be operated on urgently for a hernia and the parents then moved to their home country for the operation, with the support of relatives. The hernia operation and lip operation was performed at 3 months of age at the parents’ request. This case showed that treatment cannot always be performed as planned (Figure 6).
Discussion
Cleft lip and palate is a serious malformation affecting 1 out of 1000 of live-born Caucasians and 1 out of 500–1000 live‑born children worldwide. In a study of Danish and Japanese nuclear families, cleft lip and/or palate were subjected to a complex segregation analysis based on a mixed model. The Japanese population had a higher incidence of cleft lip and palate but a lower recurrence risk among families. The conclusion was that major gene action and multifactorial inheritance played a significant role in the Caucasian (Danish) population but not in the Japanese population [14]. The incidence of cleft lip, cleft palate, and cleft lip and palate in blacks ranges from 0.18 to 1.67 per 1.000 [15]. The incidence of cleft palate in Finland is exceptionally high and shows geographical variation (higher incidence in eastern provinces). Increased drug consumption (salicylates, opiates, penicillin), increased frequency of fever and influenza in the first trimester, and abortion in the first and second trimesters are important epidemiological factors [16]. In fact, we cannot report the exact prevalence and incidence of cleft lip, cleft palate, or cleft lip and palate because of miscarriages and the elective termination of pregnancies after ultrasound observations. This means that we can only estimate the prevalence of cleft lip and palate among newborns, stillborns, and late abortions. The prevalence of cleft lip and palate varies around the world. The poorest populations do not have surveillance systems for birth defects, and the high reported prevalence of birth defects in some of these regions is not evidence based. The birth prevalence in Asian populations is similar to published rates for Caucasians.
Between 2008 and 2014, eight babies (four boys, four girls) with different types of clefts presented at our clinic. Two boys had complete bilateral cleft lip and palate, one boy had unilateral cleft lip and palate, and one boy had soft and hard palate clefts. Among the girls, one had a complete bilateral cleft lip and palate, two had unilateral cleft lip and palate, and one had only uvula bifida. One of the eight cleft lip and palate babies was a syndromic bilateral cleft lip and palate case that included auricular and renal defects. The aetiology of the syndromic cleft might have been the mother’s older age at her pregnancy and stress and heavy cigarette smoking during pregnancy.
Seasonal variation also occurs in various countries. In Asian populations, cleft lip and palate is mostly observed between January and August. From August through December, prevalence is consistently low [17]. In our experience, cleft lip and palate is mostly seen between March and September in North Cyprus.
Clefts of the lip and palate are classified into three main categories: cleft of the lip; cleft of the palate, which involves the hard and soft palates or only the soft palate; and complete bilateral cleft lip and palate, the most severe category. Cleft lip and palate can also be classified as non-syndromic and syndromic. In syndromic cleft lip and palate, one or more additional features are involved with the cleft lip and palate. Non-syndromic lip clefts, with or without the palate, and cleft palate alone are among the most frequently observed congenital anomalies.
Facing the reality of having a cleft lip and palate baby is a disappointing, shocking, and traumatic experience for most parents. One of our patients’ mothers refused to see and cuddle her baby for a long period of time, and the baby’s grandmother took on the responsibility of looking after the child. cleft lip and palate patients may have problems with feeding, speaking, and hearing, in addition to social and psychological problems [18]. It is important to tell parents that it is normal to feel unhappy, anxious, shocked, and scared of having a cleft lip and palate baby, and during the first days the newborn’s parents need to know basic information about caring for a cleft lip and palate baby [19].
Of primary importance is teaching a cleft lip and palate baby’s mother or relatives how to feed the baby properly with a feeding plate. When we handed the plate over to the parents, we explained about maintaining oral hygiene and cleaning, inserting, and removing the plate. When the feeding plate was first applied in the oral cavity, we tested bottle feeding and observed that the baby was able to suckle without problems. The baby was kept in an upright position and breast milk was preferred for bottle feeding. More detailed information about caring for a cleft lip and palate child can be given to the parents later, and they can be reassured that after a lip operation the baby will have a more aesthetic appearance.
Cleft lip and palate requires multidisciplinary treatment, and complete bilateral cleft lip and palate is most difficult for the cleft team to treat. The lip operation is performed at 3–5 months according to the baby’s general health and weight gain and cleft palate repair is typically delayed until about 18 months of age [20].
The presurgical treatment of cleft lip and palate cleft lip and palate patients begins with taking a preliminary impression and later a secondary impression, if necessary. The dental stone model is obtained both to make the appliance and to follow up on improvements in the deformity. The initial prosthesis is a passive appliance called a feeding plate and only facilitates sucking and deglutition and partially seals the cleft. A retention button is positioned at a 40° angle to the anterior plane, and orthodontic elastics and hypoallergenic tapes help to secure the feeding plate in the mouth.
The construction of a nasal stent for nasal moulding is delayed until the cleft of the alveolus is reduced to 5–6 mm in width. The treatment goal of the PNAM appliance is to restore the normal anatomy of the lip, nose, and palate and to ease the surgeon’s alignment of the cleft segments. Unilateral cleft lip and palate is associated with significant nasal cartilage abnormalities and asymmetry of the alar base and cartilage. The lower lateral alar cartilage is depressed and concave [21]. A PNAM reduces the severity of the deformity and helps to obtain more stable results after the primary lip closure operation, especially in unilateral cleft lip and palate babies. The PNAM also reduces the costs of more complex treatments and operations. Mishra et al. observed the clinical effects of presurgical PNAM appliance use, and their findings showed better nostril height and profile in unilateral cases than bilateral cases [22]. Our treatment results confirmed these findings.
Nasal stents for the PNAM appliance were constructed on the feeding plate and weekly adjustments were required for maximum effectiveness [23,24]. Weekly adjustments were made using a semisoft acrylic to arrange maxillary lateral segments, shape nostrils, and lengthen the columella. Modifications were made by grinding the hard acrylic from areas where movement was expected, and a very thin soft denture liner (0.5–1 mm) was added in areas where moulding was required.
The PNAM appliance is recommended for full-time use, but parents must be careful to prevent ulceration of the nostrils and maxillary mucosa [25]. Significant reductions in columella deviation and increases in columella length, nostril height, and axial inclination on the cleft side in unilateral cleft lip and nose have been reported as a result of the appropriate use of a PNAM appliance [26].
Conclusions
In this study, three male and one female cleft lip and palate babies were selected according to the following criteria: possible aetiology of the cleft, classification (syndromic vs. non-syndromic), and expected parental cooperation during treatment. Babies suffering from cleft lip and palate may have to face severe aesthetic and functional problems, and serious psychological problems may arise both for themselves and for their parents. It is recommended that cleft lip and palate patients undergo treatment with a multidisciplinary team. The PNAM appliance can be used to treat unilateral and bilateral cleft and palate anomalies in newborns. This technique is easy, safe to use, and inexpensive. It helps increase the length of the columella and height of the nostrils, reducing the need for secondary rhinoplasties. The alveolar moulding can also help to reduce the number of future alveolar bone grafting surgeries. The PNAM appliance is used until the time of the cleft lip operation, typically 4–5 months of age, which provides a better appearance for the cleft baby and positively affects parental psychology. In this case series, the advantages of early management of both bilateral and unilateral cleft lip and palate defects with the PNAM appliance have been reported. Use of the PNAM application for 2–3 months provided a satisfying result before lip and nose surgery.
This series of case reports also provides information about the possible aetiologies of the clefts in this population. To the best of our knowledge, no other study or case report has been published on cleft lip and palate in Northern Cyprus, which has a small population of approximately 350,000 people of many different origins. Thus, this information may be beneficial for further studies and for presurgical interventions in this particular population.
References
- Wyszynski DF (2002) Cleft lip and palate: From origin to treatment. (1st edn), Oxford University Press. New York.
- Stanier P, Moore GE (2004) Genetics of cleft lip and palate: Syndromic genes contribute to the incidence of non-syndromic clefts. Hum Mol Genet 13: 73–81.
- Mossey PA, Little J, Munger RG, Dixon MJ, Shaw WC (2009) Cleft lip and palate. Lancet 374: 1773–85.
- Harville EW, Wilcox AJ, Lie RT, Vindenes H, Abyholm F (2005) Cleft Lip and Palate versus Cleft Lip Only: Are They Distinct Defects?Am J Epidemiol 162: 448–453
- Fraser FC (1970) The Genetics of Cleft Lip and Cleft Palate. Cleft Palate Craniofac J22: 336–352.
- Christensen K (1999) The 20th Century Danish Facial Cleft Population: Epidemiological and Genetic- Epidemiological Studies. Cleft Palate Craniofac J 36: 96–104
- Ichikawa E, Watanabe A, Nakano Y, Akita S, Hirano A, et al. (2006) PAX9 and TGFB3 are linked to susceptibility to nonsyndromic cleft lip with or without cleft palate in the Japanese: Population-based and family based candidate gene analyses. J Hum Genet 51: 38–46
- Mitchell LE (1997) Genetic Epidemiology of Birth Defects: Nonsyndromic Cleft Lip and Neural Tube Defects Epidemiol Rev 19: 61–68.
- Little J, Cardy A, Munger RG (2004) Tobacco smoking and oral clefts: A meta-analysis. Bulletin of the World Health Organization 82: 213–223.
- Calzolari E, Pierini A, Astolfi G, Bianchi F, Neville AJ, et al. and EUROCAT Working Group (2007) Associated Anomalies in Multi-Malformed Infants With Cleft Lip and Palate: An Epidemiologic Study of Nearly 6 Million Births in 23 EUROCAT Registries. Am J Med Genet A 143: 528–537.
- Tunçbilek G, Özgür F, Balcı S (2004) 1229 Yarık dudak ve damak hastasında görülen ek malformasyon ve sendromlar. ÇocukSağlığı ve Hastalıkları Dergisi 47: 172–176.
- Grayson BH, Shetye PR (2009) Presurgical nasoalveolar moulding treatment in cleft lip and palate patients. Indian J Plast Surg 42: S56–S61.
- Altuğ AT, Grayson BH, Cutting C (2004) Tek Taraflı Dudak, Alveol ve DamakYarıklarında Cerrahi Öncesi Nazoalveoler Şekillendirme -Bölüm 1- Türk Ortodonti Dergisi 17: 331–338.
- Chung CS, Bıxler D, Watanabe T, Koguchı H, Fogh-Andersen P (1986) Segregation Analysis of Cleft Lip with or without Cleft Palate: A Comparison of Danish and Japanese Data. Am J Hum Genet39: 603–611.
- Vanderas AP (1987) Incidence of Cleft lip, Palate, and Cleft Lip and Palate Among Races: A review. Cleft Palate J 24: 216–225.
- Saxen I (1975) Epidemiology of cleft lip and palate: An attempt to rule out chance correlations. Cleft Palate Craniofac J 29: 103–110.
- Cooper ME, Stone RA, Liu YE, Hu DN, Melnıck M, et al. (2000) Descriptive Epidemiology of Nonsyndromic Cleft Lip with or without Cleft Palate in Shanghai, China, from 1980 to 1989.Cleft Palate Craniofac J37: 274–280.
- Dixon MJ, Marazita ML, Beaty TH, Murray JC (2011) Cleft lip and palate: Understanding genetic and environmental influences. Nat Rev Genet 12: 167–178.
- Young JL, O’riordan M, Goldstein JA, Robin NH (2001) What Information Do Parents of Newborns With Cleft Lip, Palate, or Both Want to Know? Cleft Palate Craniofac J 38: 55–58
- Shah CP, Wong D (1980) Management of children with cleft lip and palate. Can Med Assoc J 122: 19–24.
- Grayson BH, Cuttıng CB (2001) Presurgical Nasoalveolar Orthopedic Molding in Primary Correction of the Nose, Lip, and Alveolus of Infants Born With Unilateral and Bilateral Clefts. Cleft Palate Craniofac J 38: 193–198.
- Mishra B, Singh AK, Zaidi J, Singh GK, Agrawal R, et al. (2010) Presurgical Nasoalveolar Molding for Correction of Cleft Lip Nasal Deformity: Experience From Northern India. Eplasty 10: 443–457.
- Yang S, Stelnicki EJ, Lee MN (2003) Use of Nasoalveolar Molding Appliance to Direct Growth in Newborn Patient With Complete Unilateral Cleft Lip and Palate. Pediatr Dent 25: 253–256.
- Radhakrishnan V, Sabarinath VP, Thombare P, Hazarey PV, Bonde R, et al. (2010) Presurgical Nasoalveolar Molding Assisted Primary Reconstruction in Complete Unilateral Cleft Lip Palate Infants. J Clin Pediatr Dent 34: 267–274.
- Murthy PS, Deshmukh S, Bhagyalakshmi A, Srilatha KT (2013) Pre Surgical Nasoalveolar Molding: Changing Paradigms in Early Cleft Lip and Palate Rehabilitation. J Int Oral Health 5: 70–80.
- Gomez DF, Donohue ST, Figueroa AA, Polley JW (2012) Nasal Changes After Presurgical Nasoalveolar Molding (PNAM) in the Unilateral Cleft Lip Nose. Cleft Palate Craniofac J49: 689–700.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 16095
- [From(publication date):
December-2014 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 11366
- PDF downloads : 4729