Preoperative Ultrasound Guided Botulinum Toxin A Injection for Complex Ventral Wall Hernia Repair: One Tertiary Care Centerâs Approach
Received: 16-Nov-2023 / Manuscript No. roa-23-120254 / Editor assigned: 18-Nov-2023 / PreQC No. roa-23-120254 / Reviewed: 30-Dec-2023 / QC No. roa-23-120254 / Revised: 06-Dec-2023 / Manuscript No. roa-23-120254 / Published Date: 11-Dec-2023
Abstract
Purpose: To discuss the utility of administrating botulinum toxin A (Botox) as an adjunct to surgical repair of complex abdominal wall hernias. Through discussion of the ultrasound-guided procedural technique and outcome data of one tertiary care center, it is our intention to bring awareness to this newer therapeutic option to facilitate the performance of this procedure at other care centers on a larger scale.
Materials and Methods: The procedure method of ultrasound-guided Botox injections and clinical course at one institution will be discussed. Outcome data including complications, achievement of primary fascial closure, rate of hernia recurrence, and patient population will be presented.
Results: Preoperative ultrasound-guided botulinum toxin A injection is a safe and effective procedure in patients undergoing complex ventral abdominal wall hernia repair that helps facilitate primary closure of large abdominal wall defects.
Conclusion: Awareness of this safe and effective preoperative image-guided procedure will help facilitate performance of this technique at more care centers, increasing the likelihood of primary closure of abdominal wall defects in more patients with large complex ventral hernias.
Keywords
Abdominal wall hernia; Loss of domain; Ultrasound guided intervention; Botox
Introduction
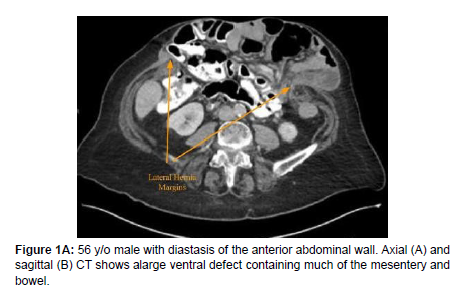
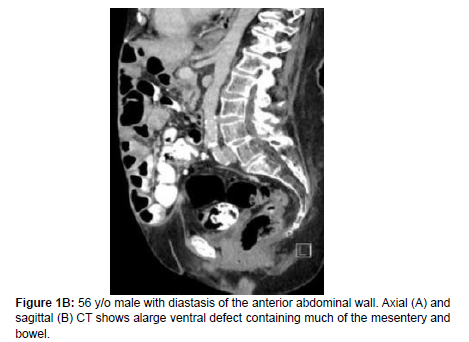
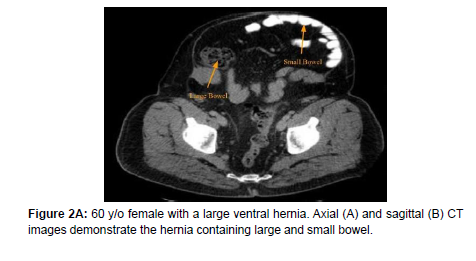
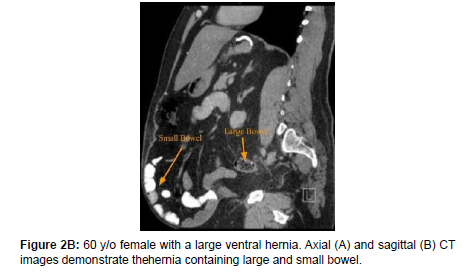
Abdominal wall reconstruction of complex ventral hernias presents several significant surgical challenges. Complex ventral hernias with loss of domain, described as large abdominal wall defects that cannot accommodate the abdominal viscera, occur when abdominopelvic contents distribute into the hernia sac (Figures 1-3) [1]. This herniation promotes increased lateral muscle retraction and abdominal wall muscle tension, causing difficulties with tissue approximation and subsequent risk for postoperative pain, compartment syndrome, and hernia recurrence [2-4]. Many of the current surgical techniques that aim to improve the preoperative expansion of the abdominal wall musculature, including pneumoperitonisation, myocutaneous fascial expanders, and component separation, are associated with high rates of post-operative wound infection and deep muscle injury, contributing to high costs and hernia recurrence rates [5,6].
Utilization of Botulinum Toxin A (BTA) has emerged as a promising technique for preoperative abdominal wall muscle relaxation [3]. A neurotoxin derived from Clostridium botulinum, BTA acts by blocking acetylcholine ligand-receptor binding at the neuromuscular junction, leading to flaccid paralysis of the local musculature. Commercially marketed as Botox and Dysport, BTA is frequently used for cosmetic procedures, dystonias, pain management, and spasticity disorders given its efficacy and duration of effects for up to 6 months from the time of administration. Since 2006, human and animal models have shown BTA’s preoperative paralytic efficacy on abdominal wall prior to operation via the lengthening and thinning of local musculature [7,8]. BTA administration may thus serve as a suitable candidate for assisting in the primary fascial closure of large hernia defects [9-13].
Methods and Material
Patients with extensive ventral wall defects with loss of domain presented to the Musculoskeletal Radiology division for US-guided injection of BTA into the abdominal wall musculature. There were 26 instances of ultrasound (US)-guided administration of BTA on 24 different patients with ventral hernias with significant loss of domain, identified according to surgical consultation documentation. The first patient of the cohort later underwent two additional US-guided BTA injection procedures solely intended as an adjunct to pain relief and not with the intention of fascial closure. As such, this patient’s subsequent encounters were excluded from the data set. The US-guided procedures were performed by the Musculoskeletal Radiology division of a 1,110 bed-academic hospital in Southeast Michigan from May 2015 to July 2018. After obtaining Institutional Review Board (IRB) approval, outcome data following the US-guided BTA injection procedure and ventral hernia repair of these 24 patients were obtained through observational retrospective review of electronic medical records. All the hernias were described as “post-surgical” in etiology.
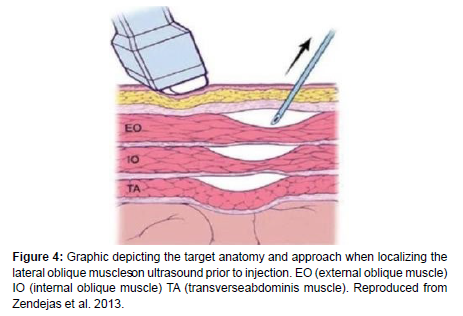
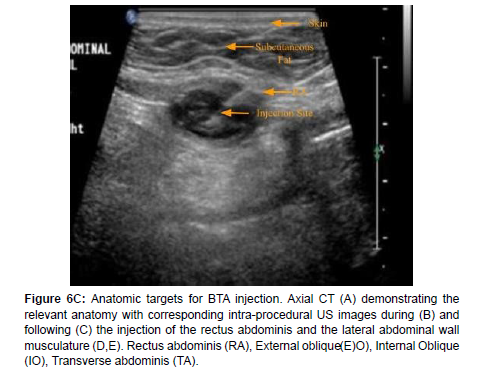
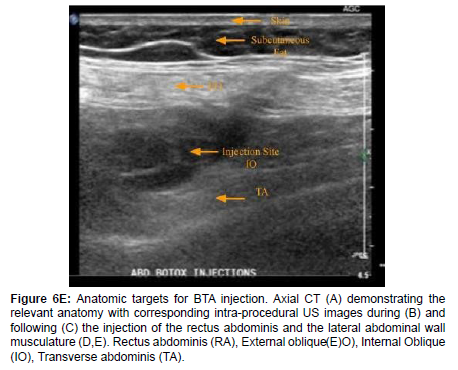
Although variable, the target time frame for BTA injection was 4 weeks prior to hernia repair. Versed and Fentanyl were administered to provide conscious sedation by an independent radiology nurse throughout the duration of the procedure. The abdomen was prepared and draped in a sterile fashion. Each injection site was anesthetized with 1% lidocaine prior to the administration of BTA (Figure 4) [11]. 300 mg of BTA was diluted in 150 cc of normal saline and under real-time ultrasound guidance, a 20-gauge spinal needle was used to administer the dilute BTA into the muscle belly of the superior, mid, and inferior portions of the rectus abdominis and lateral wall muscles (transverse abdominis, internal oblique, and external oblique). Completed injection sites were subject to minor variations in procedure technique given the variability of the size of ventral defect, degree of muscle retraction, and target visibility. The rectus abdominis was frequently difficult to visualize due to significant thinning which caused concerns for safe injection and led to reduced administrations in that muscle region (Figure 6).
Figure 6A: Anatomic targets for BTA injection. Axial CT (A) demonstrating the relevant anatomy with corresponding intra-procedural US images during (B) and following (C) the injection of the rectus abdominis and the lateral abdominal wall musculature (D,E). Rectus abdominis (RA), External oblique (E)O), Internal Oblique (IO), Transverse abdominis (TA).
Figure 6B: Anatomic targets for BTA injection. Axial CT (A) demonstrating the relevant anatomy with corresponding intra-procedural US images during (B) and following (C) the injection of the rectus abdominis and the lateral abdominal wall musculature (D,E). Rectus abdominis (RA), External oblique (E)O), Internal Oblique (IO), Transverse abdominis (TA).
Figure 6C: Anatomic targets for BTA injection. Axial CT (A) demonstrating the relevant anatomy with corresponding intra-procedural US images during (B) and following (C) the injection of the rectus abdominis and the lateral abdominal wall musculature (D,E). Rectus abdominis (RA), External oblique (E)O), Internal Oblique (IO), Transverse abdominis (TA).
Figure 6D: Anatomic targets for BTA injection. Axial CT (A) demonstrating the relevant anatomy with corresponding intra-procedural US images during (B) and following (C) the injection of the rectus abdominis and the lateral abdominal wall musculature (D,E). Rectus abdominis (RA), External oblique (E)O), Internal Oblique (IO), Transverse abdominis (TA).
Figure 6E: Anatomic targets for BTA injection. Axial CT (A) demonstrating the relevant anatomy with corresponding intra-procedural US images during (B) and following (C) the injection of the rectus abdominis and the lateral abdominal wall musculature (D,E). Rectus abdominis (RA), External oblique (E)O), Internal Oblique (IO), Transverse abdominis (TA).
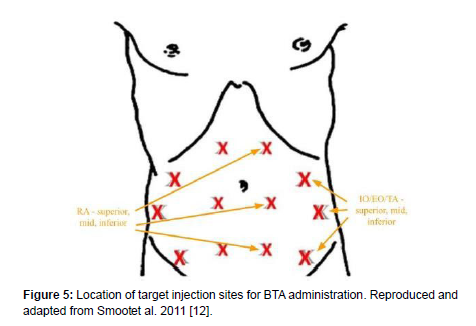
An example of typical injected volumes and locations during the procedure are as follows (Figure 5) [12]:
Right inferior oblique: 12 cc (4cc at each layer)
Right mid oblique: 12 cc (4cc at each layer)
Right superior oblique: 12 cc (4cc at each layer)
Right inferior rectus abdominis: 4 cc
Right mid rectus abdominis: 4 cc
Right superior rectus abdominis: 4 cc
Left inferior oblique: 12 cc (4cc at each layer)
Left mid oblique: 12 cc (4cc at each layer)
Left superior oblique: 12 cc (4cc at each layer)
Left inferior rectus abdominis: 4 cc
Left mid rectus abdominis: 4 cc
Left superior rectus abdominis: 4 cc
Measurements of the transverse diameter of the abdominal wall defect were obtained at the maximum defect width from the medial edge of the rectus abdominis on each side. The most recent axial abdominal CT available prior to BTA administration was used to determine these measurements.
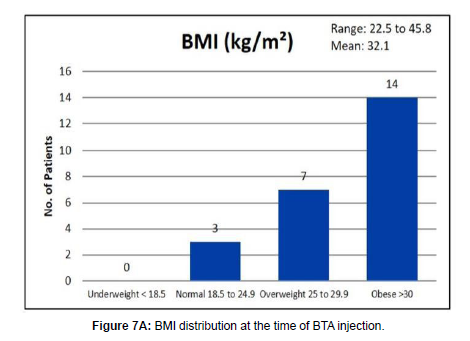
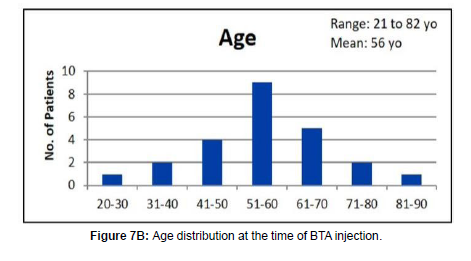
*One patient in our cohort did not undergo hernia repair due to significant comorbidities. The post ventral hernia repair outcome data is therefore calculated using 23 patients total (Figure 7).
Results
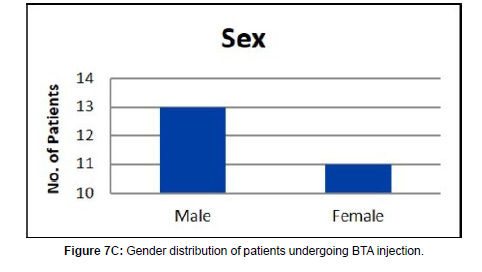
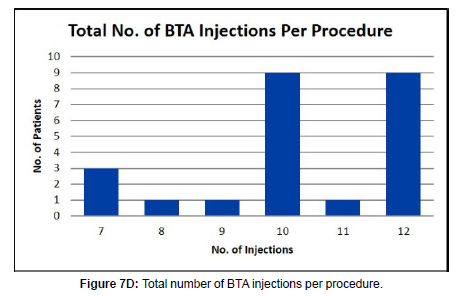
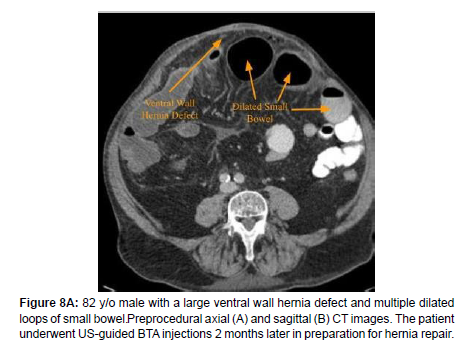
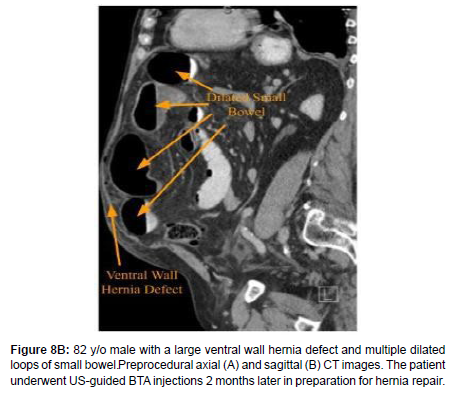
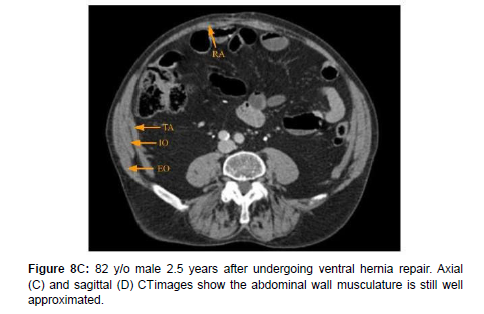
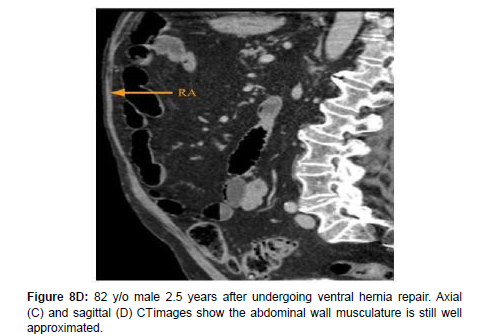
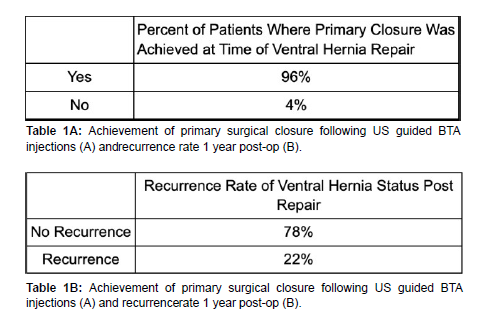
96% of our patient cohort achieved primary closure at the time of hernia repair. At 1-year post-op, 78% had experienced no recurrence (Figure 8). The mean age of the 24-patient cohort was 56 years and was predominantly male. Mean patient BMI at the time of BTA administration was 32.1. Most patients received a total of 10 to 12 injections (Table 1A and 1B). Mean hernia defect width was 15.8 centimeters (cm) with a range of 4.9 to 29.2 cm. Average time from BTA injection to hernia repair was 49 days with a range of 8 to 133 days. 0 of 24 patients experienced a documented US-related complication. 5 of 23 patients experienced a surgical procedure-related complication such as post-operative fluid collection, chronic wound, or bowel perforation.
Discussion
Outcome data on 24 patients undergoing 26 preoperative USguided abdominal wall BTA injections prior to ventral hernia repair was reported. Among studies by Elstner et al. and Rodriguez-Acevedo et al., our cohort is one of the largest data sets to examine this topic to date [2,9]. Of the 23 patients who underwent ventral hernia repair, 96% of patients achieved primary closure. This finding is consistent with the published literature that has reported a closure rate of 83% when preoperative abdominal wall BTA injections were performed [8]. Abdominal hernia recurrence was experienced by 22% of the patients in our data set. This is a significant reduction in comparison to the recurrence rate of up to 53% when only surgical techniques, such as mesh and component separation, were utilized for ventral hernia repair [10]. All BTA injections were well tolerated and there were no reported procedure-related complications.
Conclusion
Preoperative ultrasound-guided Botulinum Toxin a injection is a safe and effective procedure for patients undergoing complex ventral abdominal wall hernia repair that aids primary closure of large abdominal wall defects. Awareness of this emerging preoperative image-guided procedure will help facilitate the performance of this technique at more care centers, increasing the likelihood of primary closure of abdominal wall defects in many patients with large complex ventral abdominal wall hernias.
Conflict of Interest
There are no conflicts of interest.
References
- Azar FK, Crawford TC, Poruk KE (2017) Ventral hernia repair in patients with abdominal loss of domain: an observational study of one institution's experience. Hernia 21: 245-252.
- Rodriguez-Acevedo O, Elstner KE, Jacombs A, Read J, Tomazini Martins R, et al. (2017) Preoperative Botulinum Toxin A Enabling Defect Closure and Laparoscopic Repair of Complex Ventral Hernia. Surg Endosc 32: 831-839.
- Ibarra-Hurtado TR, Nuno-Guzman CM, Miranda-Oiaz AG, Troyo-Sanroman R, Navarra-Ibarra R, et al. (2014) Effect of botulinum toxin type A in lateral abdominal wall muscles thickness and length of patients with midline incisional hernia secondary to open abdomen management. Hernia 18: 647-652.
- Gillion JF, Sanders D, Miserez M (2016) The economic burden of incisional ventral hernia repairs: a multicentric cost analysis. Hernia 20: 819-830.
- Switzer NJ, Dykstra MA, Gill RS (2015) Endoscopic versus open component separation: systematic review and meta-analysis. Surg Endosc 29: 787-795.
- McAdory S, Cobb WS, Carbonell AM (2009) Progressive preoperative pneumoperitoneum for hernias with loss of domain. Am Surg 75: 504-508.
- Cakmak M, Caglayan F, Somuncu S (2006) Effect of paralysis of the abdominal wall muscles by botulinum A toxin to intraabdominal pressure: an experimental study. J Pediatr Surg 41: 821-825.
- Farooque F, Jacombs A, Roussos R (2016) Preoperative abdominal muscle elongation with Botulinum Toxin A for complex incisional ventral hernia repair. ANZ J Surg 86: 79-83.
- Elstner KE, Jacombs AS, Read JW (2016) Laparoscopic repair of complex ventral hernia facilitated by pre-operative chemical component relaxation using Botulinum Toxin A. Hernia 20: 209-219.
- Eriksson A, Rosenberg J, Bisgaard T (2014) Surgical treatment for giant incisional hernia: a qualitative systematic review. Hernia 18: 31-38.
- Zendejas (2013) Outcomes of chemical component paralysis using botulinum toxin for incisional hernia repairs. World J Surg 37: 2830-2837.
- Smoot D, Zielinski M, Jenkins D (2011) Botox A injection for pain after laparoscopic ventral hernia: a case report. Pain Med 12: 1121-1123.
- Weissler JM, Lanni MA, Tecce MG, Carney MJ, Shubinets V, et al. (2017) Chemical component separation: a systematic review and meta-analysis of botulinum toxin for management of ventral hernia. J Plast Surg Hand Surg 20: 1-9.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Nall C, Feraco D, Doshi S, Niblock M (2023) Preoperative UltrasoundGuided Botulinum Toxin A Injection for Complex Ventral Wall Hernia Repair: OneTertiary Care Center’s Approach. OMICS J Radiol 12: 504.
Copyright: © 2023 Nall C, et al. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 916
- [From(publication date): 0-2023 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 717
- PDF downloads: 199