Pregnancy Induced Hypertension and Associated Factors among Pregnant Women in Karamara Hospital, Jijiga, Eastern Ethiopia, 2015
Received: 18-Apr-2018 / Accepted Date: 25-May-2018 / Published Date: 01-Jun-2018 DOI: 10.4172/2376-127X.1000379
Abstract
Background: Pregnancy induced hypertension (PIH) is a significance rise of blood pressure during pregnancy, occurring after 20 weeks. It includes gestational hypertension, mild pre-eclampsia , sever pre-eclampsia and eclampsia. So more, women with PIH disorders may progress from mild diseases to more serious conditions. This study assessed pregnancy induced hypertension and associated factors among pregnant women.
Methods: A hospital based cross- sectional study design was conducted in Karamara hospital, Jijiga town among 408 pregnant. Systematic random sampling was employed. The data was collected using pretested semi-structured questionnaire and analyzed using SPSS Version 20. Results: The prevalence of pregnancy induced hypertension was 19.1% in Karamara hospital. Maternal education (AOR=2.5, 95% CI%=1.2-5.3), age (AOR=2.73, 95% CI=1.31-5.7), previous history of preeclampsia (AOR=19.3, 95% CI%=5.2-72.1) and family history of preeclampsia (AOR=7.2, 95% CI%=2.9-17.8) were identified as predictor factors for occurrence of pregnancy induced hypertension.
Conclusion and recommendations: One out of five women developed pregnancy induced hypertension in Karamara referral Hospital, Jigjiga Ethiopia. This is figure is very high compared to studies conducted in Ethiopia. Socio-demographic factors like age less than 25 years, lack formal education, previous history of PIH and family history of PIH were independent predictors of development of pregnancy induced hypertension. Hence, this study suggests that early detection and management of mothers with PIH should be mandatory as part of focused antenatal care. Lastly, this study suggests that further studies should be conducted to assess lifestyle and dietary factors, using analytical study designs.
Keywords: Pregnancy; Hypertension; Eclampsia
Abbreviations
AOR: Adjusted Odds Ratio; CI: Confidence Interval; COR: Crude Odds Ratio; PIH: Pregnancy Induced Hypertension; SPSS: Statistical Package for Social Science; WHO: World Health Organization
Background
Hypertensive disorder of pregnancy (HDP) is a common and very severe medical disorder specific to pregnancy. The Pregnancy induced hypertension (PIH) is a significance rise of blood pressure during pregnancy, occurring after 20 weeks [1]. It includes gestational hypertension, mild pre-eclampsia, sever pre-eclampsia and eclampsia. So more, women with PIH disorders may progress from mild diseases to more serious conditions [2].
The major causes of maternal deaths are similar across low income countries, often obstetric in origin and mainly severe preeclampsia and eclampsia and infection [3]. According to the World Health Organization (WHO) its incidence is seven times higher in developing countries (2.8% of live births) than in developed countries (0.4%) [4]. Eclampsia is reported to be associated with a maternal mortality rate of 0.5-10% usually requiring high quality intensive care [5].
Several studies have shown that history of chronic hypertension, being unmarried, nuliparity, family history of diabetes mellitus, extreme ages, race (being black) and others as risk factors for this problem [6].
However, there is paucity of information on the prevalence of pregnancy induced hypertension and associated factors in the study area. Hence this study was conducted to explore magnitude of pregnancy induced hypertension and associated factors among pregnant women, in Karamara Hospital, Jigjiga city of Somali regional state.
Methods
Study setting
The study was conducted in Jijiga Karamara hospital which is found in the capital of the Somali region state of Ethiopia. The region is a Pastoralist and Agro-pastoralist area and known for very lower prevalence rate of maternal health services. Karamara Hospital provides maternal, medical, surgical and pediatric health services. It has a total of 95 beds and 27 of them found in maternity ward.
Study design and sample
A Hospital based cross-sectional study was conducted in Karamara hospital, Jijiga town from February up to May 2015. All pregnant mothers attended maternal care services were our source population. All pregnant mothers who attend maternal care service after 20 weeks of gestation were included in the study. Mothers have history of chronic hypertension excluded from this study.
Sample size determination
The required sample size was determined using single population proportion formula with the following assumptions,
Level of confidence=95%
Type I error (α)=0.05
5% margin of error
Based on the assumption the prevalence pregnancy induced hypertension is 50%.
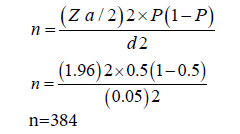
Given 10% non response rate, the final sample size is 423.
Sampling procedure
Source population estimated based on Karamara hospital maternal care service quarter year plan reports. So, Individual study subjects were selected by systematic random sampling during the data collection period until the required sample size was obtained. The sampling interval (k=2) was calculated by dividing the study population to the total sample size (423) and this interval was used to select study subjects. The first client was selected by simple random sampling among the first two maternal care service users based on the sampling frame.
Data collection and instrument
Census Data were collected by interviewer administered technique using a pretested semi-structured questionnaire developed from literatures. Questionnaire was prepared first in English then translated to local language (Somali) and back to English. It contains sociodemographic characteristics of mothers, obstetric history, signs and symptoms at presentation, laboratory data and maternal and prenatal outcomes. Four midwives were involved in the data collection and data quality was maintained through intensive supervision, pretesting and data collector training.
Data processing and analysis
Data were cleaned, edited and entered onto Epidata version 3.2.1 and exported to the statistical packages for social sciences (SPSS) version 20 statistical software for further analysis. Frequency distribution and cross tabulation were done against the variables of interest. Bivariate analyses were done to assess the association between explanatory variables and outcome variable of the study. All variables with a p-value of <0.25 at the bivariate analysis were included into multivariable logistic regression model in which odds ratio with 95% confidence intervals were estimated to identify independent predictors of pregnancy induced hypertension. P-values less to 0.05 were employed to declare the statistical significance.
Operational definitions
Chronic hypertension: Is Diastolic blood pressure 90 mmHg or more before first 20 weeks of gestation
Gestational hypertension: Defined as a blood pressure 110 by 90 mmHg 4 h apart after 20 weeks of gestation without proteinuria.
Preeclampsia: Is a pregnant woman with Gestational hypertension plus proteinuria was diagnosed.
Mild preeclampsia: Is when two readings of diastolic blood pressure 90-110 mmHg 4 h apart after 20 weeks gestation and Proteinuria up to 2+ through dipstick.
Severe preeclampsia: Is when two readings of diastolic blood pressure 110 mmHg or more after 20 weeks gestation and Proteinuria 3+ or more with blurred vision, severe headache, oliguria, altered mental status and epi-gastric pain.
Eclampsia: Is when Diastolic blood pressure 90 mmHg or more after 20 weeks gestation with Convulsions and Proteinuria 2+ or more high BP and plus seizure that cannot be attributed to some other cause.
Results
Socio-demographic characteristics
From a total of 423 sampled mothers, 408 were interviewed making a response rate of 96.45%. More than three fourth of the respondents were between the age of 20-34, with a mean age of 26.3 (+5.4 SD) years. Majority (80.1%) of them was urban dwellers and married (95.6%). Muslim 332 (81.4%) and the Somali ethnic group 255 (62.5%) were found to be predominant than others. Regarding to educational status, 101 (24.8%) mothers had no formal education, while 37.5% (153) respondents attended secondary and more (Table 1).
| Variables | Frequency | Percent |
|---|---|---|
| Age of mothers(year) | ||
| = 20 years | 73 | 17.9 |
| 20-34 years | 316 | 77.5 |
| = 35 years | 19 | 4.7 |
| Residence | ||
| Urban | 327 | 80.1 |
| Rural | 81 | 19.9 |
| Marital status | ||
| Married | 390 | 95.6 |
| Others*** | 18 | 4.4 |
| Religion | ||
| Muslim | 332 | 81.4 |
| Orthodox | 44 | 10.8 |
| Protestant | 22 | 5.4 |
| Catholic | 10 | 2.5 |
| Ethnicity | ||
| Somali | 255 | 62.5 |
| Oromo | 56 | 13.7 |
| Amhara | 45 | 11.0 |
| Guragie | 26 | 6.4 |
| Others | 26 | 6.4 |
| Maternal Education | ||
| No formal education | 101 | 24.8 |
| Primary education | 154 | 37.7 |
| Secondary education or more | 153 | 37.5 |
| Occupation of the mother | ||
| Employed* | 98 | 24.0 |
| Un employed** | 310 | 76.0 |
NB: *Government organization employees, Private organization employees
** House wives, Daily labours, Farmers, merchants, business owners, students
***Single, Divorced, Widow, Cohabited, Separated.
Table 1: Socio demographic characteristics of pregnant women attend maternal care service, Kharamara Hospital, Ethiopia, 2015.
Medical history and clinical condition
One out of ten pregnant women (8.1%) had previous history of renal disease. In addition, 24 (5.9%) of respondents had pregnancy induced hypertension in their previous pregnancy and forty-two (10.3%) of mothers had family history of pregnancy induced hypertension. Current clinical condition of the mother revealed Fifty-nine (14.5%) of respondents developed pitting edema (Table 2).
| Variables | Frequency | Percent |
|---|---|---|
| History of renal disease | ||
| Yes | 33 | 8.1 |
| No | 375 | 91.9 |
| Previous history of PIH | ||
| Yes | 24 | 5.9 |
| No | 384 | 94.1 |
| Family history of PIH | ||
| Yes | 42 | 10.3 |
| No | 366 | 89.7 |
| Edema | ||
| Pitting Edema | 59 | 14.5 |
| Non pitting Edema | 349 | 84.5 |
| Protein urea | ||
| No | 341 | 83.6 |
| 1+ | 2 | 0.5 |
| 2+ | 43 | 10.5 |
| = 3+ | 22 | 5.4 |
| Blood pressure | ||
| Systolic blood pressure | ||
| 90-129 | 301 | 73.8 |
| 130-139 | 25 | 6.1 |
| 140-159 | 27 | 6.6 |
| 160-179 | 48 | 11.8 |
| >180 | 7 | 1.7 |
| Diastolic blood pressure | ||
| <60 | 108 | 26.5 |
| 60-89 | 201 | 49.3 |
| 90-99 | 19 | 4.7 |
| 100-109 | 42 | 10.3 |
| >110 | 38 | 9.3 |
Table 2: Medical history and related conditions of pregnant women attended maternal care services, Kharamara Hospital, Ethiopia, 2015.
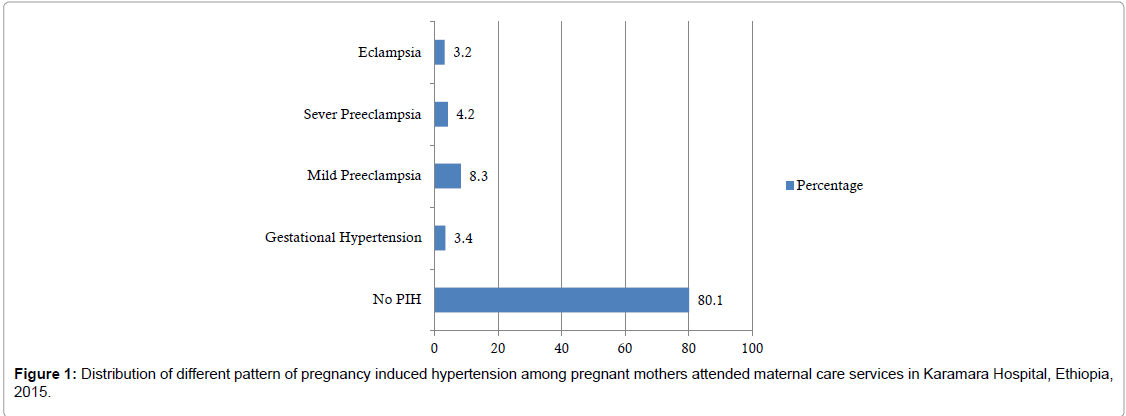
Regarding occurrence of pregnancy induced hypertension, 93 (19.1%) of the respondents had pregnancy induced hypertension. 34 (8.3%) of pregnant women developed mild preeclampsia, 17 (4.2%) had develop severe preeclampsia, 13 (3.2%) had develop eclampsia, 14 (3.4%) had gestational hypertension. (Figure 1).
Factor influencing pregnancy induced hypertension
In multivariate analysis age, maternal education, previous history of PIH and family history of PIH were identified as an independent predictor for pregnancy induced hypertension. The odds of pregnancy induced hypertension increase among women age ≥ 25 years (AOR: 2.7, 95% CI 1.3-5.7), without formal education (AOR: 2.5, 95% CI: 1.2-5.3), family history of preeclampsia (AOR: 6.2, 95% CI: 2.9-12.8) and family history of PIH (AOR: 19.3, 95% CI: 5.2-72.1) than their respective counter parts (Table 3).
| Variables | Pregnancy induced hypertension | |||
|---|---|---|---|---|
| Presence | Absence | COR(95%CI) | AOR(95%C) | |
| Age | ||||
| = 25 year | 51(23.2%) | 169(76.8%) | 1.8(1.07-3.0) | 2.7 (1.3-5.7) |
| <25 year | 27(14.4%) | 161(85.6%) | 1 | 1 |
| Maternal education | ||||
| No formal education | 33(32.7%) | 68(67.3%) | 2.8(1.7-4.8) | 2.5(1.2-5.3) |
| Formal education | 45(14.7%) | 262(85.3%) | 1 | 1 |
| Gravidity | ||||
| Primigravida | 40(22.9%) | 135(77.1%) | 1.5(0.9-2.5) | 1.6(0.8-2.8) |
| Multigravida | 38(16.3%) | 195(83.7%) | 1 | 1 |
| Previous history of PIH | ||||
| Yes | 19(79.2%) | 5(20.8%) | 20.9(7.5-58.2) | 19.3%(5.2-72.1) |
| No | 59(15.4%) | 325(84.6%) | 1 | 1 |
| Family history of PIH | ||||
| Yes | 22(52.4%) | 20(47.6%) | 6.1(3.1-11.9) | 6.2(2.9-12.8) |
| No | 56(15.3%) | 310(84.7%) | 1 | |
COR=Crude Odds Ratio; AOR=Adjusted Odds Ratio; CI=Confidence Interval.
Table 3: Multivariate logistic regression showing predictor factors of pregnancy induced hypertension among pregnant women attended maternal care services in Kharamara Hospital, 2015.
Discussion
The magnitude of pregnancy induced hypertension was 19.1% in Karamara hospital. It was high compared to studies in Ethiopia Tikur Anbessa hospital and Jimma referral hospital because 5.3% and 8.5% of pregnant women had pregnancy induced hypertension (PIH) respectively [7,8].
Pregnancy induced hypertension is influenced by varying and complex interrelated factors and multivariate logistic analysis showed that risk of pregnancy induced hypertension increases with age. Likewise, a study conducted in Dessie referral hospital and Ghana municipality showed that advanced maternal age was significantly associated with pregnancy induced hypertension [9,10].
The odds of pregnancy induced hypertension among mothers had no formal education 2.5 times than among mothers had formal education. It is in agreement with study conducted in mustaf hospital in Ilam which showed that the risk of preeclampsia increased 4 times in illiterate’s women compared to women with Academic education [11].
The odds of pregnancy induced hypertension 19.3 times increase among mothers had previous History of preeclampsia. Similarly a retrospective case control study conducted in Jahun, Nigeria showed that personal history of preeclampsia is 21.5 times increase the chance of developing severe preeclampsia/eclampsia [12].
The odds of pregnancy induced hypertension 7.2 times increase among mothers with family history of preeclampsia. It is congruent with study conducted in Dessie referral hospital and Ghana Municipality revealed that woman having family history of hypertension are found to be strongly associated with preeclampsia [9,10].
Conclusion and Recommendation
One out of five women developed pregnancy induced hypertension in Karamara referral Hospital, Jigjiga Ethiopia. This is figure is very high compared to studies conducted in Ethiopia. Socio-demographic factors like age less than 25 years, lack formal education and being prim-gravida mothers were significantly associated with pregnancy induced hypertension. In addition, medical histories like previous History of PIH and Family history of PIH were independent predictors of development of pregnancy induced hypertension.
Hence, this study suggests that early detection and management of mothers with PIH should be mandatory as part of focused antenatal care. Lastly, this study suggests that further studies should be conducted to assess lifestyle and dietary factors, using analytical study design.
Ethical Approval and Consent to Participate
The ethical approval and clearance for the study before data collection were obtained from Jigjiga University research publication and technology transfer office. Official letters were obtained from Kharamara Hospital. At the time of data collection, Informed consent was obtained from the respondents after explaining the purpose of the study.
Authors Contribution
LM conceived and designed the study, performed analysis and interpretation of data and drafted the manuscript. ZS, EW and SH participated in design conception, analysis and interpretation of data and the critical review of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We would like to acknowledge Jigjiga University for financial support and study participants for their involvement in the study.
References
- Â (2008) Medicine for Africa-medical information service. Preeclampsia/eclampsia.
- Federal democratic republic of Ethiopia, Ministry of health (2014) Basic emergencies obstetrics and neonatal care training manual.
- Alvarez JL, Gil R, Hernández V, Gil A (2009) Factors associated with maternal mortality in Sub-Saharan Africa: An ecological study.BMC Public Health 9: 462.
- Aali BS, Ghafoorian J, Mohamed-Alizadeh S (2004) Severe preeclampsia and eclampsia in Kerman, Iran: Complications and outcomes.Med Sci Monit10: 163-167.
- Roberts JM, Lain KY (2002) Recent Insights into the pathogenesis of pre eclampsia.Placenta23: 359-372.
- Teklu S, GayM A (2006) Prevalence and clinical correlates of the hypertensive disorders of pregnancy at Tikur Anbesa Hospital, Addis Abeba, Ethiopia. Ethiop Med J 44: 17-26.
- Wolde Z, Segni H, Woldie M (2011) Hypertensive disorders of pregnancy in Jimma University specialized hospital. Ethiop J Health Sci 21: 147-154.
- Tessema GA, Tekeste A, Ayele TA (2015) Preeclampsia and associated factors among pregnant women attending antenatal care in Dessie referral hospital, Northeast Ethiopia: A hospital-based study. BMC Pregnancy Childbirth 15: 73.
- Jones L, Takramah W, Axame WK, Owusu R, Parbey PA, et al. (2017) Risk factors associated with pregnancy induced hypertension in the Hohoe Municipality of Ghana. J Prev Med Healthc 1: 1011.
- Direkvand-Moghadam A, Khosravi A, Sayehmiri K (2013) Predictive factors for preeclampsia in pregnant women: A receiver operation character approach. Arch Med Sci 9: 684-689.
- Guerrier G, Oluyide B, Keramarou M, Grais RF (2013) Factors associated with severe preeclampsia and eclampsia in Jahun, Nigeria. Int J Womens Health 5: 509-513.
Citation: Mekonen L, Shiferaw Z, Wubshet E, Haile S (2018) Pregnancy Induced Hypertension and Associated Factors among Pregnant Women in Karamara Hospital, Jijiga, Eastern Ethiopia, 2015. J Preg Child Health 5: 379. DOI: 10.4172/2376-127X.1000379
Copyright: © 2018 Mekonen L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 18668
- [From(publication date): 0-2018 - Apr 06, 2025]
- Breakdown by view type
- HTML page views: 5675
- PDF downloads: 12993