Predictors and Clinical Outcome of Patients Admitted with First Episode Psychosis at Mirembe Mental Health Hospital in Dodoma, Tanzania: A Prospective Longitudinal Study
Received: 07-Apr-2023 / Manuscript No. IJEMHHR-23-79421 / Editor assigned: 10-Apr-2023 / PreQC No. IJEMHHR-23-79421 (PQ) / Reviewed: 24-Apr-2023 / QC No. IJEMHHR-23-79421 / Revised: 26-Apr-2023 / Manuscript No. IJEMHHR-23-79421 (R) / Published Date: 03-May-2023
Abstract
Objective: First Episode Psychosis (FEP) presents with varying clinical outcome on patients especially in early phase of treatment. Heterogeneity of the study populations, setting, and clinical diagnosis may all predict remission of symptoms. This study aimed at assessing the predictors of symptom remission in early phase of treatment among patients admitted for the FEP.
Methods: A sample of 131 FEP patients (aged ≥ 18) admitted with FEP were followed for 28 days. Mini International Neuropsychiatric Instrument (MINI) was used to make diagnosis at baseline. Positive and Negative Symptom Scale (PANSS), Montgomery and Asberg Depression Scale (MADRS) and Young Mania Rating Scale (YMRS) were used to measure severity and progression of symptoms during the follow-up period. Univariate and multivariable cox regressions were used to determine the predictors of symptom remission.
Results: Out of 131 subjects, 126 (96.18%) completed follow-up, of which 110 (87.30%) achieved remission of symptoms within follow-up period. Patients with longer Duration of Untreated Psychosis (DUP), 3-6 months adjusted Hazard Ration (aHR)=0.65, 95% CI=( 0.40-1.03) had decreased likelihood to remission of symptoms relative to those with less than three months of DUP and also patients living with their spouses had 0.31 decreased likelihood of remission of symptoms (aHR)=0.31, 95% CI=( 0.13-0.69) relative to those living alone.
Conclusion: Longer duration of untreated psychosis is associated with poorer remission of symptoms as reported in previous studies. Strikingly, living with a spouse could not predict better remission of symptoms as findings of earlier studies. Instead, this study suggests there may be more positive effect with social support on remission of symptoms of patients with FEP who live with their spouse and have longer DUP
Keywords: Duration of Untreated Psychosis (DUP); Mental disorder; Positive and Negative Symptom Scale (PANSS); Cox regression; Clinical outcome; Remission.
INTRODUCTION
First Episode Psychosis (FEP) is an experience of onset of psychotic symptoms for a first time in the life of an individual, however; it has also being described as having first contact to psychiatric care services following the presence of psychotic symptoms (Akena, et al.). The incidence of psychosis is approximately 26.6 new cases per 100,000 person years and has been accounted to 10% of global disease burden mostly contributed by low and middle income countries that has approximately 10% of people with psychosis who receive treatment (Kirkbride). Globally, studies on early intervention have presented improvement in remission of symptoms within first weeks of treatment and particularly a week 4 had been observed to have a good predictive value (Subeesh, et al.). The remission rate has been recorded by many studies to be increased towards an end point of follow-up, however; others studies report decreasing pattern. These variations of rate and as well predictors that influence the remission of the symptoms have been observed to differ across studies and setting (Emsley, et al.).
The female gender, being employed, being married, short Duration of Untreated Psychosis (DUP), higher education level, affective psychosis have been associated with early remission of symptoms. A younger age of onset, being single, longer DUP, lower education level, having a diagnosis of schizophrenia, use of substance, no daily occupation, family history of mental disorders are associated with poor symptoms reduction. However; other studies do not concur with findings as well others report no difference in age, sex, education level, having family history of mental disorders, occupation or marital status to those achieved symptomatic remission and those who do not achieve symptomatic remission in short term outcome (Bozzatello, et al.).
Moreover, most research on assessing the predictors of symptomatic remission among patients with FEP have been conducted in high and middle income countries whose findings may not be generalized elsewhere as evidence has shown that predictors influencing remission of symptoms differ across countries (Lambert, et al.). In Tanzania, cases presenting with psychosis are common (Jenkins, et al.), however; no study has investigated FEP and its predictors of symptomatic remission following initiation of antipsychotic medications. Therefore, this study aimed to assess the clinical outcome and determine socio demographic and clinical predictors of remission of symptoms following early intervention to patients with FEP in our setting.
MATERIALS AND METHODS STUDY
SETTINGS: This study was carried at Mirembe mental health hospital which is the only national referral health facility specialized on mental health and psychiatry treatment and rehabilitation services. The facility has a 600 bed capacity located in Dodoma, a capital city of Tanzania, a country with approximately 60 million populations with a median age of eighteen. The average annual growth rate was estimated to be 3.1% (Mwambingu). It is estimated that 100 patients are seen every day as outpatients and a total population of between 300 and 400 are inpatients at one point in time (Nyundo).
PARTICIPANTS: The study participants included patients who were seen at Mirembe mental health hospital from March, 2022 to July, 2022 with FEP, operationalized as individuals having (a) Experienced psychotic symptoms for the very first time in their lives or (b)A first contact to psychiatric care services butexperienced psychotic symptoms not more than twelvemonths since the onset (c) Received below three months ofprior antipsychotic treatment (d) Never beenhospitalized for psychosis earlier than three monthsprior to index admission (Akena, et al.). Before beinginterviewed, a written informed consent was soughtfrom all participants and care givers for those who were inno mental or physical capacity to do so.
STUDY DESIGN: This was a prospective longitudinal study whereby the patients with FEP were enrolled and follow-up assessments were conducted every day after initial treatment and patients were censored at the end of follow-up (after 28 days) or a day of discharge on pharmacological protocol. No particular intervention was initiated than what is normally offered.
SAMPLE SIZE AND SAMPLE PROCEDURE: The Krejcie and Morgan formula was used to calculate a minimum sample size of 124 participants. A total sample of 126 participants was consecutively recruited from patients seen with FEP at outpatient and emergence psychiatry department in Mirembe mental health hospital (Pauselli).
INCLUSION CRITERIA/EXCLUSION CRITERIA: The study inclusion criteria were; patients who were above 18 years old with FEP including diagnoses of schizophrenia spectrum disorder, affective disorder or substance use disorder according to the Mini International Neuropsychiatry Interview (MINI) version 7.0.2 at baseline (Koutsouleris, et al.). The exclusion criteria were patients who presented with psychoses secondary to organic etiology such as seizures or dementia.
INDEPENDENT VARIABLE: At baseline, clinical interviews and researcher designed questionnaires was used to record; the socio demographic characteristics, premorbid and clinical characteristics from patients and care givers. The socio-demographic details included age at assessment, age at onset, sex, marital status, education level, occupation status, living arrangement, family history of mental illness, DUP and baseline clinical diagnosis. DUP was calculated from the time of onset of symptoms to until initiation of treatment and categorized as below three months, 3-6 months and more than 6-12 months. M.I.N.I for DSM-5 was used to assess clinical diagnosis of schizophrenia, other psychotic disorders in schizophrenia spectrum disorders, major depressive disorder, bipolar disorder and the substance use disorder (Abbo, et al.). A Positive and Negative Symptom Scale (PANSS) for positive, negative psychotic, general psychopathology symptoms; a Young Mania Rating Scale (YMRS) for mania symptomatology and a Montgomery and Asberg Depression Rating Scale (MADRS) for depressive symptomatology.
The PANSS is a 30 item scale whereby symptom severity is rated on likert scale ranging from 1 (absent) to 7 (extreme). PANSS allows separate analysis of positive, negative and general psychopathology symptoms. The minimum total score of symptoms is 30 and 210 is maximum total score whereby a more than 50% score reduction from baseline total score at end point of follow-up was used to report remission of symptoms. PANSS with reliability and validity and high internal consistency has been used worldwide and in Uganda which is similar to setting of this study (Abbo, et al.).
The MADRS is a rating based in clinical interview with the broadly phrased questions about symptoms in more detailed that allow precise rating of severity. It can use collateral information for rating of the patients who cannot communicate/speak. The tool has a total number of 10 items with a likert score ranging from 0-6 and a total score of 0-60. The cut off score is 10 with score of 10-17 indicating mild, 18-34 moderate and 35-60 severe depression. The score of 9 andbelow indicates remission of depressive symptoms.This tool has been used in Uganda (Abbo, et al.).
The YMRS is a patient’s subjective report of symptom experience over the preceding 48 hours with 11 items rating. This tool has been used to rate the severity of manic symptoms. The additional information is based upon the clinical observations made during the course of clinical interview. It includes four items graded on 0 to 8 scales (irritability, speech, thought content and disruptive/aggressive behavior), while remaining seven items are graded on a 0 to 4 scale. The score range is 0-60 and a cut off score of 20 is taken as indicativeof illness. The tool has been used in Uganda (Abbo, etal.).
DEPENDENT VARIABLE: The remission of symptoms was defined as a state of at least seven days (one week) duration in which no symptoms are experienced and operationalized as more than 50% reductions of the PANSS total score, less than 20 score of YMRS total score and equal or less than 9 score from MADRS total score. No remission of symptoms was a less than 50% improvement of the PANSS total score, an equal or more than 20 score of YMRS total score and more than 9 score of the MADRS total score at end point or 28 days from the baseline which is within 72 hours after treatment is initiated. A patient who fulfilled criteria for both remission of symptoms from PANSS score, MADRS score and YMRS score was classified as “in symptomatic remission”, otherwise a patient was classified as “not in symptomatic remission”. This dependent variable was measured in nominal scale (1-Symptomatic remission or 2-No symptomatic remission).
DATA ANALYSIS: All data were collected and entered into a single database. Data were analyzed using Statistical Package for Social Sciences (SPSS) version 25.The descriptive analysis of the demographicpredictors and clinical predictors of FEP’s clinicaloutcome were performed using frequency tables, proportions, means and standard deviations. Using SPSS, descriptive statistics were calculated for two groups of those in symptomatic remission and those not in symptomatic remissions during the treatment (Brown).
This was done using independent sample t-test for continuous variables and on other hand; the χ² test (Fisher’s exact test) was used for categorical variables. Univariate cox regression analysis was first performed on each potential predictor variable (Kaminga).
Variables with P ≤ 0.25 were then entered into multivariable cox regression model using enter method. This methodology allows the investigation of the effects of several variables upon the time a specific event takes to happen. Time to remission was defined as the number of days from the initiation of antipsychotic medications until the last day of discharged.
For those who did not achieve remission, the last known date of end point of follow-up was used. Cox regression analysis was used to determine unadjusted Hazard Ratio (HR) and adjusted HR (aHR in multivariable analysis) with 95% Confidence Intervals (CI) for predictors of symptomatic remission. An HR of 1 indicates the same relative risk of remission, an HR<1 indicates lower relative risk and an HR>1 indicates higher relative risk. The level of significance was set at ≤ 0.05 (Brown, et al.).
RESULTS
Socio-demographic and clinical profile of the sample of the 131 (93.04%) patients who were enrolled in this study, 4 (3.05%) patients defaulted on their treatment and were lost to follow-up; 1 (0.76%) patient died in the course of treatment and 126 (96.18%) completed the follow-up. Figure 1 demonstrates the details.
The demographic and clinical characteristics of the total cohort are presented in Table 1. The sample comprises of 101 (80.16%) males and 25 (9.94%) females with population mean (SD) age of 29.83 (9.93) ranging from 18 years to 70 years. The majority 78 (61.90%) of participants were single/never married, 82 (65.08%) attained primary education, 104 (82.54%) had non-formal occupation and 101 (80.16%) were living with care giver/family. One hundred and three (81.75%) had no known family history of mental illness, 37 (29.37%) of patients were having other psychotic disorders and 46 (36.51%) had less than three months of DUP.
| Variable | Mean (SD) | N (%) |
|---|---|---|
| Age (years) | 29.83 (9.93) | |
| 18 years-24 years | 50 (39.68%) | |
| 25 years-34 years | 45 (35.71%) | |
| 35 years-44 years | 18 (14.28%) | |
| 45 years-54 years | 11 (8.73%) | |
| 65+ years | 2 (1.59%) | |
| Age at the onset of illness, years | 28.75 (10.03) | |
| Sex | ||
| Male | 101 (80.16%) | |
| Female | 25 (9.94%) | |
| Marital status | ||
| Single/never married | 78 (61.90%) | |
| Married/conjugate | 34 (26.98%) | |
| Divorced/separated/widowed | 14 (11.11%) | |
| Education level | ||
| Primary education | 82 (65.08%) | |
| Secondary education | 19 (15.08%) | |
| Tertiary education | 14 (11.11%) | |
| No formal education | 11 (8.73%) | |
| Occupation | ||
| Formal employment | 3 (2.38%) | |
| Non-formal | 104 (82.54%) | |
| Unemployed/dependent | 14 (11.11%) | |
| Student | 5 (3.97%) | |
| Living arrangement | ||
| Alone | 10 (7.94%) | |
| Spouse | 25 (19.84%) | |
| Care giver/family | 101 (80.16%) | |
| Family history of mental disorder | ||
| No | 103 (81.75%) | |
| Yes | 23 (18.25%) | |
| Diagnosis at baseline | ||
| Schizophrenia | 25 (19.84%) | |
| Other psychotic disorder | 37 (29.37%) | |
| Major depressive disorder | 18 (14.29%) | |
| Bipolar disorder | 33 (26.19%) | |
| Substance induced psychosis | 13 (10.32%) | |
| Comorbid substance use disorder | 38 (30.16%) | |
| Cannabis | 18 (14.28%) | |
| Alcohol | 22 (17.46%) | |
| DUP | 5.63 (4.20) | |
| DUP | ||
| <3 months | 46 (36.51%) | |
| 3 months-6 months | 39 (30.95%) | |
| >6 months-12 months | 41 (32.54%) | |
| Baseline PANSS total | 139.85 (34.36%) | |
| Baseline MADRS total | 33.38 (10.11) | |
| Baseline YMRS total | 27.57 (10.77) | |
| Note: DUP=Duration of Untreated Psychosis; MDRS=Montgomery and Asberg Rating Scale; N=Sample size, PANSS=Positive and Negative Symptom Scale; SD=Standard Deviation; YMRS=Young Mania Rating Scale | ||
Table 1: Socio demographic and clinical profile of the patients with first episode psychosis at baseline (N=126).
The medications that were prescribed to the patients were categorized into five groups includes: Typical antipsychotic medications, atypical medications, antidepressant medications, mood stabilizer medications and adjunctive medications (Table 2). Typical antipsychotic medications were prescribed to 89.68% of patients whereby 96.46% with haloperidol, 3.54% with chlorpromazine. The atypical antipsychotic medications were prescribed to 10.31% of patients: 76.92% were under olanzapine and 23.08% with risperidone.
8.73% of patients were prescribed with antidepressant medications: 54.55% with amitriptyline and 45.45% with fluoxetine. 36.51% were prescribed with mood stabilizer medications: 97.83% with carbamazepine and 2.17% with sodium valproate. Furthermore, adjunctive medications were prescribed to 85.71% in addition to other medications: 97.22% with diazepam and 2.78% with promethazine.
| Medication | Percentage |
|---|---|
| Typical antipsychotic | 89.68 |
| Haloperidol | 96.46 |
| Chlorpromazine | 3.54 |
| Atypical antipsychotic | 10.31 |
| Olanzapine | 76.92 |
| Risperidone | 23.08 |
| Antidepressant medication | 8.73 |
| Amitriptyline | 54.55 |
| Fluoxetine | 45.45 |
| Mood stabilizer medication | 36.51 |
| Carbamazepine | 97.83 |
| Sodium valproate | 2.17 |
| Adjunctive medication | 85.71 |
| Diazepam | 97.22 |
| Promethazine | 2.78 |
Table 2: Medications prescribed to patients in the study.
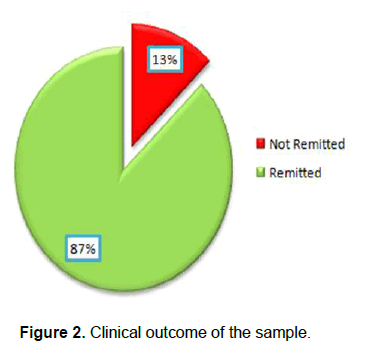
THE CLINICAL OUTCOME OF THE SAMPLE: Out of the 126 study participants, 110 remaining 16 (12.70%) patients did not achieve symptomatic remission. Figure 2 demonstrates this result.
Patients with symptomatic remission had relatively older age of onset of illness by (mean age: 29.80 (SD=10.42) compared to those who had no symptomatic remission 25.94 (SD=6.14). The large proportional of patients who achieved symptomatic remission was living with the care givers, followed by those who were living with spouse and those who were living alone. Table 3 shows the results in more details.
| Variable | No Symptomatic remission N (%) | Symptomatic remission N (%) | P-value |
|---|---|---|---|
| Age at onset, years | 25.94 (6.14) | 29.80 (10.42) | 0.152 |
| Sex | 0.734* | ||
| Female | 2 (8.33) | 22 (91.67) | |
| Male | 14 (13.73) | 88 (86.27) | |
| Marital status | 0.498* | ||
| Single/never married | 12 (15.19) | 67 (84.81) | |
| Married/conjugate | 2 (6.06) | 31 (93.94) | |
| Divorced/separated/widowed | 2 (14.29) | 12 (85.71) | |
| Education level | 0.704* | ||
| Primary education | 9 (10.98) | 73 (89.02) | |
| Secondary education | 2 (10.53) | 17 (89.47) | |
| Tertiary education | 3 (21.43) | 11 (78.57) | |
| No Formal education | 2 (18.18) | 9 (81.82) | |
| Occupation | 0.282* | ||
| Employed | 12 (11.32) | 94 (88.68) | |
| Unemployed/dependent | 4 (20.00) | 16 (80.00) | |
| Living arrangement | 0.005 | ||
| Alone | 0 (0.00) | 9 (100.00) | |
| Spouse | 0 (0.00) | 24(100.00) | |
| Care giver/family | 16 (17.20) | 77 (82.80) | |
| Family history of mental disorder | 0.300 | ||
| No | 15 (14.56) | 88 (85.44) | |
| Yes | 1 (4.35) | 22 (95.65) | |
| DUP | 4.89 (4.60) | 3.45 (3.96) | 0.187 |
| DUP, in group | 0.539 | ||
| <3 months | 5 (10.87) | 41 (89.13) | |
| 3 months-6 months | 4 (10.00) | 36 (90.00) | |
| >6 months-12 months | 7 (17.50) | 33 (82.50) | |
| Schizophrenia | 0.310 | ||
| No | 11 (10.89) | 90 (89.11) | |
| Yes | 5 (20.00) | 20 (80.00) | |
| Other psychotic disorder | 0.777 | ||
| No | 12 (13.48) | 77 (86.52) | |
| Yes | 4 (10.81) | 33 (89.19) | |
| Major depressive disorder | .700* | ||
| No | 13 (12.04) | 95 (87.96) | |
| Yes | 3 (16.67) | 15 (83.33) | |
| Bipolar disorder | 0.558 | ||
| No | 13 (13.98) | 80 (86.02) | |
| Yes | 3 (9.09) | 30 (90.91) | |
| Comorbid substance use disorder | 0.894 | ||
| No | 15 (13.27) | 98 (86.73) | |
| Yes | 1 (7.69) | 12 (92.31) | |
| Note: P values ≤ 0.05 indicates significance; *P is Fisher’s exact test | |||
Table 3: Clinical demographic of the sample, including those with symptomatic remission and those with no symptomatic remission after follow-up.
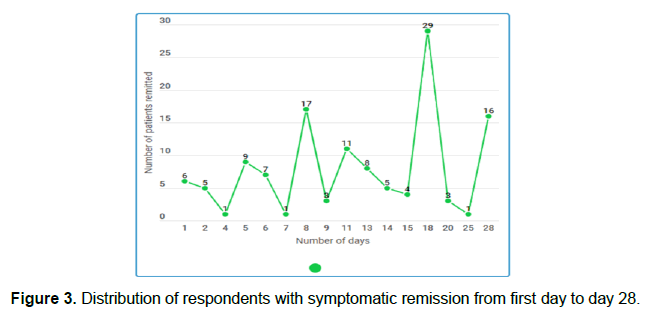
RATE AND TIME TO SYMPTOMATIC REMISSION: During a period of 28 days, patients achieved symptomatic remission at the mean duration of 13.39 (7.82) days. Among the subjects who achieved symptomatic remission; 26.36% achieved remission within seven days (week 1), while 40.0% within 14 days (week 2) and 32.73% within 21 days (week 3) and 0.91% within 28 days (week 4). Figure 3 demonstrates the distribution of the respondents.
PREDICTORS OF TIME TO SYMPTOMATIC REMISSION
UNIVARIATE COX REGRESSION ANALYSIS: The analysis was performed with each baseline explanatory variable for cox proportional hazard regression model (P ≤ 0.25) as shown in Table 4. The results indicate that being divorced/separated/widowed (HR=1.44, 95% CI=(0.94-2.21) increased the likelihood to symptomatic remission and being unemployed (HR=0.73, 95% CI=(0.43-1.24), living with a spouse (HR=0.32, 95% CI=(0.15-0.65) and having a DUP of 3 months-6 months (HR=0.69, 95% CI=0.44-1.09) reduced the likelihood to symptomatic remission at any time during the 28 days of treatment.
| Variable | Unadjusted analysis | Adjusted analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P value | aHR (95% CI) | P value | |
| Age of onset | 1.000 (0.998, 1.001) | 0.599 | ||
| Sex | ||||
| Female | Ref | |||
| Male | 1.009 (0.632, 1.611) | 0.969 | ||
| Marital status | ||||
| Single/never married | Ref | Ref | ||
| Married/conjugate | 1.202 (0.649, 2.228) | 0.557 | 0.848 (0.427, 1.684) | 0.637 |
| Divorced/separated/Widowed | 1.445 (0.942, 2.215) | .091* | 0.864 (0.430, 1.733) | 0.680 |
| Education level | ||||
| Primary education | 0.941 (0.470, 1.882) | 0.862 | ||
| Secondary education | 1.219 (0.543, 2.737) | 0.631 | ||
| Tertiary education | 0.712 (0.295, 1.722) | 0.451 | ||
| No formal education | Ref | |||
| Occupation | ||||
| Employed | Ref | Ref | ||
| Unemployed | 0.732 (0.431, 1.244) | .249* | 0.780 (0.448, 1.361) | 0.382 |
| Living arrangement | ||||
| Alone | Ref | Ref | ||
| Spouse | 0.321 (0.157, 0.656) | .001* | 0.311 (0.139, 0.697) | .004** |
| Care giver/family | 0.645 (0.298, 1.399) | 0.267 | 0.701 (0.233, 2.107) | 0.526 |
| Family history of mental disorder | ||||
| No | Ref | |||
| Yes | 1.072 (0.672, 1.712) | 0.77 | ||
| Duration of untreated psychosis | ||||
| <3 | Ref | Ref | ||
| 03 months-06 months | 0.699 (0.445, 1.096) | .118* | 0.650 (0.409, 1.035) | .069** |
| >6 months | 0.777 (0.491, 1.231) | 0.283 | 0.702 (0.439, 1.125) | 0.141 |
| Schizophrenia | ||||
| No | Ref | |||
| Yes | 0.977 (0.601, 1.586) | 0.923 | ||
| Other psychotic disorder | ||||
| No | Ref | |||
| Yes | 0.916 (0.609, 1.378) | 0.674 | ||
| Major depressive disorder | ||||
| No | Ref | |||
| Yes | 1.025 (0.594, 1.768) | 0.928 | ||
| Bipolar disorder | ||||
| No | Ref | |||
| Yes | 1.148 (0.630, 2.094) | 0.651 | ||
| Substance use disorder | ||||
| No | Ref | |||
| Yes | 1.035 (0.680, 1.575) | 0.872 | ||
| Typical antipsychotic medication | ||||
| No | Ref | |||
| Yes | 1.337 (0.717, 2.495) | 0.361 | ||
| Atypical antipsychotic medication | ||||
| No | Ref | |||
| Yes | 0.748 (0.401, 1.395) | 0.342 | ||
| Antidepressant medication | ||||
| No | Ref | |||
| Yes | 1.355 (0.707, 2.596) | 0.36 | ||
| Mood stabilizer medication | ||||
| No | Ref | |||
| Yes | 0.790 (0.536, 1.163) | 0.291 | ||
| Note: *P value ≤ 0.25; **P value ≤ 0.05; Presence of * or ** indicates significance at unadjusted and adjusted analysis respectively | ||||
Table 4: Univariate and multivariate cox regression analysis of predictors of symptom remission.
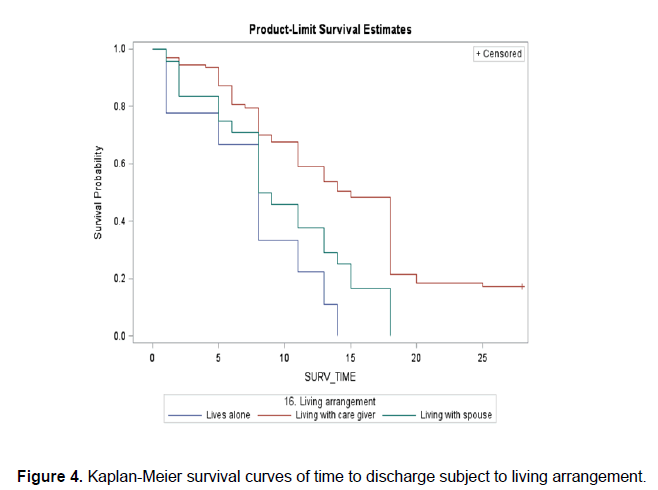
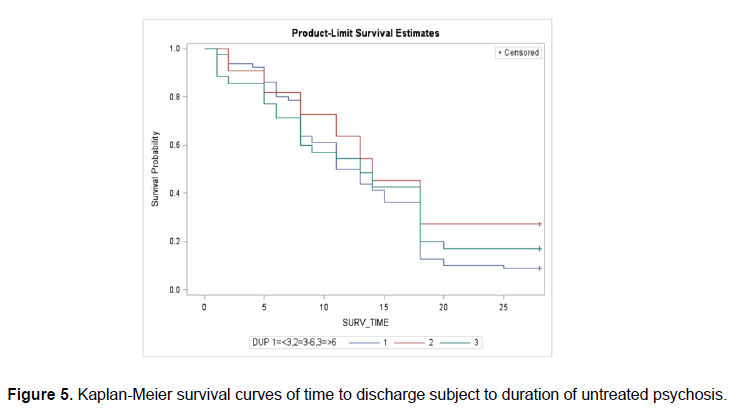
MULTIVARIATE COX REGRESSION ANALYSIS: Under adjusted analysis no independent factor was significantly associated with increased likelihood of symptomatic remission as demonstrated in Table 4. Two independent predictors are shown to be associated with reduced likelihood of symptomatic remission: Living with spouse (aHR)=0.31, 95% CI=(0.13-0.69) relative to “living alone” and DUP of 3 months-6 months (aHR)=0.65, 95% CI=(0.40-1.03) relative to DUP of less than three months. Figure 4 shows the survival curves of time to discharge of patients to living arrangement and Figure 5 shows the survival curves of the time to discharge of the patients to DUP.
DISCUSSION
This is the first study in Tanzania to assess the predictors of symptomatic remission in early treatment among patients with FEP. First, 87.30% of subjects achieved symptomatic remission at the mean time of 13.39 (7.82) days with 28 days of treatment. Second, living with the spouse was independently associated with reduced likelihood symptomatic remission within 28 days of treatment of FEP. Finally, longer DUP was independently associated with prolonged time to symptomatic remission among patients with FEP during 28 days of follow-up.
These findings are consistent with many previous reports on demographic and clinical characteristics of patients presenting with FEP. The remission rate in this study is higher compared to study that was done in Turkey in a 4 week follow-up that presented with 40.7% at the end point (Yildiz). The higher rate of remission of this study is relevant to findings of other studies particularly in Africa and that has been accounted due to use stringent inclusion criteria of definition of remission, having longer average periods of follow-up, studies that are done recently and results of early interventions to patients with FEP, however, this study has been done in a short period of follow-up (Lally).
Other factors that define high remission rate of symptoms might include methodological differences or regional variations and service level confounds (Kaminga). Early treatment response, baseline severity of psychopathological symptoms and subjective well-being of patients were as well linked to prediction of early remission of symptoms (Emsley). The biological markers among people with FEP have been found to influence response to antipsychotic medications and predicting side effects that may dictate and increase early remission of symptoms; however, still there are no data in Africa setting that support of the knowledge (Campbell, et al.). Hence, more studies need to investigate factors that define and predict higher remission in our setting.
The multivariate cox regression analysis revealed no any independent variable to be significant predictor of symptomatic remission of FEP. However, the patients who were living with their spouses had 0.31 decreased likelihood of remission of symptoms (aHR=0.31, 95% CI=(0.14-0.70) relative to “living alone”. Patients with longer DUP, 3-6 months (aHR=0.70, 95% CI=(0.44-1.10) had decreased likelihood of remission of symptoms relative to those with less than three months of DUP.
This study, opposite to other studies has shown that living with a spouse decreased likelihood of symptomatic remission. Living with relatives/family members or an adult including a spouse in the household has been significantly associated with attainment of symptomatic remission (Alem, et al.). This is because living arrangement is associated with social ties that provide social support that modulates stressors for mental health disorders or accessing support for mental health care (Breier). Social support particularly the emotional support from close relationship including spouses has been found to be a key protective factor against mental disorders but also helps in accessing treatment and adherence to medications and hence, remission of symptoms (Gomes-Villas Boas). Consequently, living with a spouse might have needed social support to enhance response to antipsychotic medications and improving remission of symptoms. The support system that might be there when living with the spouse may no longer be sustained or cease to be effective and patients will be more unlikely to achieve response to medications (Robinson). This is to mean, social support when living with a spouse may play a crucial role in helping patients with FEP achieve early symptomatic remission. Therefore, psychological interventions and social support along prescription of antipsychotic medications are recommended to improve better response to patients with FEP (Kaminga).
Longer DUP has been associated with lower chance of treatment and reported to be a significant predictor of poor symptomatic remission as observed in this study and other studies as well (Demjaha, et al.). This is because longer DUP contributes to biological toxic effect, causing poorer outcome of illness due to deteriorating brain functions and as well presentation of severe psychotic symptoms including negative symptoms at the initiation of antipsychotic medications that delayed remission of symptoms in the course of treatment. Having lower level of social and other domains of premorbid functions have been associated with longer DUP as well and in other direction this is contributed by the effects of psychotic disorders on deteriorating of individual function from childhood (Jeppesen, et al.). However, a study by Malla presents a contradicting outcome by finding that DUP was not associated with symptomatic remission particularly of negative nature which might be affected with type of antipsychotic medication used and if the negative symptoms are result of other psychotic disorder. DUP was as well found to have no significant association with remission of symptoms when analyzed using bivariate approach which potentially introducing a methodological variation. Nevertheless, substantial mechanisms for reductions of DUP especially at early stages of psychosis are needed to be studies and implemented including cognitive, restructuring processes, regulation of mesolimbic dopaminergic system to intervene and achieve remission of symptoms of people with FEP (Caneja D, et al.). Moreover, marital status has been shown to alter the effect of longer DUP on symptomatic remission due to the fact that marriage provided adequate social support that helped as a protective factor to mental health and also adherence to antipsychotic medications and improve remission of symptoms to patients with FEP. Therefore, patients with FEP and longer DUP need social support from spouse or close relationship such as family members to enhance their response to antipsychotic medications and early remission of symptoms (Kaminga, et al.).
CONCLUSION
In this cohort study of 126 patients with FEP, report has produced that 87.30% of patients with FEP achieve symptom remission. Multivariate analysis revealed no independent predictor of symptomatic remission of FEP. However, two predictors; living with a spouse and longer DUP have been associated with reduced likelihood of symptomatic remission. Living with a spouse with no adequate social support including emotional support and treatment support do contribute to having no protection against mental disorders and poor prognosis of psychosis and hence, unlikely to achieve early symptomatic remission. Longer DUP has been associated with poorer symptomatic remission due to its impact in prognosis of psychosis among individuals. However, social support has been shown to alter the impact of longer DUP to remission of symptoms due to increased response to antipsychotic medications and hence, enhance early achievement of remission of symptoms.
Therefore, this study supports the idea of including psychosocial interventions and social support fromspouse, care giver and f amily members in relation to prescription of medications and may improve better response to medications and achieve quicker remission of symptoms even with short period of 28 days after initiation of treatment. This study sets a background for more studies to be done on predictive value of social support to symptomatic remission among patients with FEP and tailored early intervention that address this confounding factor.
LIMITATIONS
This study has several strengths: Being a first study of this nature has set a ground by sharing information for other studies to be done in the area of predictors of FEP in Tanzania. A longitudinal follow-up, a cohort with a good representativity, low attrition during follow-up, use of validated psychometric instruments. However, the sample had to be large to raise strong evidence of correlation of the predictors.
ETHICAL ISSUES
Ethical approval was sought from university of Dodoma research and ethics committee and permission to conduct the research at Mirembe mental health hospital was sought from hospital management and obtained respectively. The patients and/or their relatives consented to the follow-up procedure. The conduct during the study adhered to the Helsinki declaration.
COMPETING INTERESTS
The authors declare that they have no competing interests.
ACKNOWLEDGEMENT
Acknowledging the support and supervision of staff of department of psychiatry, school of medicine and dentistry at university of Dodoma and hospital administration of Mirembe mental health hospital. Also the contribution of the ministry of health in united republic of Tanzania on funding the work.
References
- Abbo C (2012) Naturalistic outcome of treatment of psychosis by traditional healers in Jinja and Iganda districts, Eastern Uganda 3 months-6 months follow up. Int J Ment Health Syst, 6: 13
[Crossref] [Google Scholar] [PubMed]
- Akena D (2020) Clinical outcomes among individuals with a first episode psychosis attending Butabika national mental referral hospital in Uganda: A longitudinal cohort study. A study protocol for a longitudinal cohort study. BMJ Open, 10: e034367.
[Crossref] [Google Scholar] [PubMed]
- Alem, A (2009) Clinical course and outcome of schizophrenia in a predominantly treatment naive cohort in rural Ethiopia. Schizophr Bull, 35: 646-654.
[Crossref] [Google Scholar] [PubMed]
- Anath J (1978) Prediction of lithium response in affective disorders. J Clin Psychiatry, 39: 95-100.
[Google Scholar] [PubMed]
- Ang MS, Rekhi G, Lee J (2021) Associations of living arrangements with symptoms and functioning in schizophrenia. BMC Psychiatry, 21: 497.
[Crossref] [Google Scholar] [PubMed]
- Bozzatello P, Bellino S, Rocca P (2019) Predictive factors of treatment resistance in first episode of psychosis: A systematic review. Front Psychiatry, 10: 67.
[Crossref] [Google Scholar] [PubMed]
- Brown E, Bedi G, McGorry P, O’Donoghue B (2020) Rates and predictors of relapse in first episode psychosis: An Australian cohort study. Schizophr Bull Open, 1: sgaa017.
- Campbell MC, Tishkoff SA (2008) African genetic diversity: Implications for human demographic history, modern human origins and complex disease mapping. Ann Rev Genomics Hum Genet, 9: 403-433.
[Crossref] [Google Scholar] [PubMed]
- Caton CL, Hasin DS, Shrout PE, Drake RE, Dominguez B, et al (2006) Predictors of psychosis remission in psychotic disorders that co-occur with substance use. Schizophr Bull, 32: 618-625.
[Crossref] [Google Scholar] [PubMed]
- Crespo-Facorro B, Pelayo-Terán JM, Pérez-Iglesias R, Ramírez-Bonilla M, Martínez-García, et al. (2006) Predictors of acute treatment response in patients with a first episode on non-affective psychosis: Sociodemographics, premorbid and clinical variables. J Psychiatr Res, 41: 659-666.
[Crossref] [Google Scholar] [PubMed]
- Crumlish N, Whitty P, Clarke M, Browne S, Kamali M, et al. (2018) Beyond the critical period: Longitudinal study of 8-year outcome in first episode non-affective psychosis. Br J Psychiatry, 194: 18-24.
[Crossref] [Google Scholar] [PubMed]
- Demjaha A, Lappin JM, Stahl D, Patel MX, MacCabe JH, et al. (2017) Antipsychotic treatment resistance in first episode psychosis: Prevalence, subtypes and predictors. Psychol Med, 47: 1981-1989.
[Crossref] [Google Scholar] [PubMed]
- Díaz I, Pelayo-Terán JM, Pérez-Iglesias R, Mata I, Tabarés-Seisdedos R, et al. (2012) Predictors of clinical remission following a first episode of non-affective psychosis: Sociodemographics, premorbid and clinical variables. Psychiatry Res, 206: 181-187.
[Crossref] [Google Scholar] [PubMed]
- Di Capite S, Upthegrove R, Mallikarjun (2016) The relapse rate and predictors of relapse in patients with first episode psychosis following discontinuation of antipsychotic medication. Early Interv Psychiatry, 12: 893-899.
[Crossref] [Google Scholar] [PubMed]
- Emsley R (2009) New advances in pharmacotherapy for early psychosis. Early Interv Psychiatry, 3: S8-S12.
[Crossref] [Google Scholar] [PubMed]
- Emsley R, Chiliza B, Asmal L, Lehloenya K (2011) The concepts of remission and recovery in schizophrenia. Curr Opin Psychiatry, 24: 114-121.
[Crossref] [Google Scholar] [PubMed]
- Fraguas D, De Castro MJ, Medina O, Parellada M, Moreno D, et al (2008). Does diagnostic classification of early onset psychosis change over follow-up? Child Psychiatry Hum Dev, 39: 137-145.
[Crossref] [Google Scholar] [PubMed]
- Fond G, d’Albis MA, Jamain S, Tamouza R, Arango C, et al. (2015) The promise of biological markers for treatment response in first episode psychosis: A systematic review. Schizophrenia Bull, 41: 559-573.
[Crossref] [Google Scholar] [PubMed]
- Gallego JA, Robinson DG, Sevy SM, Napolitano B, McCormack J, et al. (2011) Time to treatment response in first episode schizophrenia: Should acute treatment trials last several months? J Clin Psychiatry, 72: 1691-1696.
[Crossref] [Google Scholar] [PubMed]
- Huber CG, Naber D, Lambert M (2008) Incomplete remission and treatment resistance in first episode psychosis: Definition, prevalence and predictors. Expert Opin Pharmacother, 9: 2027-2038.
[Crossref] [Google Scholar] [PubMed]
- Hyman SE (2000) The genetics of mental illness: Implications for practice. Bull World Health Organ, 78: 455-463.
[Google Scholar] [PubMed]
- Jaeger M, Laux G, Pfeiffer H, Naber D, Schmidt LG, et al. (2009) Early improvement as a predictor of remission and response in schizophrenia: Results from a naturalistic study. Eur Psychiatry, 24: 501-506.
[Crossref] [Google Scholar] [PubMed]
- Jenkins R, Mbatia J, Singleton N, White B (2010) Prevalence of psychotic symptoms and their risk factors in urban Tanzania. Int J Environ Res Public Health, 7: 2514-2525.
[Crossref] [Google Scholar] [PubMed]
- Jeppesen P, Petersen L, Thorup A, Abel MB, Krarup G, et al. (2008) The association between pre-morbid adjustment, duration of untreated psychosis and outcome in first episode psychosis. Psychol Med, 38: 1157-1166.
[Crossref] [Google Scholar] [PubMed]
- Kanahara N, Yamanaka H, Suzuki T, Takase M, Iyo M (2018) First episode psychosis in treatment resistant schizophrenia: A cross sectional study of a long term follow-up cohort. BMC Psychiatry, 18: 274.
[Crossref] [Google Scholar] [PubMed]
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Usage
- Total views: 1480
- [From(publication date): 0-2023 - Nov 27, 2025]
- Breakdown by view type
- HTML page views: 1137
- PDF downloads: 343