Predictive Validity of Lumbar X-ray Images and MRIs for Chronic Low Back Pain Subtypes
Received: 14-May-2018 / Accepted Date: 21-May-2018 / Published Date: 28-May-2018 DOI: 10.4172/2167-0846.1000321
Abstract
Purpose: The aim of this observational study alongside our inter-rater reliability trial (ISRCTN 43417727) is to investigate the accuracy of lumbar X-ray images and MRIs as diagnostic tools of low back pain (LBP) subtypes (sacroiliac joint, disc and facet joint).
Patients and methods: Included were patients aged 18 or more with medical history and physical examination suggestive of a chronic LBP subtype, followed by a diagnostic test block. Numbers of spinal imaging tests, and whether or not pathology was present was evaluated in patients with positive- as well as negative diagnostic test blocks. The sensitivity, specificity, positive and negative predictive value of the lumbar X-ray images and MRIs discriminating between the three LBP subtypes are presented.
Results: One hundred patients were included. Facet joint pain was a general working diagnosis in 40 patients, disc pain in 8 patients and SI joint pain in 35 patients. The positive predictive value of X-ray was 82.6% for facet joint pain, 66.7% for disc pain and 60% for SI joint pain; the negative predictive value of X-ray was 50% for facet joint pain, 66.7% for disc pain and 7.7% for SI joint pain. The positive predictive value of MRI was 81.8% for facet joint pain, 50% for disc pain and 0% for SI joint pain; the negative predictive value of MRI was 55.6% for facet joint pain, 0% for disc pain and 13% for SI joint pain.
Conclusion: The predictive validity of lumbar X-ray images and MRIs to distinguish between low back pain subtypes in patients with chronic LBP is questionable.
Keywords: Low back pain; Sacroiliac joint; Intervertebral disc; Facet joint
Introduction
Low back pain (LBP) continues to be a very common problem globally and will increase in prevalence over the next years [1,2]. Low back pain causes more disability than any other condition and ranks highest in terms of disability and sixth in terms of overall burden [2,3]. Besides its negative impact on physical functioning and the quality of life, treatment of LBP is costly; 2% of all physician office visits are for low back pain complaints [4]. Aging affects the spinal elements and causes a certain degree of degeneration, resulting in changes such as a reduction of disc height and altered load transmission across the vertebral endplates and paired facet joints (the three-joint spinal complex) [5]. Identification of the pain-producing structure is not easy in degenerative spinal disease.
The intervertebral disc, facet joint and sacroiliac (SI) joint can act as a major cause of chronic low back pain and referred pain. The prevalence of internal disc disruption, facet joint pain and SI joint pain was 39-42%, 15-31% and 10-38%, respectively; the younger the patient, the more likely LBP is discogenic in origin [6-11].
We recently have investigated the effect on pain reduction and global perceived effect (GPE) of a percutaneous radiofrequency (RF) heat lesion compared to a sham procedure, applied to the ramus communicans [12], the medial branch of the primary dorsal ramus [13] and the dorsal ramus of L5 and lateral branches of the S1, S2, S3 and S4 nerve roots [14]. Based on the results of the sham-controlled trials we asked ourselves what is known about the diagnostic accuracy of the physical examination, X-ray images and MRIs in diagnosing chronic low back pain subtypes.
The inter-rater reliability of diagnostic tests that point towards SI joint, disc or facet joint pain was investigated in a subsequent study [15]. Judging from spinal imaging tests whether the cause of chronic LBP is due to intervertebral disc degeneration, facet arthritis, or SI arthritis can be challenging [16]. When determining the association between deviations on spinal imaging and LBP, the research data yield conflicting results. Patients with disc herniations may have no symptoms [17-20], while patients with severe symptoms demonstrated no evidence on imaging of nerve root compression at all [21-23].
The severity of symptoms is not well correlated with the size of the herniation [24-27] and features on imaging may have little prognostic value towards outcome [28-32]. Routine imaging can be associated with radiation exposure, increased expenses and possibly unnecessary procedures [33]. Patient expectations and increasing satisfaction may play a role. Clinical practice guidelines for the diagnosis and treatment of LBP have been developed in the past [34]. Appropriateness criteria for LBP were issued by the American College of Radiology (1996, last revision 2011) [35].
The aim of this study is to investigate the accuracy of lumbar X-ray images and MRIs as diagnostic tools of LBP subtypes (SI joint, disc and facet joint). Whether or not abnormalities were visible on the spinal imaging tests was judged by a radiologist and a pain physician.
Materials and Methods
We conducted an observational study alongside the inter-rater reliability trial (International Standard Randomized Controlled Trial Number Register (Current Controlled Trials) 43417727) to investigate the accuracy of lumbar X-ray images and MRIs as diagnostic tools of LBP subtypes. Patients who were referred because of their chronic LBP received three separate consultations (two from experienced pain physicians and one from an experienced orthopedic surgeon) within a period of two weeks to decrease the chance for confounding and jointly determine the cause of the pain problem. Findings from the physical examination [36-40] suggestive of a SI joint, disc or facet joint pain problem are presented in Table 1.
| Physical examination | SI | Disc | Facet |
|---|---|---|---|
| Drop-test positive | Yes | ||
| Sitting exam shows no reflex, motor or sensory signs in the legs | Yes | ||
| Straight leg raising (Lasegue) negative between 30 and 70 degrees of passive flexion | Yes | ||
| Distraction (Gapping) test positive | Yes | ||
| Posterior shear (thigh trust) test positive | Yes | ||
| Pelvic torsion (Gaenslen’s) test positive | Yes | ||
| Patrick-Faber test positive | Yes | ||
| Compression test positive | Yes | ||
| Sacral thrust test positive | Yes | ||
| Cranial shear test positive | Yes | ||
| Bilateral internal rotation of the hip / Unilateral rotation of the hip painful at SI joint(s) | Yes | ||
| Yeoman’s test positive | Yes | ||
| Gait deviation | Yes | ||
| Abnormal sensory and motor examination, hyperactive or diminished reflexes | Yes | ||
| Digital Interspinous Pressure (DIP) test positive | Yes | ||
| Straight leg raising (Lasegue) positive between 30 and 70 degrees of passive flexion | Yes | ||
| Pain in extension | Yes | ||
| Pain eased in flexion | Yes | ||
| Pain when rising from forward flexion | Yes | ||
| Schober test <3-5 cm | Yes | ||
| Pain in extension, lateral flexion or rotation manoeuvers to the ipsilateral side | Yes | ||
| Replication or aggravation of pain by unilateral or bilateral pressure over the facet joints or transverse process | Yes | ||
| Local unilateral or bilateral passive movements show reduced range of motion or increased stiffness on the side of the involved facet joints | Yes | ||
| Tight or facilitated muscles (psoas, hip adductors, gluteus medius muscles) | Yes | ||
| Weak muscles (gluteus maximus, gluteus medius) | Yes |
Table 1: Findings from the physical examination suggestive of a Si joint, disc or facet joint problem [36-40].
A training session was held before the study to ensure as much consistency as possible of methods and standardization of test procedures, during which every item from the list with diagnostic criteria were judged on their presence or absence. Medical history was noted, along with the results from spinal imaging.
Patients suspected of a lumbar spine related pain disorder who met the inclusion (age ≥ 18 years, chronic (>3 months) LBP) and exclusion criteria (presence of red flags [41], progressive neurological deficits, major psychiatric disorder (according to psychiatrists opinion), pain in other parts of the body that is more severe, pregnancy, active infection, communication (language) difficulties (according to physicians opinion) were eligible for inclusion. If the working diagnoses from the three physicians were in agreement with each other, a general working diagnosis was made, after which a diagnostic test block (gold standard) was performed:
1) Diagnostic SI joint test block
The injection was performed under fluoroscopy with a 10 cm Sluijter-Mehta Kit (SMK) needle (Cotop® via Neurotherm®, Wilmington, Massachusetts, United States). The patient lies in the prone position on the operating table with a pillow under the pelvis. From the anteroposterior (AP) view, the c-arm is rotated contralaterally until the medial cortical line of the posterior articulation is in focus. Local anesthesia with 1 mL lidocaine 2% was given for skin infiltration. Needle insertion is 1-2 cm cranially from the lower border of the SI joint at the level of the zone of maximal radiographic translucency. Introduction of the needle into the SI joint is characterized by a change in resistance. On a lateral view, the needle tip should appear anterior to the dorsal border of the sacrum. The SI joint was injected with a total of 3 mL lidocaine 2%.
2) Diagnostic test block at the ramus communicans
The injection was performed under fluoroscopy with 15 cm Sluijter- Mehta Kit (SMK) needles (Cotop® via Neurotherm®, Wilmington, Massachusetts, United States). The patient lies prone on the operating table with a pillow under the abdomen to flatten the lumbar lordosis. From the AP view, the c-arm is rotated obliquely to the ipsilateral side so that facet joints are projected away and the vertebral column is clearly visible. From the sagittal plane, the c-arm is rotated to let the transverse process change its location relative to the vertebral body and, as a result, the axis of the transverse process lies slightly above the middle of the vertebral body.
The injection point is marked just caudally to the transverse process and somewhat medially to the lateral border of the vertebral body. Local anesthesia with 1 mL lidocaine 2% was given for skin infiltration. The needle is advanced until contact is made with the vertebral body. On the lateral view, the tip of the needle should be somewhat ventral to the posterior side of the lateral body. After sensory (50 Hz) and motor (2 Hz) stimulation as an adjunct to confirm correct needle placement, the ramus communicans was surrounded with a total of 0.5 mL lidocaine 2%.
3) Diagnostic test block at the medial branch of the primary dorsal ramus
The injection was performed under fluoroscopy with three 10 cm Sluijter-Mehta Kit (SMK) needles (Cotop® via Neurotherm®, Wilmington, Massachusetts, United States of America) at the facet joint that was presumed to be the source of the pain and then at the two adjacent levels (in the case of the L5/S1 facet joint level, the adjacent L4/L5 facet joint level was also treated).
The patient lay prone on the operating table with a pillow under the abdomen in order to flatten the lumbar lordosis. From the AP view, the c-arm was rotated obliquely to the ipsilateral side so that the junction between the superior articular process and the transverse process was more easily accessible. Local anesthesia with 1 mL lidocaine 2% per level was given for skin infiltration. Contact was made with the transverse process as close as possible to the superior articular process.
After contacting bone, the needle was advanced slightly in a cranial direction so that its tip slides over the transverse process. In the lateral view the electrode tip lay at the base of the superior articular process at the lower aspect of the intervertebral foramen, approximately 1 mm dorsal to its posterior border. After sensory (50 Hz) and motor (2 Hz) stimulation (contraction of the ipsilateral multifidus muscle and excluding a too close proximity to the segmental nerve), each medial branch was surrounded with a total of 0.5 mL lidocaine 2%.
The diagnostic test injection was evaluated using the Numerical Rating Scale (NRS, 0-10 point scale) for pain [42-48]. When employing the NRS for pain patients are asked to rate their pain on a scale from 0 to 10, where 0 represents "no pain" and 10 represents "the worst pain possible," using whole numbers (11 integers including zero); if the decrease in NRS was equal to or greater than 2, the test was called positive [42].
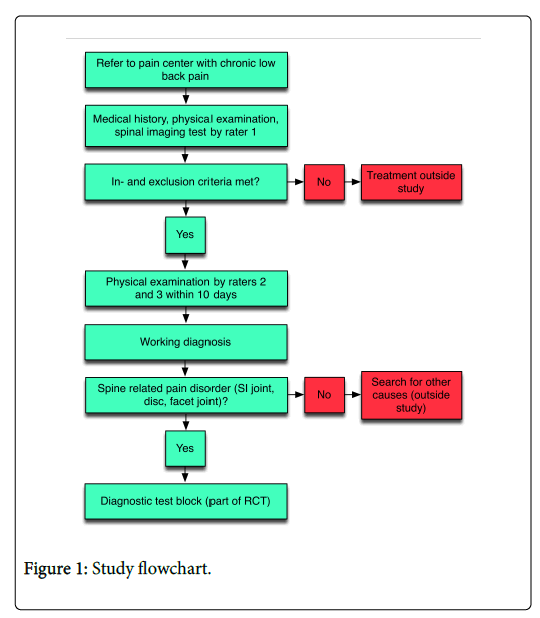
Numbers of spinal imaging tests were noted for the entire sample and LBP subtypes. The presence of abnormalities on each lumbar spinal imaging test was judged by a radiologist as well as a pain physician; presence itself was assumed when at least one physician described it. The study flowchart is presented in Figure 1. The medical ethics committee from the Erasmus MC University Medical Center approved the protocol (reference number MEC-2011-246). Written informed consent was obtained from all patients. The predictive validity of X-ray images and MRIs in patients with a diagnosis of a LBP subtype (SI joint, disc and facet joint) was determined by assessing the sensitivity, specificity, positive and negative predictive value. Data were analyzed using SPSS for Mac, version 22 (International Business Machines (IBM) Corporation, Software Group, Route 100, Somers, NY, 10589, United States of America).
Results
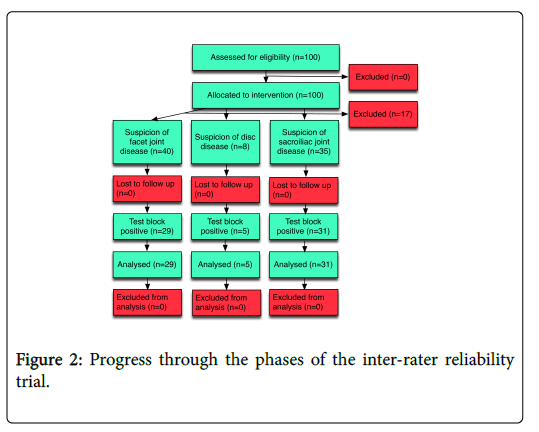
One hundred patients were included between January 2013 and April 2014. Demographic data of the patients were a median age of 55 (interquartile range (75,25) 65.75-44.25), a mean BMI of 26.8 (standard deviation 5.6), 66% female gender and 100% Caucasian race. The progress through the phases of the inter-rater reliability study is presented in Figure 2. Numbers of lumbar spinal imaging tests for the entire sample as well as for the LBP subtypes (before the diagnostic test block) are presented in Table 2.
| Group (before test block) | Nr | X-ray made | CT made | MRI made |
|---|---|---|---|---|
| Total | 100 | 90 (90%) | 2 (2%) | 61 (61%) |
| Facet joint | 40 | 37 (92.5%) | 2 (2%) | 20 (50%) |
| Disc | 8 | 6 (75%) | 0 (0%) | 6 (75%) |
| Sacroiliac joint | 35 | 31 (88.6%) | 0 (0%) | 23 (65.7%) |
Table 2: Total number of spinal imaging techniques, as well as for each subtype (differential diagnosis).
Lumbar X-ray imaging was used in 90% of the patients in the sample, MRI in 61%. No general working diagnosis could be made in 17 patients; these patients were excluded from the study. Deviations present on lumbar X-ray imaging for each LBP subtype, and including the outcome of the diagnostic test block are presented in Table 3.
| Group | Nr | X-ray made (%) | Facet joint pathology present (%) | Disc pathology present (%) | Sacroiliac joint pathology present (%) |
|---|---|---|---|---|---|
| Facet joint (test block positive) | 29 | 26 (89.6) | 19 (73.1) | 23 (88.5) | 1 (3.8) |
| Facet joint (test block negative) | 11 | 11 (100) | 4 (36.4) | 9 (81.2) | 0 (0) |
| Disc (test block positive) | 5 | 3 (60) | 1 (33.3) | 2 (66.7) | 0 (0) |
| Disc (test block negative) | 3 | 3 (100) | 1 (33.3) | 1 (33.3) | 0 (0) |
| Sacroiliac joint (test block positive) | 31 | 27 (87.1) | 16 (59.2)1 | 18 (66.7)1 | 3 (11.1) |
| Sacroiliac joint (test block negative) | 4 | 4 (100) | 4 (100) | 4 (100) | 2 (50) |
Table 3: Pathology present on x-ray for each subtype of low back pain, depending on the outcome of the test block. (1: 1 missing data entry).
When the facet joint was considered to be the primary source of pain and the diagnostic test block was positive (decrease in numerical rating scale for pain of 2 or more on a 0-10 point scale [42]), facet joint abnormalities were seen on X-ray imaging in 73.1%, disc abnormalities (in these same patients) in 88.5%. Deviations present on lumbar MRI for each LBP subtype, and including the outcome of the diagnostic test block are presented in Table 4.
| Group | Nr | MRI made | Facet joint pathology present (%) | Disc pathology present (%) | Sacroiliac joint pathology present (%) |
|---|---|---|---|---|---|
| Facet joint (test block positive) | 29 | 13 (44.8) | 9 (69.2) | 13 (100) | N/A |
| Facet joint (test block negative) | 11 | 7 (63.4) | 2 (28.6) | 6 (85.6) | N/A |
| Disc (test block positive) | 5 | 3 (60) | 2 (66.7) | 3 (100) | N/A |
| Disc (test block negative) | 3 | 3 (100) | 0 (0) | 3 (100) | N/A |
| Sacroiliac joint (test block positive) | 31 | 20 (64.5) | 9 (45) | 20 (100) | 0 (0)1 |
| Sacroiliac joint (test block negative) | 4 | 3 (75) | 1 (33.3) | 3 (100) | 0 (0)2 |
Table 4: Pathology present on MRI for each subtype of low back pain, depending on the outcome of the test block. [1: 17 missing data entries; 2: 3 missing data entries (MRI of lumbar spine)].
Disc abnormalities were present in almost 100% of cases, irrespective of the results from the diagnostic test block and the general working diagnosis. The sensitivity, specificity, positive and negative predictive value of X-ray imaging in the population with chronic LBP and in each LBP subtype is presented in Table 5, these of MRI in Table 6.
| X-ray | ||||
|---|---|---|---|---|
| Sensitivity (%) | PPV (%) |
Specificity (%) | NPV (%) |
|
| Facet joint | 73.1 | 82.6 | 63.6 | 50 |
| Disc | 66.7 | 66.7 | 66.7 | 66.7 |
| Sacro-iliac joint | 11.1 | 60 | 50 | 7.69 |
Table 5: Sensitivity, specificity and predictive validity of lumbar spinal X-ray. Abbreviations: PPV=Positive Predictive Value; NPV=Negative Predictive Value.
| MRI | ||||
|---|---|---|---|---|
| Sensitivity (%) | PPV (%) |
Specificity (%) | NPV (%) |
|
| Facet joint | 69.2 | 81.8 | 71.4 | 55.6 |
| Disc | 100 | 50 | 0 | 0 |
| Sacro-iliac joint | 0 | 0 | 100 | 13 |
Table 6: Sensitivity, specificity and predictive validity of lumbar spinal MRI scan. Abbreviations: PPV=Positive Predictive Value; NPV=Negative Predictive Value.
The positive predictive value of lumbar X-ray imaging for facet joint pain was 82.6%, the negative predictive value 50%. The positive predictive value of MRI for disc pain was 50%, the negative predictive value 0%. During the study we recorded no adverse events.
Discussion
This trial investigated the sensitivity, specificity and predictive value of X-ray and MRI in respect to the effectiveness of the diagnostic test block in patients in whom medical history and physical examination point towards a LBP subtype (SI joint, disc or facet joint). The results of this study show that the predictive validity of the lumbar spinal images in distinguishing between LBP subtypes is questionable. Anatomic changes normally occur as a result from aging and have the potential of producing mechanical and clinical symptoms. Loss of disc height alters the transmission of loads across structures like the facet joints, increasing further loading on adjacent structures. Establishing an accurate diagnosis of the specific source of low back pain will help in directing (or avoiding) treatment towards the source of the symptoms.
In the population without low back pain, the percentage of people with disc abnormalities varied between 31 and 64% [24,25], while in this sample the prevalence of disc abnormalities in the patients with LBP was 100%, irrespective of the general working diagnosis. Furthermore, facet abnormalities were seen in 8% of people without LBP [24], but increased to 69.2% in the sample of patients with LBP when a working diagnosis of facet joint pain was established. From the MRI studies in people with and without low back pain we know that the high prevalence of disc abnormalities, combined with the high prevalence of back pain, bulging discs and protrusions of the disc may frequently be coincidental [13-16, 20-23]; therefore, in chronic LBP, disc abnormalities cannot be used to distinguish one LBP type from the other. A limitation of this study is that during the first consultation the pain physician took into account the results from lumbar spinal imaging, i.e. to exclude red flags. Perhaps this moment biased our results in moving more specifically towards a LBP subtype. There were relatively few individuals under the age of 40 present in the study. This limits the interpretation and generalizability of the study findings.
Conclusion
We conducted this study to investigate the accuracy of lumbar X-ray imaging and MRIs as diagnostic tools of LBP subtypes (SI joint, disc and facet joint). Based on the results from this study, the predictive validity of lumbar X-ray imaging and MRIs to distinguish between LBP subtypes in patients with chronic LBP is questionable.
Acknowledgements
This manuscript also serves as part of the PhD thesis of the first author on minimally invasive treatment for lumbar spine related pain disorders.
Disclosure
All authors declare that no support from any organization for the submitted work has been received, no financial relationships with any organizations have been established that might have an interest in the submitted work and no other relationships or activities were established that could appear to have influenced the submitted work.
References
- Walker BF (2000) The prevalence of low back pain: A systematic review of the literature from 1966 to 1998. J Spinal Disord 13: 205-217.
- Hoy D, Bain C, Williams G, March L, Brooks P, et al. (2012) A systematic review of the global prevalence of low back pain. Arthritis Rheum 64: 2028-2037.
- Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, et al. (2013) The state of US health, 1999-2010: Burden of diseases, injuries, and risk factors. JAMA 310: 591-608.
- Flynn TW, Smith B, Chou R (2011) Appropriate use of diagnostic imaging in low back pain: A reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther 41: 838-846.
- Iorio JA, Jakoi AM, Singla A (2016) Biomechanics of degenerative spinal disorders. Asian Spine J 10: 377-384.
- Manchikanti L, Singh V, Pampati V (2001) Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician 4: 308-316.
- DePalma MJ, Ketchum JM, Saullo T (2011) What is the source of chronic low back pain and does age play a role? Pain Med 12: 224-233.
- Cohen SP, Raja SN (2007) Pathogenesis, diagnosis, and treatment of lumbar zygapophysial (facet) joint pain. Anesthesiol 106: 591-614.
- Sizer PS Jr, Phelps V, Thompsen K (2002) Disorders of the sacroiliac joint. Pain Pract 2: 17-34.
- Hansen HC, McKenzie-Brown AM, Cohen SP, Swicegood JR, Colson JD et al. (2007) Sacroiliac joint interventions: A systematic review. Pain Physician 10: 165-184.
- Cohen SP, Chen Y, Neufeld NJ (2013) Sacroiliac joint pain: A comprehensive review of epidemiology, diagnosis and treatment. Expert Rev Neurother 13: 99-116.
- Tilburg CWJV, Stronks DL, Groeneweg JG, Huygen FJ (2017) Randomized sham-controlled, double blind, multicenter clinical trial on the effect of percutaneous radiofrequency at the ramus communicans for lumbar disc pain. Eur J Pain 21: 520-529.
- Tilburg CWJV, Stronks DL, Groeneweg JG, Huygen FJ (2016) Randomised sham-controlled double-blind multicentre clinical trial to ascertain the effect of percutaneous radiofrequency treatment for lumbar facet joint pain. Bone Joint J 98-B: 1526-1533.
- Tilburg CWJV, Schuurmans FA, Stronks DL, Groeneweg JG, Huygen FJ (2016) Randomized sham-controlled double-blind multicenter clinical trial to ascertain the effect of percutaneous radiofrequency treatment for sacroiliac joint pain: Three-month results. Clin J Pain 32: 921-926.
- Tilburg CWJV, Groeneweg JG, Stronks DL, Huygen FJPM (2017) Inter-rater reliability of diagnostic criteria for sacroiliac joint, disc and facet joint pain. J Back Musculoskelet Rehabil 30: 551-557.
- Lim HW, Cho YH, Kim SH, Lee DH, Kang SH (2013) The effectiveness of L2 nerve root block for the management of patients who are suffering from chronic low back and referred pain. Korean J Anesthesiol 65: 182-183.
- Wiesel SW, Tsourmas N, Feffer HL, Citrin CM, Patronas N (1984) A study of computer-assisted tomography. I. The incidence of positive CAT scans in an asymptomatic group of patients. Spine 9: 549-551.
- Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW (1990) Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg 72: 403-408.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, et al. (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. New Eng J Med 331: 69-73.
- Borenstein DG, O’Mara JW, Boden SD, Lauerman WC, Jacobson A, et al. (2001) The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects. J Bone Joint Surg Am 83-A: 1306-1311.
- Ohnmeiss DD, Vanhartana H, Ekholm J (1997) Degree of disc disruption and lower extremity pain. Spine 22: 1600-1605.
- Boos N, Rieder R, Schade V, Spratt KF, Semmer N, et al. (1995) 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine 20: 2613-2625.
- Vucetic N, Bri E, Svensson O (1997) Clinical history in lumbar disc herniation. A prospective study in 160 patients. Acta Orthop Scand 68: 116-120.
- Thelander U, Fagerlund M, Friberg S, Larsson S (1992) Straight leg raising test versus radiologic size, shape, and position of lumbar disc hernias. Spine 17: 395-399.
- Valls I, Saraux A, Goupille P, Khoreichi A, Baron D, et al. (2001) Factors predicting radical treatment after in-hospital conservative management of disk-related sciatica. Joint Bone Spine 68: 50-58.
- Dubourg G, Rozenberg S, Fautrel B, Valls-Bellec I, Bissery A, et al. (2002) A pilot study on the recovery from paresis after lumbar disc herniation. Spine 27: 1426-1431.
- Barzouhi A, Vleggeert-Lankamp CLAM, Kallen BFVD, Nijeholt GJL, Hout WBVD, et al. (2014) Back pain’s association with vertebral end-plate signal changes in sciatica. Spine J 14: 225-233.
- Beauvais C, Wybier M, Charzerain P, Harboun M, Liote F, et al. (2003) Prognostic value of early computed tomography in radiculopathy due to lumbar intervertebral disk herniation. A prospective study. Joint Bone Spine 70: 134-139.
- Bejia I, Younes M, Zrour S, Touzi M, Bergaoui N (2004) Factors predicting outcomes of mechanical sciatica: A review of 1092 cases. Joint Bone Spine 71: 567-571.
- Takatalo J, Karppinen J, Niinimaki J, Taimela S, Nayha S, et al. (2011) Does lumbar disc degeneration on magnetic resonance imaging associate with low back symptom severity in young Finnish adults? Spine 36: 2180-2189.
- Kovacs FM, Arana E, Royuela A, Estremera A, Amengual G, et al. (2014) Disc degeneration and chronic low back pain: An association which becomes nonsignificant when endplate changes and disc contour are taken into account. Neuroradiology 56: 25-33.
- Chou D, Samartzis D, Bellabarba C, Patel A, Luk KD, et al. (2011) Degenerative magnetic resonance imaging changes in patients with chronic low back pain: A systematic review. Spine 36: S43-53.
- Andersen JC (2011) Is immediate imaging important in managing low back pain? J Athl Train 46: 99-102.
- Chou R, Qaseem A, Snow V, Casey D, Cross JT, et al. (2007) Diagnosis and treatment of low back pain: A joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 147: 478-491.
- American college of radiology appropriateness criteria for low back pain.
- Laslett M, Williams M (1994) The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine 19: 1243-1249.
- Slipman CW, Sterenfeld EB, Chou LH, Herzog R, Vresilovic E (1998) The predictive value of provocative sacroiliac joint stress maneuvres in the diagnosis of sacroiliac joint syndrome. Arch Phys Med Rehabil 79: 288-292.
- Young S, Aprill C, Laslett M (2003) Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J 3: 460-465.
- Robinson HS, Brox JI, Robinson R, Bjelland E, Solem S, et al. (2007) The reliability of selected motion and pain provocation tests for the sacroiliac joint. Manual Therapy 12: 72-79.
- Hancock MJ, Maher CG, Latimer J, Spindler MF, McAuley JH, et al. (2007) Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain. Eur Spine J 16: 1539-1550.
- New Zealand low back pain guide. Accident rehabilitation and compensation insurance corporation of New Zealand and the National Health Committee. Wellington, 1997.
- Ostelo RWJG, Deyo RA, Stratford P, Waddell G, Croft P, et al. (2008) Interpreting change scores for pain and functional status in low back pain- Towards international consensus regarding minimal important change. Spine 33: 90-94.
- Breivik EK, Bjornsson GA, Skovlund E (2000) A comparison of pain rating scales by sampling from clinical trial data. Clin J Pain 16: 22-28.
- Grotle M, Brox JI, Vollestad NK (2004) Concurrent comparison of responsiveness in pain and functional status measurement used for patients with low back pain. Spine 29: E492-E501.
- Roer NVD, Ostelo RW, Bekkering GE, Tulder MWV, et al. (2006) Minimal clinically important change for pain intensity, funtional status, and general health status in patients with nonspecific low back pain. Spine 31: 578-582.
- Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM (2001) Clinical importance of changes in chronic pain intensity measured on a 11-point numerical pain rating scale. Pain 94: 149-158.
- Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain rating scale in patients with low back pain. Spine 30: 1331-1334.
- van Tilburg CWJV (2017) Minimally invasive treatment for lumbar spine related pain disorders. Erasmus University Rotterdam.
Citation: van Tilburg CWJ, Groeneweg JG, Stronks DL, Huygen FJPM (2018) Predictive Validity of Lumbar X-ray Images and MRIs for Chronic Low Back Pain Subtypes. J Pain Relief 7: 321. DOI: 10.4172/2167-0846.1000321
Copyright: © 2018 van Tilburg CWJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8089
- [From(publication date): 0-2018 - Nov 06, 2025]
- Breakdown by view type
- HTML page views: 7029
- PDF downloads: 1060