Research Article Open Access
Prediction of Malnutrition Using Modified Subjective Global Assessment-Dialysis Malnutrition Score in Patients on Chronic Hemodialysis
Fatin Allawi Mohammed1, Hadeel Fadhil Farhood2* and Moshtak Abdul-AtheemWtwt32Department of Community Medicine, College of Medicine, Babylon University, Iraq
3Department of Internal Medicine, College of Medicine, Babylon University, Iraq
- Corresponding Author:
- Hadeel Fadhil Farhood
Assistant Professor, Department of Community Medicine
College of Medicine, Babylon University, Iraq
Tel: 964 (1) 885 1398
E-mail: hadeelfadhil75@yahoo.com
Received Date: April 09, 2014; Accepted Date: June 05, 2014; Published Date: June 09, 2014
Citation: Mohammed FA, Farhood HF, AtheemWtwt MA (2014) Prediction of Malnutrition Using Modified Subjective Global Assessment-Dialysis Malnutrition Score in Patients on Chronic Hemodialysis. J Community Med Health Educ 4:291. doi:10.4172/2161-0711.1000291
Copyright: © 2014 Mohammed FA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community Medicine & Health Education
Abstract
Background: Malnutrition is a relatively common problem in patients on hemodialysis (HD) and is associated with increased morbidity and mortality in affected patients. Many factors may contribute to malnutrition in these patients. There is no single measurement that can reliably predict the risk for malnutrition.
Aim of study: Our aim was to determine the risk of malnutrition among hemodialysis (HD) patients in Merjan hospital / dialysis center in Iraq by using modified subjective global assessment, and to examine the relationship between various nutritional and non-nutritional factorsin those patients.
Patients and method: Cross-sectional study was undertaken in Merjan hospital dialysis center in Babylon during the period from 1st of March to 30 of June 2013. Seventy five participants diagnosed with end-stage renal failure (ESRD) were enrolled. These participants who underwent hemodialysis treatment were recruited using a convenience sampling technique. Modified Subjective global assessment (m-SGA), anthropometry, and biochemical measurements were used as evaluative tools.
Results: Nutritional status of the patients was assessed. Mean age of the study population was 51.16 ± 15.03years. Males were older than females. The mean of malnutrition score was 18.61 ± 6.17. This study shows that 32% of our patients were diabetic, while 68% of them were hypertensive; about 68% of those patients had dialysis in frequency of twice per week. Based on MS, (71%) had mild to moderate malnutrition, (23%) patients were having severe malnutrition and remaining (6%) had normal nutrition score. There was no significance of the nutritional status with age, sex, occupation or smoking habit, while there was significance with residence of patients, cause of renal failure and frequency of dialysis that our patients had regarding the laboratory investigation, nutritional status show significance only with serum albumin, and serum phosphate. 99% of our patients were anemic. The anthropometric measurements done were basal metabolic rate BMI, waist / hip ratio W/H ratio, mid arm circumference MAC. The nutritional status was significant with the mid arm circumference MAC, while there was no significance between nutritional status and basal metabolic rate BMI, and waist / hip ratio W/H ratio . 1.4
Conclusions: The frequency of malnutrition is high among patients in our dialysis center, mostly the mild to moderate malnutrition.Most of our patients on maintenance hemodialysis had nutritional problem.
Introduction
Chronic kidney disease (CKD) is currently a public health problem [1]. More than 60 million worldwide people lose their lives annually due to the risk of kidney failure [2]. CKD is a slow, progressive, and irre-versible loss of kidney function [1]. Because this loss is slow and progressive, it results in an adaptive process in which the patient remains asymptomatic for some time [3]. When the kidney fails to perform most of its function, the clinical state is labeled End-stage renal disease (ESRD), and dialysis or transplantation is required to sustain life. Hemodialysis (HD) is the most common renal treat¬ment today [4].
Malnutrition is common in haemodialysis patients and may affect as many as 40% of patients, and is associated with increased mortality and morbidity [5]. The cause of malnutrition is multifactorial and includes: inadequate food intake, hormonal and gastrointestinal disorders, dietary restric¬tions, drugs that alter nutrient absorption, insufficient dialysis, and constant presence of associated diseases. Furthermore, uremia, acidosis, and HD procedure are hyper catabolic and associated with the presence of an inflammatory state [6]. Management of the nutritional aspects of chronic kidney disease (CKD) presents a number of challenges. Most of the standard methods for assessing nutritional status can be applied to patients with renal failure; however, some of these parameters are altered by uremia. Currently, with the use of modern technology in dialysis, malnutrition is less prevalent in those patients undergoing maintenance haemodialysis. However, there is evidence suggesting that many factors that promote malnutrition in renal failure even with modern methods of haemodialysis treatment [5].
Nutritional status may be assessed by measuring anthropometric variables, using several methods. These methods include dual-energy X-ray absorptiometry, bioelectric impedance analysis, and total body protein [7]. However, these methods are expensive, cumbersome, rarely available, and impractical for routine use [8]. More recently, subjective global assessment (SGA)was used to assess nutritional status in hemodialysis patients. It was reported that the use of SGA in detecting malnutrition is simple, valid, noninvasive, and applicable [9], and its use correlates significantly with nutritional parameters [10].
Subjective Global Assessment (SGA) is a tool used by health care providersto assessnutritional status and aid in the prediction of nutrition -associated clinical outcomes, such as postoperative infections [11] and/or mortality [12]. The tool has many strengths in the clinical and research setting: it is inexpensive; is rapid to conduct ; can be used effectively by providers from different disciplines, such as nursing, dietitians, and physicians; and in some studies has been found to be reproducible, valid, and reliable [13]. Because of its strengths, SGA has been recommended by the National Kidney Foundation (NKF) Kidney Disease/Dialysis Outcomes and Quality Initiative (K/DOQI) for use in nutritional assessment in the adult dialysis population (K/DOQI 2000).
The incidence of patients with end-stage renal disease being treated by renal replacement therapy varies enormously depending on the level of affluence of the country. The highly developed countries such as North America, Europe, and Japan have the highest incident rates of treated endstage renal failure, whereas the emerging countries have very low incident rates. There are now over 1 million dialysis patients worldwide, with an incidence of about a quarter of a million new patients each year [14].
Malnutrition is considered a marker of poor progno¬sis in CKD [6]. The patients’ nutritional status is inverse¬ly associated with increased risk of hospitalization and mortality; thus constituting an important risk factor for the outcome of these patients [15]. Therefore, assessing the nutritional status of patients is essential both to prevent malnutrition and to indicate appropriate intervention in malnourished patients [16].
Patients and Methods
A cross sectional study was conducted in Hilacity, Babylon governorate, Iraq, in a Merjan Medical City (the Center for dialysis), during the period from 1st of March to 30 of June 2013.A 75 patients was collected by study application during the period from 16 of March to 30 of June 2013. The sample was convenient (any patient present at time of data collection was included in the study). The inclusion criteria for patient were:
1) age 18 years or older; 2) hemo- dialyzed for at least six months with continuing dialysis at least one time a week; 3) not hospitalizedor discharged from hemodialysis sessions ; and 4) absence of enteral or parenteral feeding. 5) Who agreed to participate in the study by verbal consent? While the Exclusion criteria for patients:
1) patients who were unable to answer the questionnaire (difficulty in understanding questions, vi¬sual or hearing impairment ,severely ill patient or uncooperative family); 2) those who refused to an¬swer the screening criteria (because they are ill or tired); 3) patients had acute renal failure); 4) those transferredfor renal failure monitoring in another city or without identification of the transfer site; 5) and those who answered less than 50% of the questionnaire (incomplete answer for all questions).
The approval of the ethics committee in the hospital was obtained.
All patients were informed about the nature of the study. They were also informed that their participation in this study is voluntary and they have the right to withdraw at any time without any penalization and their refusal to participate and withdraw will not affect their treatment at the Center. The patient read and signed the consent form. However, if the patient was illiterate, the caregiver read the consent form to participants.
A specially designed data sheet that contains:
1. Questionnaires.
2. Anthropometric measurements (post–dialysis weight, height, body mass index (BMI), Waist circumference (WC), Waist to hip ratio (WHR), Mid arm circumference (MAC)).
Biochemical investigations
Data collection took place in three steps. The first step was to interview with patients and to fill out the questionnaires, and the second steps was to perform the anthropometric measurements and the last one to take the biochemical investigations
Questionnaires: divided into three sections:
Section 1: Include socio-demographic factors: gender, age, residential location (urban or rural), employment, income, and number of people living in the same household, and smoking habit.
Section 2: Include health-related risk factors: include the number of years the patient has lived with kidney disease, the number of years on hemodialysis,number ofdialysis session per week , the presence or absence of co-morbid diseases ( DM and its duration , Hypertension and its duration, IHD, history of obstructive uropathy, SLE ,history of analgesia intake , hepatitis B and C)
Section 3: Modified subjective global assessment: The modified SGA has been indicated as a reliable and valid tool for the nutritional assessment of ‘hemodialyzed patients’. The modified SGA includes two major categories: the history and physical examination. The history portion of five sections: weight/weight change; dietary intake; gastrointestinal symptoms; functional capacity; and disease state/ co-morbidities as related to nutritional status. For weight/weight change, the patient’s weight loss from the preceding six months is recorded along with the current weight. To obtain the dietary intake of the patient, the patient was asked to recall all foods and beverages consumed during the previous 24 hours. Gastrointestinal symptoms such as nausea, vomiting, and/or diarrhea, anorexia were recorded from the patient’s self report. The gastrointestinal symptoms are considered significant if most or all symptoms have persisted for at least two weeks. Short term or intermittent symptoms are not considered significant. To assess physical functional status, patients were asked to describe their physical capabilities. The functional capacity must be related to changes associated with nutritional status (e.g. anemia, low dietary intake), and changes in the previous six months. The final feature of the history portion is co-morbid diseases related to nutritional needs (e.g. hypertension, diabetes). The second major category of the modified SGA is the physical examination. The physical examination includes an evaluation of the patient for fat and muscle wasting and edema. The area below the eye and around the triceps and bicep muscles was evaluated to determine subcutaneous fat loss. Muscle wasting was assessed by examining the temporalis muscle, prominence of the clavicles, the contour of the shoulders (rounded indicates well-nourished; squared indicates malnutrition), visibility of the scapula, interosseous muscle between the thumb and forefinger, and the gastrocnemius muscle. The area of the ankles was evaluated to determine edema. In HDP, it is critical that weight change and edema be assessed in tandem to determine if tissue wasting is masked by fluid retention. Each component has a score between one (normal) to five (very severe). After completion of physical examinations, patients were placed in one of three groups: well-nourished mild to moderate malnutrition and severe malnutrition. Thus MS has a total score between 7 and 35. Patients having MS score between (7-10) are considered as well nourished patients. MS score between 11-22 are considered as having mild to moderate malnutrition .Likewise score between 23 and 35 are considered as severely malnourished [17]. Therefore, a lower score denotes tendency towards a normal nutritional status. A higher score however is considered to be an indicator of the presence of malnutrition elements, i.e. the higher the nutritional score, the stronger the tendency towards protein calorie malnutrition.
Total nutritional scoring for each patient was assessed within 20 min. Nutritional assessment by means of the modified quantitative SGA was performed on all 75 dialysis patients. The measurements were:
1. Body mass index (BMI):
Measured according to the formula of [Weight (kg) /Height (m2)] in which the weight was measured in (kilogram) using the balanced digital scale for all subject (wearing light clothing) with an accepted error of 0.1 kg. Height was measured(in meter) using a flexible tape measures to the nearest 0.5 cm with the patient standing without shoes, heals together and the head in the horizontal plane. BMI classification is: <18.5 (Underweight), 18.5-24.9 (normal), 25-29.9 (pre-obese), and 30 or more (obese).
2. Waist circumference (WC) and waist to hip ratio (WHR)
The (WC) can be calculated to assess the central obesity, which was taken to the nearest 0.5 cm with a flexible non stretchable tape measure on the horizontal plane at the level midpoint between the lower rib margin and the iliac crest. WC ≥ 102 cm for men and ≥ 88cm for women were regarded as indicators of risk of co morbidities. The (WHR) measured by the ratio between waist circumference (WC) to hip circumference (HC) which was taken as the maximal circumference around the buttocks posteriorly and pubic symphysis anterior to the level of a greater trochanter, we depended on the criteria of NCEP/ ATPIII for the cutoff points, the ratio of (WHR) was considered as indicators of increased risk of co morbidity if >1 in male and >0.85 in female.
3. Mid-arm circumference was measured with a flexible non stretchable measure tape. The patient was asked to stand with his/her feet together, shoulders relaxed, and arms hanging freely at the sides. The non access (fistula free) arm was located to avoid the possibility of an inaccurate measurement due to fluid retention in the arm with the fistula. The midpoint on the posterior aspect of the upper arm was established between the acromial and olecranon and marked with a pencil. The measuring tape was placed around the upper arm at midpoint and pulled snugly enough to ensure contact with the arm. The measurement was recorded to the nearest centimeter.
With the patient’s permission, the patient’s file was examined to acquire the necessary biochemical data such as, s. creatinine, blood urea, s. calcium, s. albumin, s. phosphate, s. potassium, s. sodium and PCV.
A questionnaire form was prepared by researcher and supervisors, following a review of related literature and our reference about risk assessment of malnutrition in adults on maintenance hemodialysis.
Data Analysis
Recording information was checked for missing values and data entry errors. Statistical analysis was performed using Statistical Package for Social Science software (SPSS, version 17) and Microsoft office Excel 2010 was used for data processing and statistical analysis. Variables were described using frequency distribution and percentage for the patients according to their characteristics and mean (-x); standard deviation (SD) for continuous variable. The Chi square test was used for the assessment of association between the variables studied. The pvalue of less than 0.05 was significant statistically.
Results
seventy five patients had been selectedand data was collected themean age of patients (51 ± 15.03), their BMI( 25.21 ± 5.80) and modified SGA score (18.61 ± 6.17) (Table1) , 32% of patients had history of diabetes,5% had hepatitis B and 4% had hepatitis C and 68% reported history of hypertension (Table 2).There was significant difference between the mean age of male (54.34 ± 13.69) years old and female (47.32 ± 15.86) years old, t= 2.056, df=73, p= 0.043 (Table 3). Majority (69%) of study population were nonsmoker while only (5%) of them were smoker and (68%) of study population presented with frequency of dialysis twice per week, 24% once per day and 8% three per day.
| Variable | Mean ± SD |
|---|---|
| Age (years) | 51.16 ±15.03 |
| Serum creatinine (µmol/l) | 674.16 ± 290. 26 |
| Potassium | 4.81 ± 0.93 |
| PCV | 26.86 ± 4.79 |
| Body Mass Index (kg/m2) | 25.21 ± 5.80 |
| Waist to Hip Ratio (WHR) | 0.95 ± 0.09 |
| Modified SGA score | 18.61 ± 6.17 |
Table 1: Mean ± SD of study variables of study population.
| Variable | Number | % |
|---|---|---|
| Diabetes | 24 | 32 % |
| Type I | 5 | 7% |
| Type II | 19 | 25 % |
| Hypertension | 51 | 68 % |
| Ischemic heart disease | 17 | 23 % |
| Hepatitis (B and C) | 7 | 9 % |
| Hepatitis B | 4 | 5 % |
| Hepatitis C | 3 | 4 % |
| Bed ulcer | 2 | 3 % |
| Asthma | 3 | 4 % |
| Malignancy | 1 | 1 % |
| SLE | 1 | 1 % |
Table 2: Distribution of study population by medical history.
| Variable | Categories | N | Mean ± SD | t-test | df | P-value |
|---|---|---|---|---|---|---|
| Age | Male | 41 | 54.34 ± 13.69 | 2.056 | 73 | 0.043* |
| Female | 34 | 47.32 ± 15.86 |
*p value ≤ 0.01 was significant
Table 3: The mean difference of age of study population by gender.
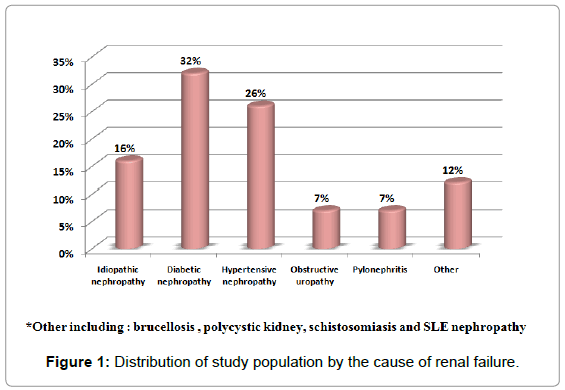
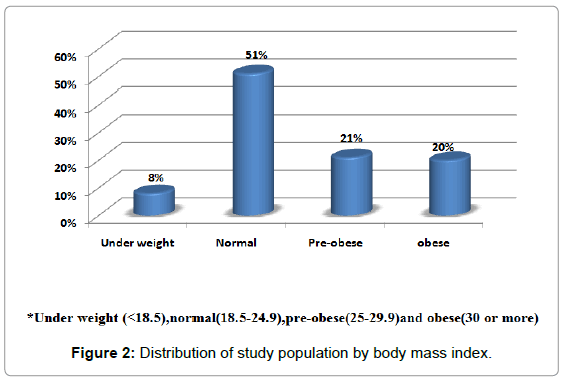
Figure 1 shows the distribution of the study population by the cause of renal failure(32%)of study population presented with diabetic nephropathy, (26%) presented with hypertensive nephropathy while only (7%) presented with obstructive uropathy and pyelonephritis as a cause of renal failure.(51%) of study population were normal BMI (18.5-24.9) while only (8%) were underweight (<18.5) (Figure 2).
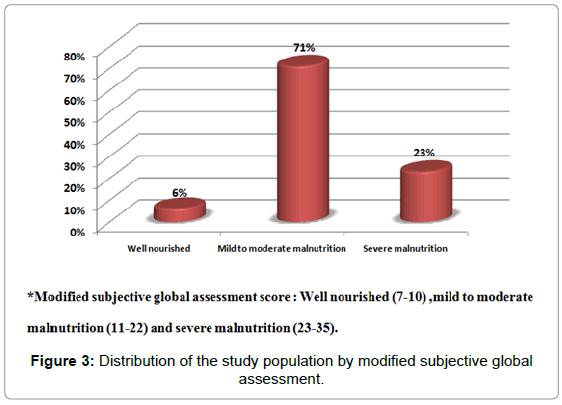
Figure 3 shows the distribution of the study population by modified subjective global assessment score to assess the nutritional status for patients with renal failure, (71%) of study population presented in mild to moderate malnutrition while only (23%) of them presented with severe malnutrition.
Table 4 shows the association of nutritional status (well nourished, mild to moderate malnutrition and severe malnutrition) by study variables including (age, sex, occupation, residence, smoking habit, cause of renal failure and dialysis frequency). There was significant association between nutritional status with cause of renal failure and dialysis frequency; meanwhile there was no significant association between nutritional status and other study variables. (59%) of those patients with severe malnutrition presented with age of (40-60) years, (53%) of them were male, (76%) of them were not employed, (65%) of them came from rural area, (23%) of them presented with diabetic nephropathy as cause of renal failure and (94%) of them presented with once per week frequency of dialysis.
| Variable | Well nourished | Mild to moderate | Severe | Total | P-value |
|---|---|---|---|---|---|
| Age | 0.817a | ||||
| < 20 years | 0 (0%) | 3 (6%) | 0 (0%) | 3 (4%) | |
| (20-40) years | 1 (20%) | 10 (19%) | 3 (18%) | 14 (19%) | |
| (40-60) years | 3 (60%) | 21 (40%) | 10 (59%) | 34 (45%) | |
| (≥60) years | 1 (20%) | 19 (35%) | 4 (23%) | 24 (32%) | |
| Sex | |||||
| Male | 3 (60%) | 29 (55%) | 9 (53%) | 41 (55%) | 1.000a |
| Female | 2 (40%) | 24 (45%) | 8 (47%) | 34 (45%) | |
| Occupation | |||||
| Employee | 2 (40%) | 12 (23%) | 4 (24%) | 18 (24%) | 0.723a |
| Not Employed | 3 (60%) | 41 (77%) | 13 (76%) | 57 (76%) | |
| Residence | |||||
| Urban | 4 (80%) | 33 (62%) | 6 (35%) | 43 (75%) | 0.089a |
| Nonurban | 1 (20%) | 20 (38%) | 11 (65%) | 32 (43%) | |
| Smoking habit (smoker & x-smoker) | |||||
| Present | 1 (20%) | 17 (32%) | 5 (29%) | 23 (31%) | 1.000a |
| Absent | 4 (80%) | 36 (68%) | 12 (71%) | 52 (69%) | |
| Cause of renal failure | |||||
| Diabeticnephopathy | 5 (100%) | 15 (28%) | 4 (23%) | 24 (32%) | 0.006**a |
| Other causes | 0 (0%) | 38 (72%) | 13 (77%) | 51 (68%) | |
| Frequency of dialysis | |||||
| Once/week | 0 (0%) | 2 (4%) | 16 (94%) | 18 (24%) | <0.001**a |
| Twice/week | 0 (0%) | 50 (94%) | 1 (6%) | 51 (68%) | |
| Thrice/week | 5 (100%) | 1 (2%) | 0 (0%) | 6 (8%) | |
Table 4: The association of nutritional status by study variables.
Table 5 shows the association of nutritional status (well nourished, mild to moderate malnutrition and severe malnutrition) by laboratory investigation including (serum creatinine, serum calcium, serum sodium, phosphate, serum potassium, serum albumin and packed cell volume). There was significant association between nutritional status with phosphate and serum albumin levels, meanwhile there was no significant association between nutritional status and other laboratory investigation (100%) of patients with severe malnutrition with high serum creatinine, (53%) of them with hypocalcaemia, (100%) of them with hyponatermia, (65%) of them with normal serum potassium level , (65%) of them with high serum phosphate level, (94%) of them with low serum albumin level and (100%) of them presented with anemia.
| Variable | Well nourished | Mild to moderate | Severe | Total | P-value |
|---|---|---|---|---|---|
| Serum creatinine | 1.000a | ||||
| High | 5 (100%) | 52 (98%) | 17 (100%) | 74 (99%) | |
| Normal | 0 (0%) | 1 (20%) | 0 (0%) | 1 (1%) | |
| Serum calcium | |||||
| Hypocalcemia | 2 (40%) | 22 (42%) | 9 (53%) | 33 (44%) | 0.791a |
| Normal | 3 (60%) | 31 (58%) | 8 (47%) | 42 (56%) | |
| Sodium | |||||
| Hypematemia | 0 (0%) | 1 (2%) | 0 (0%) | 1 (2%) | 0.769a |
| Hypenatemia | 5 (100%) | 48 (91%) | 17 (100%) | 70 (93%) | |
| Normal | 0 (0%) | 4 (7%) | 0 (0%) | 4 (5%) | |
| Potassium | |||||
| Hyperkalemia | 0 (0%) | 18 (34%) | 5 (29%) | 23 (31%) | 0.564a |
| Hypokalemia | 0 (0%) | 2 (4%) | 1 (6%) | 3 (4%) | |
| Normal | 5 (100%) | 33 (62%) | 11 (65%) | 49 (65%) | |
| Phosphate | |||||
| High | 3 (60%) | 14 (26%) | 11 (65%) | 28 (37%) | 0.009**a |
| Normal | 2 (40%) | 39 (74%) | 6 (35%) | 47 (63%) | |
| Albumin | |||||
| Low | 3 (60%) | 33 (62%) | 16 (94%) | 52 (69%) | 0.023*a |
| Normal | 2 (40%) | 20 (38%) | 1 (6%) | 23 (31%) | |
| Packed Cell volume | |||||
| Anemia | 5 (100%) | 52 (98%) | 17 (100%) | 74 (99%) | 1.000a |
| Normal | 0 (0%) | 1 (2%) | 0 (0%) | 0 (0%) | |
*Normal value:S.creatinine (53-97 μmol/l), S.Potassium (3.5-5.3 μmol/l), S.Phosphate (0.8-1.6 μmol/l), and S.Albumin (35-52 g/l)
Table 5: The association of nutritional status among study population by laboratory investigation.
Table 6 shows the association of nutritional status (well nourished, mild to moderate malnutrition and severe malnutrition) by body mass index and waist to hip ratio .There was no significant association between nutritional status with body mass index and waist to hip ratio. (47%) of patients with severe malnutrition presented with normal body mass index (18.5-24.9) while only (23%) of them presented with high risk waist to hip ratio (>1 in male or >0.85 in female).
| Variable | Well nourished | Mild to moderate | Severe | Total | P-value |
|---|---|---|---|---|---|
| Body Mass Index | |||||
| Under weight (<18.5) | 0 (0%) | 3 (6%) | 3 (18%) | 6 (8%) | 0.456a |
| Normal (18.5-24.9) | 4 (80%) | 26 (49%) | 8 (47%) | 38 (51%) | |
| Pre-obese (25-29.9) | 0 (0%) | 14 (26%) | 2 (12%) | 16 (21%) | |
| Obese (30 and more) | 1 (20%) | 19 (0%) | 4 (23%) | 15 (20%) | |
| Waist hip ratio (WHR) | |||||
| High risk (> 1 in male and >085 in female) | 3 (60%) | 23 (43%) | 4 (23%) | 30 (40%) | 0.262a |
| Not high risk | 2 (40%) | 30 (57%) | 13(77%) | 45 (60%) | |
Table 6: The association of nutritional status among study population by BMI and WHR.
Table 7 shows the mean differences of mid arm circumference by nutritional status (well nourished, mild to moderate malnutrition and severe malnutrition) among patients with renal failure. There were significant differences between means ofmid arm circumference for study sub-groups (p- value=0.046).
| Variable | Categories | N | % | Mean ± SD | F | P-value |
|---|---|---|---|---|---|---|
| MAC | Well nourished | 5 | 6% | 28.6 ±3.04 | 3.205 | 0.046* |
| Mild to moderate malnutrition | 53 | 71 % | 27.3± 3.98 | |||
| Severe malnutrition | 17 | 23 % | 24.7 ±4.41 |
Table 7: The mean difference of mid arm circumference by nutritional status.
Discussion
Malnutrition is a frequent complication which affects quality of life and is associated with increased risk of mortality and morbidity in maintenance hemodialysis patients [18,19].Compounding factors for malnutrition in hemodialysis patients are numerous. Nevertheless, the nutritional status of dialysis patients is frequently ignored. Most indicators, especially biochemical markers such as serum albumin, are useful in identifying high risk patients with malnutrition. They do not necessarily correlate with changes in other parameters and can be influencedby non-nutritional factors, such asconcomitant liver disease, iron deficiency anemia and chronic inflammation [20,21].
Several methods of nutritional state evaluation are available. However; these methods are costly and time-consuming, which restricts their use to a few research centers. Detsky et al.[22] defined special methodology, named Subjective Global Assessment which was designed to circumvent many of these problems. SGA is a reproducible and useful method for assessing the nutritional status of MHD patients. It is inexpensive, can be performed rapidly, requires only brieftraining and gives a global score of protein energy nutritional status [23].
In this study the mean of age of maintenance hemodialysis patients was 51.16 ± 15.03, the average of dialysis malnutrition score (DMS) was 18.61 ± 6.17 while in study of Soodeh et al. [24]. The mean of DMS was 16.6 ± 5.19 in another study done in India by Vansantha et al. [25], the mean of DMS was 17.9 ± 2.85. Regarding the means of BMI and WHR of our patients they were 25.21 ± 5.80, 0.95 ± 0.09 respectively. The frequency of malnutrition is high among patients in our dialysis center, mostly the mild to moderate malnutrition that can be contributed to inadequate follow up, control of dietary intake and due to co-morbid conditions since (24%)of patients had Diabetes (32%) ,7% of those were type- I DM and 25% were type - II DM. Fifty one of our patients were hypertensive (68%) while only seventeen of them(23%) had ischemic heart disease ,in study performed by Al Saran K in Saudi Arabia [26], (81%) were hypertensive, (45%) were diabetic, (27%) had ischemic heart diseases. The most common causes of CKD are diabetes mellitus, hypertension, and glomerulonephritis according to United States Renal Data System, USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda, MD, 2010.. Together these cause approximately 75% of all adult cases. Certain geographic areas have a high incidence of HIV nephropathy. ESRDcan be caused by multiple factors including, diabetes mellitus hypertension, autoimmune diseases such as lupus, glomerulonephritispyelonephritis, inherited diseases such as polycystic kidney disease and congenital abnormalities [27].
Regarding the causes of chronic renal failure in our study the main causes were Diabetes nephropathy (32%) and hypertensive nephropathy (26%), while least one was that for obstructive uropathy and pyelonephritis (7%for each one) these results agree with a study in Iran done by Malkmakan et al. [28] in which the main causes of chronic renal failure were hypertension (30.5%) and Diabetes (30.1%). Another study in Iraq Al-Anbar by Awad SM [29] found that Diabetes mellitus (33%) and hypertension (22.6%) were the most common causes of chronic renal failure in Iraq, followed in order by obstructive uropathy in 17.3%, and pyelonephritis in only4.7%. These results attributed to sedentary lifestyle, lack of healthy diet (most of our diet rich in fat and carbohydrate), lack of exercise and these certainly increase the risk of obesity and its complication. 51% of patients have normal BMI, (8%) of patients were underweight (BMI<18.5 ), and (41%) of them were preobese and obese respectively .In a prospective multicenter cohort study, researchers from the Netherlands found that baseline BMI was: below 20 kg/m2 (7.5%), 20 to 25 kg/m2 (47.0%), 25 to 30 kg/m2 (34.5%), and 30 kg/m2 or higher (11.0%)( Nancy,2011). In a study done at large Saudi center for dialysis by Al Saran et al. [30], 4% of the patients were found to be underweight, 49% had average weight, 27.5% were overweight, 14% were obese, and 5.5% had morbid obesity [26]. The countries of the Gulf Cooperation Council (GCC), which consist of Saudi Arabia, the United Arab Emirates, Kuwait, Qatar, Bahrain, and Oman, we can consider Iraq share a similar background of culture and ethnicity, while their socio-demographic distributions and socioeconomic development may also similar. Although the countries of the GCC have experienced noticeable advances in delivering healthcare, the burden of non-communicable diseases is increasing rapidly [31].
Many reports have shown evidence of increasing prevalence of the most common causes of end stage renal disease (ESRD) in the GCC: the prevalence of obesity in these countries, which is associated with multi-chronic diseases, exceeds that in the developed countries because of their rapid economic growth and associated changes in lifestyle [32].
In addition to the physical limitations in functioning caused by renal failure and its co-morbidities, HD patients have various restrictions resulting from HD therapy requiring radical lifestyle changes. Therefore, HD patients tend to have both physical and psychosocial problems. In spite of that 12% of patients in our study have no physical impairment, the majority of them (48%) presented with difficult ambulation, while only 16% of them were bed or chair ridden.
Regarding the smoking habit (5%) of population of the study were smoker, the majority (69%) were non smoker and (26%) were x-smoker that may be due to co-morbid in those patients and deterulation in general health conditions of those patients in USA, Causland et al. [33] found that 17%of hemodialysis patientswere current smokers and 32% were former smokers [33]. Another study in New Zealand by Braatvedt et al. [34] show that Seventeen percent of the total cohort study population were current smokers, 45% former smokers and 38% lifetime non smokers at dialysis commencement [34].
The modified subjective global assessment score in our patients show that there is 6% of total study population were “well nourished” , 71% were classified as “mild to moderate” malnourished , and 23% were defined as “severely malnourished” , in India by Vansantha et al. [25]. Based on the modified SGA scoring method, 91% patients were mild to moderately malnourished [25], the study of Manandhar,2008, found (84.6%) had mild to moderate malnutrition, (7.7%) patients were having severe malnutrition and remaining(7.7%) had normal nutrition score Soodeh et al. [24,35] found that in a study done Iran on hemodialysis patients that (32.1%) patients were classified as well nourished, (49.1%) as mildly to mo¬derately malnourished, and the (18.8%) as severely malnourished (Soodeh et al [24]), another study in Iran by Afshar et al. [17] found that 59.3% of patients were well nourished, 35.1% had mild to moderate malnutrition , and 5.6% had severe malnu¬trition [17]. In a study of Swedish patients on hemodialysis, Qureshi et al. [36] showed that 36% were well nourished, 51% were mildly malnourished, and 13% were severely malnourished. Forty-six percent of patients on hemodialysis were found to be wellnourished, whereas 34% were moderately nourished, and 20% were poorly nourished, according to SGA, in New York, [37].
Many factors play a role in causing variations in the prevalence of malnutrition in different studies. These factors include variations between the countries that conducted those studies, sample heterogeneity, and diversity in dietary patterns, socioeconomic status, co morbidities, and medical care at hospitals from one country to another, or even within the same country. In addition, the dose and conditions of dialysis may influence the rate of developing malnutrition [38]. The experience of the caregiver who administers the SGA may also influence the classification process [39].The cause that there was high percentage of this study’s population had severe malnutrition may be due to low dose of dialysis (inadequate, non-efficient dialysis) in our center, as there is interrelation between adequacy of dialysis and malnutrition in patients on maintenance hemodialysis. All the available evidence in hemodialysis patients confirms the close association between dialysis dose and biochemical outcome. A body of evidence also highlights the existence of relationship between malnutrition and outcome among these patients. Dose of dialysis and nutrition are considered to be interrelated [40].
This study show no significance between the nutritional state with age of the patients, since socioeconomic status, co- morbidities and medical care at hospitals mostly similar to all the patients, this results agree with study of Vansantha et al. [25] which show that there is no correlation between age and malnutrition also study by Soodeh et al. [24], show no significance between malnutrition and age of the patients other study by Kalantar et al. [41], show a significance between age and malnutrition [41].
In addition there is no significance between degree of malnutrition and the gender of the patients of this study since deterioration in the nutritional status of HD patients may be caused by disturbances in protein and energy metabolism, hormonal derangement, and reduction in energy and protein intake [42] and due to co-morbid conditions, HD patients may become malnourished despite adequate dialysis and enough protein intake [43] that may no differ regarding gender , the study of Soodeh et al. [24], as well as study of Vansantha et al.[25] and Kalantar-Zadeh et al. [37]. Also show no significance of malnutrition and sex of the patients. 53% of those with severe malnutrition were male, while 47% of them were female. Only (24% ) of our patients in the study were employed , while the rest of them (76%) were non employed in a study in Saudi Arabia by Khadija et al. [44], the majority of the patients (80.3%) did not earn an income (retired, housewife, student, unemployed) [44]. In anotherstudy done in Saudi Arabia by Zaki S 22.6% of patients are employed and 1.6% is business men [45].
The significance association between residence and malnutrition. 34%HD patients with severe malnutrition, were from rural area compare to 14% lived in urban area, this may be due to low educational level of the patients with co-morbidity like those with Hypertension, or Diabetes regarding the complication of the disease and the need for good control. This results also detected the significant association between nutritional state and causes of renal failure were majority of HD patient with diabetes nephropathy had mild to moderate malnutrition. In the developing world, diabetic nephropathy that is increasing over the years constitutes more than 25% of the dialysis population. It appears to be higher in Latin America and India than in Africa. The reported contribution of diabetes ranged from 9.1% in Egypt to 29.9% in Thailand. Hypertensive nephrosclerosis accounted for 13% to 21% of reported ESRD [46]. The Co-morbid conditions frequently contribute to deceased intake and malnutrition. One example is gastroparesis, which is likely to contribute to a poor intake in those patients with renal failure who have diabetes.
This study reported significance association between malnutrition score and frequency of dialysis, the least the dialysis frequency , the more severe degree of malnutrition that is controversy with other result that mention malnutrition is an important problem in patients treated with chronic hemodialysis, with an increasing length of time on dialysis correlating with an increasing decline in nutritional parameters [47].
The significance between malnutrition and serum phosphate, and albumin level, other studies like Vasantha et al. [25] show significance between malnutrition score and s. albumin while there was no significance with s. creatinine. The research shows that serum albumin can be used as an indicator of malnutrition in severe cases. Inflammation is considered the major contributor in the decreased serum albumin of patients on hemodialysis [48]. However, Desbrow et al. [49] found a significant inverse correlation between degrees of SGA and serum albumin (r 5 -0.28, P.038). Jankovic and Dimkovic [50] demonstrated the presence of a significant reduction in total protein and serum albumin as SGA grades increased. Regarding the serum creatinine, our study show that 99% of our patients had s. creatinine more than normal, this agree with study done in Iraq Al-Najaf by Kadhum et al. [51], the results show that all the study subjects (100%) present with high level of S.creatinine above the normal level [51]. Measurements of hemoglobin revealed the presence of anemia in all study populations, including patients in mild malnutrition. Anees et al. [52] demonstrated that 41 of 51 patients on hemodialysis were anemic. In ESRD, a low level of hemoglobin may result from many causes; hence, it is unreasonable to measure hemoglobin when assessing nutritional status. Kadhum et al. [51], also show that 100% of his study population was anemic [51]. Overzealous diet restrictions can also contribute to decreased intake. The provision of a renal diet that limits protein, salt, potassium, phosphate and fluid may further limit dietary intake in a patient with existing malnutrition and poor oral intake. Dietary intervention should notbe initiated until nutritional status and dietary habits have been assessed and clear needs for dietary restrictions are established. Underlying causes for electrolyte abnormalities such as poor glucose control, use of potassium sparing diuretics causing hyperkalemia, need to be investigated before imposing dietary restrictions. Acchiardo et al. [53] have proposed that the primary cause of hypoalbuminaemia in CKD is malnutrition.
However, poor food intake does not often result in hypoalbuminaemia if CKD is not present and although food intake is markedly lower in patients with anorexia nervosa, serum albumin levels and catabolism of protein have been shown to be similar to those of control subjects. Serum albumin levels may be low even in apparently well-nourished HD patients, and they decrease in relation to the degree of malnutrition [54].
Inflammation can cause hypoalbuminaemia by suppressing albumin synthesis and by causing transfer of albumin from the vascular to the extra vascular space. The combination of inflammation and reduced protein intake will lead to a significant reduction in serum albumin concentration.
There was no significance between the malnutrition status and the BMI, 47% from those with severe malnutrition had normal BMI. Many studies show that there was a significance of malnutrition status with BMI, as in study of Kalantar et al. [41], Khadija et al. [44] in Saudi Arabia. However, Demirag et al. [55] found that there is no significance between malnutrition status and BMI. This variation may be due to in adequate dialysis in those patients, and as a result, the remained edema affects the weight measurement and BMI calculation. For this reason we cannot depend on BMI in nutritional assessment of those patients.
Regarding MAC measurement, it was significant with nutritional status , many studies show significant relationship between MAC and malnutrition such as Kadhum et al. [51] in Al-Najaf Al ashraf, study of Kalantar et al. [41] in USA [41] Manandhar et al. [35] in Nepal [35] Vasantha et al. [25], in India [25] and Soodeh et al.[24] in Iran [24]. However, Demirag et al. [55] show that there was no correlation between nutritional status and MAC.
In this study we concluded that the frequency of malnutrition is high among patients in our dialysis center, mostly the mild to moderate malnutrition .Most of our patients on maintenance hemodialysis had nutritional problem.
In order to prevent and treat malnutrition in dialysis patients it is important to assess appropriately the nutritional status and to identify patients at risk.
References
- SBN (2009)(SociedadeBrasileira de Nefrologia). Censos
- Mojahedi M, Behroozhdam A, Hekmat R (2008) [Correlation between quality of life and social care among hemeodialysis patients] Persian. Med J Tabriz Univ Med Sci 29: 49-54.
- Romão Jr. JE (2004) Doença renal crônica: definição, epidemiologia e classificação. J Bras Nefrol. 26:1-4.
- SessoRde C, Lopes AA, Thomé FS, Lugon JR, Burdmann Ede A (2010) Brazilian dialysis census, 2009. J Bras Nefrol 32: 374-378.
- Beekley MD (2007) National Kidney Foundation. Clinical practice guidelines for nutrition in chronic renal failure.
- Shah SN, Abramowitz M, Hostetter TH, Melamed ML (2009) Serum bicarbonate levels and the progression of kidney disease: a cohort study. Am J Kidney Dis 54: 270-277.
- Sarkar SR, Kuhlmann MK, Khilnani R, Zhu F, Heymsfield SB, et al. (2005) Assessment of body composition in long-term hemodialysis patients: rationale and methodology. J RenNutr 15: 152-158.
- Bollag D, Genton L, Pichard C (2000) [Assessment of nutritional status]. Ann Med Interne (Paris) 151: 575-583.
- Anees M, Ahmed AM, Rizwan SM (2004) Evaluation of nutritional status of patients on haemodialysis. J Coll Physicians Surg Pak 14: 665-669.
- Julien JP, Combe C, Lasseur C (2001) Subjective global assessment of nutrition a useful diagnostic tool for nurses? EDTNA ERCA J 27: 193-196.
- Detsky S, Mclaughlin R, Baker P(1987)What is subjective global assessment? J Parenter Enteral Nutr11:440-446.
- [No authors listed] (1996) Adequacy of dialysis and nutrition in continuous peritoneal dialysis: association with clinical outcomes. Canada-USA (CANUSA) Peritoneal Dialysis Study Group. J Am SocNephrol 7: 198-207.
- Jones CH, Wolfenden RC, Wells LM (2004) Is subjective global assessment a reliable measure of nutritional status in hemodialysis? J RenNutr 14: 26-30.
- Moeller S, Gioberge S, Brown G (2002) ESRD patients in 2001: global overview of patients, treatment modalities and development trends. Nephrol Dial Transplant 17: 2071-2076.
- Pupim LB, Cuppari L, Ikizler TA (2006) Nutrition and metabolism in kidney disease. SeminNephrol 26: 134-157.
- Segall L, Mardare NG, Ungureanu S, Busuioc M, Nistor I, et al. (2009) Nutritional status evaluation and survival in haemodialysis patients in one centre from Romania. Nephrol Dial Transplant 24: 2536-2540.
- Reza Afshar, Suzan Sanavi , AkramIzadi-Khah(2007) Assessment of Nutritional Status in Patients Undergoing Maintenance Hemodialysis: A Single-Center Study from Iran, Saudi journal of kidney diseases and transplantation,18: 397-404.
- Neumayer LA, Smout RJ, Horn HG, Horn SD (2001) Early and sufficient feeding reduces length of stay and charges in surgical patients. J Surg Res 95: 73-77.
- Heys SD, Walker LG, Smith I, Eremin O (1999)Enteral nutritional supplementation with key nutrients in patients with critical illness and cancer: A meta-analysis of randomized controlled clinical trials. Ann Surg, 229:467-77.
- Smedley F, Bowling T, James M, Stokes E, Goodger C, et al. (2004) Randomized clinical trial of the effects of preoperative and postoperative oral nutritional supplements on clinical course and cost of care. Br J Surg, 91:983-990.
- Potter J, Langhorne P, Roberts M (1998) Routine protein energy supplementation in adults: systematic review. BMJ 317: 495-501.
- Detsky AS, Baker JP, Mendelson RA, Wolman SL, Wesson DE, et al. (1984) Evaluating the accuracy of nutritional assessment techniques applied to hospitalized patients: methodology and comparisons. JPEN J Parenter Enteral Nutr 8: 153-159.
- Persson C, Sjödén PO, Glimelius B (1999) The Swedish version of the patient-generated subjective global assessment of nutritional status: gastrointestinal vs urological cancers. ClinNutr 18: 71-77.
- Soodeh Razeghi Jahromi, Saeed Hosseini, Effat Razeghi, Ali pasha Meysamie, Haleh Sadrzadeh (2010) Malnutrition predicting factors in hemodialysis patients ,Saudi journal of kidney diseases and transplantation, 21: 846-851.
- Vasantha Janardhan, P Soundararajan, N Vanitha Rani, G Kannan, P Thennarasu, et al. (2011) Prediction of Malnutrition Using Modified Subjective Global Assessment-dialysis Malnutrition Score in Patients on Hemodialysis. Indian journal of pharmaceutical sciences, 73: 38–45.
- Al Saran K, Elsayed S, Sabry A, Hamada M (2011) Obesity and metabolic syndrome in hemodialysis patients: single center experience. Saudi J Kidney Dis Transpl 22: 1193-1198.
- Kouidi EJ (2001) Central and peripheral adaptations to physical training in patients with end-stage renal disease. Sports Med 31: 651-665.
- Malekmakan L, Haghpanah S, Pakfetrat M, Malekmakan A, Khajehdehi P (2009) Causes of chronic renal failure among Iranian hemodialysis patients. Saudi J Kidney Dis Transpl 20: 501-504.
- Awad SM (2011) Chronic renal failure in Al-Anbar of Iraq. Saudi J Kidney Dis Transpl 22: 1280-1284.
- Al Saran K, Elsayed S, Molhem A, Aldrees A, Alzara H (2011) Nutritional assessment of patients on hemodialysis in a large dialysis center. Saudi J Kidney Dis Transpl 22: 675-681.
- Mandil A (2009) Commentary: Mosaic Arab world, health and development. Int J Public Health 54: 361-362.
- Ng SW, Zaghloul S, Ali HI, Harrison G, Popkin BM (2011) The prevalence and trends of overweight, obesity and nutrition-related non-communicable diseases in the Arabian Gulf States. Obes Rev 12: 1-13.
- McCausland FR, Brunelli SM, Waikar SS (2012) Association of smoking with cardiovascular and infection-related morbidity and mortality in chronic hemodialysis. Clin J Am SocNephrol 7: 1827-1835.
- Geoffrey Braatvedt, Bronwyn Rosie, Warwick Bagg, John Collins (2006) Current and former smoking increases mortality in patients on peritoneal dialysis, Journal of the New Zealand Medical Association, 119(1234).
- DN Manandhar, PK Chhetri, LR Pahari, R Tiwari and SK Chowdhary (2008) Nutritional assessment of patients under hemodialysis in Nepal Medical College Teaching Hospital. Nepal Med Coll J, 10: 164-169.
- Qureshi AR, Alvestrand A, Danielsson A, Divino-Filho JC, Gutierrez A, et al. (1998) Factors predicting malnutrition in hemodialysis patients: a cross-sectional study. Kidney Int 53: 773-782.
- Kalantar-Zadeh K, Kleiner M, Dunne E, Ahern K, Nelson M, et al. (1998) Total iron-binding capacity-estimated transferrin correlates with the nutritional subjective global assessment in hemodialysis patients. Am J Kidney Dis 31: 263-272.
- Schulman G (2004) The dose of dialysis in hemodialysis patients: impact on nutrition. Semin Dial 17: 479-488.
- Raguso CA, Maisonneuve N, Pichard C (2004) [Subjective Global Assessment (SGA): evaluation and followup of nutritional state]. Rev Med Suisse Romande 124: 607-610.
- Azar AT, Wahba K, Mohamed AS, Massoud WA (2007) Association between dialysis dose improvement and nutritional status among hemodialysis patients. Am J Nephrol 27: 113-119.
- Kalantar-Zadeh K, Kleiner M, Dunne E, Lee GH, Luft FC (1999) A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol Dial Transplant 14: 1732-1738.
- Ikizler TA, Greene JH, Wingard RL, Parker RA, Hakim RM (1995) Spontaneous dietary protein intake during progression of chronic renal failure. J Am SocNephrol 6: 1386-1391.
- Chazot C, Laurent G, Charra B, Blanc C, VoVan C, et al. (2001) Malnutrition in long-term haemodialysis survivors. Nephrol Dial Transplant 16: 61-69.
- Khadija Alharbi, Evelyn B Enrione (2012) Malnutrition is prevalent among hemodialysis patients in Jeddah, Saudi Arabia ,Saudi journal of kidney diseases and transplantation 23: 598-608.
- Zaki S. Abu-AlMakarem Nutritional Status Assessment of the Hemodialysis Patients in Riyadh Al-Kharj Hospital A Thesis Submitted in Partial Fulfillment of the Requirements for the Master's Degree in Clinical Nutrition in the Department of Community Health Sciences at the College of Applied Medical Sciences King Saud University By Rabi I, 1425 H May, 2004 G
- Barsoum RS (2002) Overview: end-stage renal disease in the developing world. Artif Organs 26: 737-746.
- Centers for Medicare and Medicaid Services, Kinney R (2006) 2005 Annual Report: ESRD Clinical Performance Measures Project. Am J Kidney Dis 48: S1-106.
- Visser R, Dekker FW, Boeschoten EW, Stevens P, Krediet RT (1999) Reliability of the 7-point subjective global assessment scale in assessing nutritional status of dialysis patients. AdvPerit Dial 15: 222-225.
- Desbrow B, Bauer J, Blum C, Kandasamy A, McDonald A, et al. (2005) Assessment of nutritional status in hemodialysis patients using patient-generated subjective global assessment. J RenNutr 15: 211-216.
- Tirmentajn-Jankovia B, Dimkovia N (2004) [Simple methods for nutritional status assessment in patients treated with repeated hemodialysis]. Med Pregl 57: 439-444.
- Ibrahem A, Kadhum N (2012) Nutritional status of adult hemodialysis patients in Al-Najaf Al-Ashraf Governorate.Iraqi National Journal Of Nursing Specialties, 25.
- Anees M, Ahmed AM, Rizwan SM (2004) Evaluation of nutritional status of patients on haemodialysis. J Coll Physicians Surg Pak 14: 665-669.
- Acchiardo SR, Moore LW, Latour PA (1983) Malnutrition as the main factor in morbidity and mortality of hemodialysis patients. Kidney IntSuppl 16: S199-203.
- Qureshi AR, Alvestrand A, Danielsson A, Divino-Filho JC, Gutierrez A, et al. (1998) Factors predicting malnutrition in hemodialysis patients: a cross-sectional study. Kidney Int 53: 773-782.
- Demirağ A, Kalayci M, Kantarci G, Gökçe O (2009) Modified quantitative subjective global assessment of nutrition in patients on the renal transplant waiting list. Transplant Proc 41: 108-111.
Relevant Topics
- Addiction
- Adolescence
- Children Care
- Communicable Diseases
- Community Occupational Medicine
- Disorders and Treatments
- Education
- Infections
- Mental Health Education
- Mortality Rate
- Nutrition Education
- Occupational Therapy Education
- Population Health
- Prevalence
- Sexual Violence
- Social & Preventive Medicine
- Women's Healthcare
Recommended Journals
Article Tools
Article Usage
- Total views: 16664
- [From(publication date):
June-2014 - Apr 07, 2025] - Breakdown by view type
- HTML page views : 11913
- PDF downloads : 4751