Research Article Open Access
Postural Stability after Hippotherapy in an Adolescent with Cerebral Palsy
Monika Zadnikar1* and Darja Rugelj21Centre for Education and Rehabilitation for Children and Adolescents with Special Needs, Kamnik, Slovenia
2University of Ljubljana, Health Faculty of Ljubljana, Slovenia
- *Corresponding Author:
- Monika Zadnikar
Centre for Education and Rehabilitation for Children
and Adolescents with Special Needs (CIRIUS), Kamnik, Slovenia
E-mail: monika.zadnikar@guest.arnes.si
Received date : October 31, 2011; Accepted date : December 22, 2011; Published date : December 23, 2011
Citation: Zadnikar M, Rugelj D (2011) Postural Stability after Hippotherapy in an Adolescent with Cerebral Palsy. J Nov Physiother 1:106. doi: 10.4172/2165-7025.1000106
Copyright: © 2011 Zadnikar M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Objectives:To investigate whether hippotherapy has short- and long-term effects on postural control in an adolescent with cerebral palsy (CP).
Design: Pre-and post-treatment follow-up with 5-week intervention. Quantitative stabilometry and a modified sensory organization test were performed to determine the subject’s response after hippotherapy (HT). The total path length and the lengths of the mediolateral and anteroposterior centre of pressure (COP) movements were calculated.
Settings: Measurement system from the Health Faculty research laboratory in centre for HT.
Participant: Adolescent with CP.
Intervention: 5 weeks’ hippotherapy, 3 times per week for 30 minutes.
Measures: Modified sensory organization test, stabilometry and gross motor function measure.
Results: The results of measurement of the short-term effect of HT on the parameters of movement of the COP on a firm surface with eyes open show that the total path length decreased by 20.94%, the path length in the mediolateral direction decreased by 24.30%, and in the anteroposterior direction by 17.91%; the area of the stabilogram decreased by 55.54% and the individual variance index (IVI) decreased by 9.95%. After completion of HT, the total path length decreased by 33.70%, the path length in the mediolateral direction decreased by 30.48%, in the anteroposterial direction by 35.06%; the stabilogram area decreased by 59.82% and IVI decreased by 15.10%.
Conclusion: In our case study the modified sensory organization test on the force plate was sufficiently sensitive to detect fluctuation changes in the COP; therefore it is appropriate for continued use. Similarly, HT was found to have a positive effect on postural control.
Keywords
Cerebral Palsy; Diplegic; Postural Control; Hippotherapy; Stabilometry
Abbreviations
CP: Cerebral Palsy; HT: HippoTherapy
Introduction
CP
The term “cerebral palsy” is used when the cerebral insult has occurred before birth, around the time of birth or up to the age of about 3 years, while the brain is still undergoing rapid development [1,2]. Disorders of movement and posture are caused by damage to the motor cortex. In addition to postural and motor abnormalities, which are always present, people with CP may exhibit learning disabilities, other cognitive and sensory impairments, hearing and visual loss, speech and language disorders, emotional problems, orthopaedic complications and epilepsy [3-6]. The consequences of chronic muscle imbalance and the resultant deformities can cause increasing disability with age [7,8]. One of the most significant problems in children with CP is defective postural control.
Posture
Posture involves orientation of the body in space so that muscles work efficiently against gravity. Postural control is dependent on proper functioning of righting, equilibrium and protective reactions, which are controlled by the central nervous system [9,10]. A certain degree of postural control is essential for controlled and coordinated movement of the extremities, head and trunk control, functional trunk mobility, maintaining symmetry, displaying the ability to weight shift and bear weight in all directions, and coordinated and voluntary limb movements [11-13]. Individuals with central nervous system damage may show signs of disrupted postural mechanisms [10,13] “Postural control is organized at two functional levels. The first level consists of a direction-specific adjustment when the equilibrium of the body is endangered, or the generation of direction-specific patterns of postural adjustment, while the second level fine-tunes the basic, direction-specific adjustment with input from the somatosensory, visual, and vestibular systems” [9]. Hippotherapy, in which equine movement is used for its therapeutic effect, is one of the approaches for improving postural control [15].
Hippotherapy (HT)
HT is defined as the therapeutic use of a horse as part of an integrated treatment strategy for children and adults with movement dysfunction [16-18]. The primary goal of HT is to improve the individual’s balance, posture, function, and mobility. The horse’s gait provides a precise, smooth, rhythmic, and repetitive threedimensional pattern of movement to the rider [19-23]. In general, the movement of the horse provides a variety of inputs to the rider, which may be used to facilitate improved contraction, weight shift, and postural equilibrium and balance responses, and improve strength, coordination, muscle tone, joint range of movements, weight bearing, gait, and sensory processing [19,24-26].
Stabilometry
Stabilometry is one of the most commonly used methods for measuring the parameters of postural steadiness. It determines the movement of the body’s COP within the support base during upright stance [27].
The dual purpose of our study was to:
1. Verify the suitability and feasibility of the modified test of sensory organization
2. Establish the short and long-term effects of HT in a person with cerebral palsy on the stability of posture, which are inferred from parameters of movement of the centre of pressure.
Methods
Participants - subjects
The University of Ljubljana, Faculty of Health Studies and the Centre for Education and Rehabilitation for Children and Adolescents with Special Needs approved the pilot study. Inclusion criteria for the subject included: (1) adult; (2) CP; (3) no previous hippotherapy. The participant signed a consent form approved by the Centre for Education and Rehabilitation for Children and Adolescents with Special Needs. No attempt was made to limit participation in other activities. The participant continued to receive physiotherapy and occupational therapy.
The subject of the case study was an 18-year-old male with a diagnosis of cerebral palsy and epilepsy. The subject suffered from spastic diplegia, with greater impairment on the left side. The asymmetry of muscle tone and increased muscle tone on the left side of the body resulted in mild asymmetry of the ribcage, an asymmetrical position of the pelvis and adduction and internal rotation of the left lower limb with knee flexion and inversion of the left foot. Asymmetry of muscle tone causes asymmetry of the whole body and perception of the body in space, which is reflected in the change in control of body posture in the standing position, with the asymmetry being even more pronounced when walking. The degree of functional motor ability, expressed by the GMFM test (Gross motor function measure), was 79% before hippotherapy.
Procedures and design
Intervention: The adult participated in a 30 – minute hippotherapy intervention 3 times a week for 5 weeks HT intervention. HT was individualized according to the adult’s needs and administered by one physiotherapist with support from riding instructors. During a 30-minute session the therapist encouraged a symmetrical body position, additional pelvic movement, especially to the left and right, and stimulated lateral trunk flexion and rotation between the pelvis and the shoulder girdle.
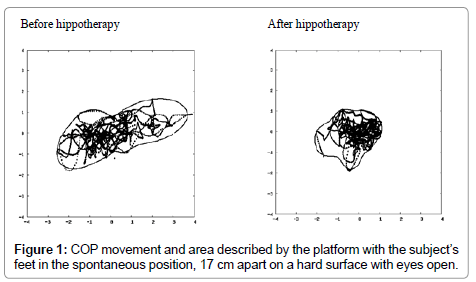
Measurements on the force platform, on which movement of the COP was measured, were performed before the commencement of HT, immediately after the first HT session and after the five-week period. Besides stabilometry, a modified sensory organization test [12], which comprised six measurements in quiet standing on the force platform, was performed before hippotherapy. Immediately following HT the same six measurements were repeated. The first two movements comprised standing on a firm base with the feet 17cm apart, with eyes open and closed. For the next two measurements the subject had his feet together with eyes open and closed. In the third two measurements the subject stood on a soft base with his feet 17 cm apart with eyes open and closed (Figure 1). The demand for postural control was increased by standing with feet together, thus decreasing the support base, and by closing his eyes.
Data analysis: Stabilometry was used to assess the amount of postural sway. Data were collected at a 50 Hz sampling rate for 60 seconds using a portable force platform (Kistler 9286 AA, Wintherthur, Switzerland). The raw data were stored on the disk of a PC-type computer using Kistler’s BioWare programme. For the analysis they were later uploaded to a server running under the Linux (Fedora 12) operating system. Data analysis was performed using webbased software that had been specially developed for our stabilometric measurements [27].
Analysis of the stabilometric data was begun by smoothing the acquired COP positions in the mediolateral and anteroposterior directions using moving averages over 10 adjacent points. From the resulting data standard statistical parameters of standard deviation and the averages of the absolute values of COP displacements and velocities, total path length and the lengths of the mediolateral and anteroposterior COP movements and the frequency distributions of the positions and velocities were calculated. Finally, we determined the outline of the measured data and calculated its Fourier coefficients, area and other related parameters.
Results
The 18-year-old adolescent, despite impaired movement due to CP, was able to stand on the force platform for 60 seconds with feet together or apart with eyes open and closed. On the soft base, before the first hippotherapy session, he stood with feet apart and eyes open for 60 seconds and in the same position with eyes closed for only 25 seconds, while after 5 weeks’ therapy he also stood for 60 seconds under the same conditions (Table 1).
| Path (cm) | M-L path (cm) | A-P path (cm) | Area (cm2) | IVI | |
|---|---|---|---|---|---|
| Before the first HT | |||||
| Spontaneous position | |||||
| FB EO | 121.27 | 70.56 | 83.74 | 14.26 | 2.11 |
| FB EC | 120.89 | 56.46 | 95.75 | 7.29 | 1.93 |
| SB EO | 153.13 | 85.29 | 109.45 | 18.92 | 2.05 |
| SB EC | / | / | / | / | / |
| Feet together | |||||
| FB EO | 132.23 | 75.51 | 91.63 | 14.39 | 1.83 |
| FB EC | 182.23 | 94.16 | 136.91 | 18.47 | 2.01 |
| After the first HT | |||||
| Spontaneous position | |||||
| FB EO | 95.87 | 53.41 | 68.74 | 6.34 | 1.90 |
| TP EZ | 117.27 | 73.86 | 75.84 | 15.84 | 1.76 |
| SB EO | 134.29 | 76.64 | 94.22 | 14.61 | 1.61 |
| SB EC | / | / | / | / | / |
| Feet together | |||||
| FB EO | 114.66 | 63.05 | 82.92 | 12.50 | 2.09 |
| FB EC | 166.04 | 109.82 | 102.51 | 19.36 | 1.83 |
| Before the last HT | |||||
| Spontaneous position | |||||
| FB EO | 82.27 | 41.59 | 63.23 | 11.97 | 2.57 |
| FB EC | 101.14 | 45.51 | 81.14 | 8.42 | 2.24 |
| SB EO | 150.48 | 89.00 | 102.59 | 16.43 | 2.10 |
| SB EC | 169.91 | 101.30 | 114.47 | 16.52 | 1.74 |
| Feet together | |||||
| FB EO | 103.97 | 63.05 | 70.03 | 8.36 | 1.75 |
| FB OC | 123.79 | 73.08 | 84.13 | 10.52 | 1.83 |
| After the last HT | |||||
| Spontaneous position | |||||
| FB EO | 80.40 | 49.05 | 54.38 | 5.73 | 1.79 |
| FB EC | 89.65 | 51.91 | 63.00 | 6.19 | 2.26 |
| SB EO | 112.49 | 69.45 | 74.64 | 11.04 | 1.88 |
| SB EC | 179.04 | 123.34 | 103.66 | 57.04 | 2.67 |
| Feet together | |||||
| FB EO | 93.96 | 61.06 | 58.80 | 10.88 | 1.85 |
| FB EC | 127.29 | 83.95 | 78.19 | 11.24 | 1.75 |
Table 1: Results of the modified sensory organization test before HT and after 5 weeks’ HT; data on the paths, areaandIVI. Data are classified according to when hippotherapy was performed.
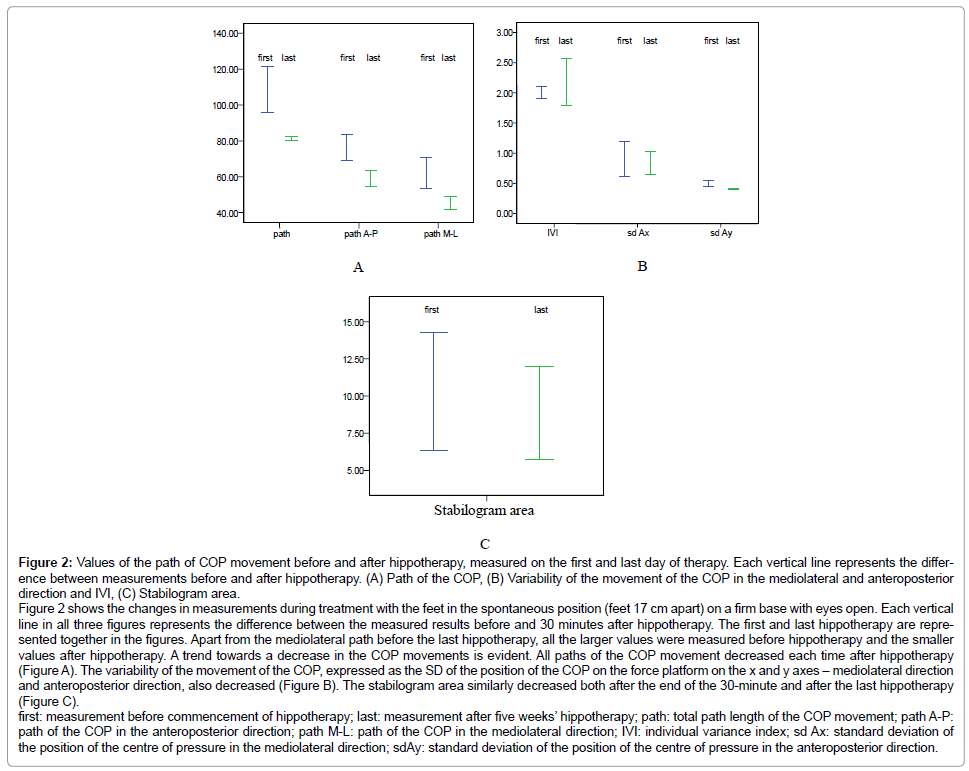
The results of measurements with the force platform were analysed on two levels. Initially, we observed the short-term effect of a 30-minute hippotherapy session on the parameters of movement of the COP on a firm base and eyes open: the total path length decreased by 20.94%, the path length in the mediolateral direction decreased by 24.30% and in the anteroposterior direction by 17.91%; the stabilogram area decreased by 55.54% and IVI decreased by 9.95% (Figure 2). Later, we compared the results before hippotherapy and after five weeks’ therapy, which revealed that the total path length decreased by 33.70%, the path length in the mediolateral direction decreased by 30.48%, in the anteroposterior direction by 35.06%; the stabilogram area decreased by 59.82% and IVI decreased by 15.10%. All the results for the total path length of the COP, path length in the mediolateral and anteroposterior directions, stabilogram area and IVI of the subject are presented in table 1. The pretest GMFM score was 79% compared to 86% at the conclusion of the test period after five weeks’ hippotherapy. The 7% improvement was found only in parts D (standing) and E (walking, running and jumping).
Figure 2: Values of the path of COP movement before and after hippotherapy, measured on the first and last day of therapy. Each vertical line represents the difference between measurements before and after hippotherapy. (A) Path of the COP, (B) Variability of the movement of the COP in the mediolateral and anteroposterior direction and IVI, (C) Stabilogram area. Figure 2 shows the changes in measurements during treatment with the feet in the spontaneous position (feet 17 cm apart) on a firm base with eyes open. Each vertical line in all three figures represents the difference between the measured results before and 30 minutes after hippotherapy. The first and last hippotherapy are represented together in the figures. Apart from the mediolateral path before the last hippotherapy, all the larger values were measured before hippotherapy and the smaller values after hippotherapy. A trend towards a decrease in the COP movements is evident. All paths of the COP movement decreased each time after hippotherapy (Figure A). The variability of the movement of the COP, expressed as the SD of the position of the COP on the force platform on the x and y axes – mediolateral direction and anteroposterior direction, also decreased (Figure B). The stabilogram area similarly decreased both after the end of the 30-minute and after the last hippotherapy (Figure C). first: measurement before commencement of hippotherapy; last: measurement after five weeks’ hippotherapy; path: total path length of the COP movement; path A-P: path of the COP in the anteroposterior direction; path M-L: path of the COP in the mediolateral direction; IVI: individual variance index; sd Ax: standard deviation of the position of the centre of pressure in the mediolateral direction; sdAy: standard deviation of the position of the centre of pressure in the anteroposterior direction.
Discussion
The presented case study provided information on the suitability of the proposed measurement protocol for the assessment of the effects of hippotherapy on the stability of posture or improvement in balance in people with sensorimotor disturbances. We established that it is possible to carry out the proposed modified sensory organization test in its entirety before and after hippotherapy in a person with the spastic form of CP. The subject was able to maintain the position for the 60 seconds required to obtain the data under all measurement conditions, in the spontaneous feet position, with feet together, with eyes open and closed and on a soft base. Sixty seconds represents the period for obtaining data that provides greater reliability and reproducibility of obtained stabilometric data [28]. We found that the parameters of COP movement after hippotherapy decreased when the subject had his eyes open, as did parameters for the total path length of the COP and individual components, that is anteroposterior and mediolateral components of the path length and the area described by the COP. They increased if the subject closed his eyes, and further increased if he stood on a soft base. The increase in postural sway is characteristic of the fluctuation in sensory input and conflicting information, resulting in a significant increase in the stabilogram area [27,28]. Since the path length of the COP and average speed are correlated, the results of our study can be compared with those of Kuczynski and Slonka [29], who reported a decrease in average speed and extent of sway in the anteroposterior and mediolateral direction and their standard deviations, which means decreased variability between attempts or a smaller number of larger excursions towards the edge of the force platform. Similarly, speed of movement decreased. There was no change in movement frequency in children with CP after 3 months’ therapy that consisted of riding on the Brunel active balance saddle twice weekly for 20 minutes. The difference between people with CP and a comparable group of healthy children was statistically significant in this study.
Knowledge of equine-assisted therapies, especially hippotherapy, and their efficacy is continually increasing and becoming more reliable and precise [30]. Most studies focus on researching the effects on the Gross Motor Function Measure (GMFM), muscle tone, temperospatial parameters of walking and energy use during walking. One of the rare studies to use stabilometry as a measurement tool is the above-mentioned study of Kuczynski et al. [29]. In addition, in metaanalyses with systematic reviews a detailed analysis of studies that influence the effect of HT on postural control and balance has been performed [31]. These results show that hippotherapy, which transmit stimuli across the pelvis and thus elicit the righting and equilibrium reactions are effective improving postural control in people with CP.
Conclusion
With this case study we verified the feasibility and suitability of the modified test of sensory organization and stabilometry and the short-term effects before and after hippotherapy in a person with CP. We established that the modified sensory organization test on the force platform is sufficiently sensitive to detect changes in oscillation of the COP on the force platform. A longitudinal study is planned to analyse the long-term effects of hippotherapy. This will enable us to answer the question as to how hippotherapy influences postural control in a larger sample of adolescents with CP. Analysis of obtained data showed that the protocol is suitable for obtaining answers to the hypothesis posed prior to the case study.
Acknowledgements
We thank Dianne Jones for language review and the physiotherapists at CIRIUS Kamnik for assistance with hippotherapy intervention. The second author was supported by the Slovenian Research Agency.Rehabilitation Research Center of Tehran University of Medical Sciences for providing the place and necessary equipments for data collection.
References
- E Bower (2009) Finnie's Handling the young child with cerebral palsy at home. Butterworth Heinemann Elsevier 15-27.
- Koman LA, Smith BP, Shilt JS (2004) Cerebral palsy. Lancet 363: 1619-1631.
- Best SJ (2005) Cerebral Palsy. Teaching individuals with physical or multiple disabilities. 5th edn. Upper Saddle River: Prentice Hall.
- Miller F (2007) Physical therapy of cerebral palsy. New York: Springer: 416.
- Taylor JR, Kopriva PG (2002) Cerebral palsy. In: Brodwin MG, Tellez FA, Brodwin SK, editors. Medical, psychosocial, and vocational aspects of disability. Athens: Elliott Fitzpatrick 387-400.
- Meregillano G (2004) Hippotherapy. Phys Med RehabilClin N Am 15: 843-854.
- Benda W, McGibbon NH, Grant KL (2003) Improvements in muscle symmetry in children with cerebral palsy after equine-assisted therapy (hippotherapy). J Altern Complement Med 9: 817-825.
- Massion J, Alexandrov A, FrolovA (2004) Why and how are posture and movement coordinated? Prog Brain Res 143: 13-27.
- van der Heide JC, Hadders-Algra M (2005) Postural muscle dyscoordination in children with cerebral palsy. Neural Plast 12: 197-203.
- Land G, Errington-Povalac E, Paul S (2002) The effects of therapeutic riding on sitting posture in individuals with disabilities. OccupTher Health Care 14: 1-12.
- van der Heide JC, Begeer C, Fock JM, Otten B, Stremmelaar E, et al. (2004) Postural control during reaching in preterm children with cerebral palsy. Dev Med Child Neurol 46: 253-266.
- Shumway-Cook A, Horak FB (1986) Assessing the influence of sensory interaction of balance. Suggestion from the field. PhysTher 66: 1548-1550.
- Shumway-Cook A, Horak FB (1986) Assessing the influence of sensory interaction on balance. PhysTher 66:1538-1550.
- Forssberg H, Hirschfeld H (1994) Postural adjustments in sitting humans following external perturbations: muscle activity and kinematics. Exp Brain Res 97: 515-527.
- McGibbon NH, Benda W, Duncan BR, Silkwood-Sherer D (2009) Immediate and long-term effects of hippotherapy on symmetry of adductor muscle activity and functional ability in children with spastic cerebral palsy. Arch Phys Med Rehabil 90: 966-974.
- McGibbon NH, Andrade CK, Widener G, Cintas HL (1998) Effect of an equinemovement therapy program on gait, energy expenditure, and motor function in children with spastic cerebral palsy: a pilot study. Dev Med Child Neurol 40: 754-762.
- Hamill D, Washington KA, White OR (2007) The effect of hippotherapy on postural control in sitting for children with cerebral palsy. PhysOccupTherPediatr 27: 23-42.
- Cherng RJ, Liao HF, Leung HWC, Hwang AW (2004). The effectiveness of therapeutic horseback riding in children with spastic cerebral palsy. APAQ21: 103-121.
- Bertoti DB (1988) Effect of therapeutic horseback riding on posture in children with cerebral palsy. PhysTher 68: 1505-1512.
- Shurtleff TL, Standeven JW, Engsberg JR (2009) Changes in dynamic trunk/ head stability and functional reach after hippotherapy. Arch Phys Med Rehabil 90: 1185-1195.
- MacPhail A, Edwards J, Golding J, Miller K, Moiser C, Zwiers T (1998) Trunk postural reactions in children with and without cerebral palsy during therapeutic horseback riding. Pediatr Phys Ther 10: 143-147.
- McGee MC, Reese NB (2009) Immediate effects of a hippotherapy session on gait parameters in children with spastic cerebral palsy. Pediatr Phys Ther 21: 212-218.
- Winchester P, Kendall K, Peters H, Sears N, Winkley T (2002) The effect of therapeutic horseback riding on gross motor function and gait speed in children who are developmentally delayed. Phys OccupTher Pediatr 22: 37-50.
- Freeman G (1984) Hippotherapy: therapeutic horseback riding. ClinManag PhysTher 4: 20-25.
- Murphy D, Kahn-D'Angelo L, Gleason J (2008) The effect of hippotherapy on functional outcomes for children with disabilities: a pilot study. Pediatr Phys Ther 20: 264-270.
- Haehl V, Giuliani C, Lewis C (1999) Influence of hippotherapy on the kinematics and functional performance of two children with cerebral palsy. PediatrPhysTher 11: 89-101.
- Rugelj D, Sevsek F (2011) The effect of load mass and its placement on postural sway. ApplErgon 42: 860-866.
- Doyle RJ, Ragan BG, Rajendran K, Rosengren KS, Hsiao-Wecksler ET (2008) Generalizability of Stabilogram Diffusion Analysis of center of pressure measures. Gait Posture 27: 223-230.
- Kuczynski M, Slonka K (1999) Influence of artificial saddle riding on postural stability in children with cerebral palsy. Gait Posture 10: 154-160.
- Sterba JA (2007) Does horseback riding therapy or therapist-directed hippotherapy rehabilitate children with cerebral palsy? Dev Med Child Neurol 49: 68-73.
- Zadnikar M, Kastrin A (2011) Effects of hippotherapy and therapeutic horseback riding on postural control or balance in children with cerebral palsy: a metaanalysis. Dev Med Child Neurol 53: 684-691.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 8018
- [From(publication date):
December-2011 - Apr 02, 2025] - Breakdown by view type
- HTML page views : 3312
- PDF downloads : 4706