Post-partum Lymphocytic Hypophysitis in Ethiopian Woman's
Received: 24-Oct-2020 / Manuscript No. jomb-22-21160 / Editor assigned: 26-Oct-2020 / PreQC No. jomb-22-21160 (PQ) / Reviewed: 11-Feb-2022 / QC No. jomb-22-21160 / Revised: 16-Feb-2022 / Manuscript No. jomb-22-21160 (R) / Accepted Date: 22-Feb-2022 / Published Date: 23-Feb-2022 DOI: 10.4172/jomb.1000110
Abstract
A 28 year-old young woman who was referred from Bahir Dar, Ethiopia for possible neurosurgical evaluation and management after she presented with headache and failure to lactate one month following delivery. The initial hormonal analysis was consistent with hypopituitarism. The magnetic resonance imaging (MRI) of the Brain done initially showed diffuse enlargement of the pituitary gland and thickening of the pituitary stalk. Most of the pituitary axes recovered after one month of hormonal replacement therapy. The follow-up MRI done after four weeks showed resolution of pituitary gland enlargement and stalk thickening. Based on clinical presentation, pituitary hormonal insufficiency and Brain MRI findings, the diagnosis of lymphocytic hypophysitis was made. Lymphocytic hypophysitis is a rare disease in which inflammation of the pituitary gland and stalk occurs. It is associated with transient or permanent insufficiency pituitary hormones. It usually occurs in women during third trimester of pregnancy or postpartum period. Systemic corticosteroid treatment at early stage may avoid unnecessary surgery in some cases but there are reported cases of spontaneous resolution.
Keywords
Hypopituitarism; Lymphocytic hypophysitis; Pregnancy; Postpartum period
Introduction
Lymphocytic hypophysitis is a rare disease characterized by inflammation of the pituitary gland and stalk. It is generally seen in women during third trimester of pregnancy or postpartum period [1]. The estimated incidence of Lymphocytic hypophysitis is one case per 9 million people [2]. The incidence reported might be underestimated because of the recent recognition of IgG4 related disease and immune check point inhibitor related disease [3]. It is often associated with other autoimmune disease conditions like autoimmune thyroiditis, Addison’s disease and Systemic lupus erythematosus. The histological characteristics show lymphocytic infiltration accompanied by edema and fibrosis with different levels of severity that may lead to transient or permanent hormonal dysfunction [4].
Patients with hypophysitis present with symptoms related to mass effect from pituitary gland enlargement and dysfunction. The area the pituitary gland affected and the size of its enlargement determine the various clinical manifestations. The treatment of Lymphocytic hypophysitis has not been examined well in prospective controlled studies. Medical management using immunosuppressive drugs can induce remission of autoimmune hypophysitis by treating both pituitary dysfunction and compression symptoms [5]. For those with mass effect like Visual loss, intractable headache and lack of response to medical therapy may require decompressive transsphenoidal surgery. In a number of published case reports of lymphocytic hypophysitis pituitary enlargement that resolved spontaneously has been described. In one group of study done recently showed radiologic finding regression in 15/15 patients receiving supportive therapy [6]. Here we describe a patient in the postpartum period with markedly enlarged pituitary gland due to lymphocytic hypophysitis and associated hypopituitarism on replacement dose of corticosteroid with follow up clinical and radiologic improvement.
Case Report
A 28 year-old young woman who was referred from Bahir Dar, Ethiopia for possible neurosurgical evaluation and management after she presented with headache and failure to lactate one month following delivery. The headache was severe global in type with difficulty opening her eyes. It was unresponsive to analgesics and stayed for six consecutive days with subsequent resolution. She gave birth at term through caesarian section the indication being failed induction and the outcome was an alive male neonate weighing 3.6kg. There was no history suggestive of obstetric haemorrhage. She has no visual impairment and started seeing her menstruation regularly following delivery.
The patient’s vital signs were stable with blood pressure in the normal range with no postural hypotension, BP=110/72-120/80 mmHg and pulse rate normal ranging from 74-80/min, and the rest of the physical examination had no significant findings (Table 1). Laboratory findings showed Fasting blood glucose in normal range, [FBS=87 mg/ dL [74 – 110]], Serum electrolytes within normal range [sodium= 143 mmol/L [136 – 146], potassium= 4.3mmol/L [3.4 - 4.5]].
Serum creatinine was normal with [0.56 mg/dL [0.51 - 0.95]] and complete blood count within normal limit with hemoglobin of [12.3 g/dl [11.8 - 14.7]], leucocytes [6000/micro liter [4100 – 9900]] and platelets [233,000/micro liter [150,000-450,000]] and liver function test was also normal. VDRL, HBSAg, HCV Ab and HIV all were negative. The initial hormonal study done was compatible with hypopituitarism [thyrotropin = 0.09 mU/L [0.55 - 4.78], free thyroxine = 0.68 ng/dL [0.80 - 1.76], Free T3 = 3.18 pmol/l [3.5-6.5], Cortisol <2.9ng/dl [4.22 - 22.4], LH= 1.89 U/L [1.9 - 12.5], FSH = 2.62 U/L [3.9-12]; estradiol, within normal limit =353.73 pg/mL [93-575] and prolactin; in the lower half of the reference range = 8.74 ng/mL [2.8 - 29.2]]. Chest X-ray showed normal findings.
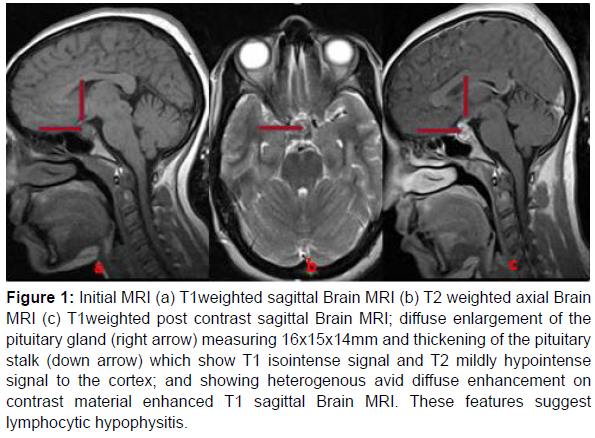
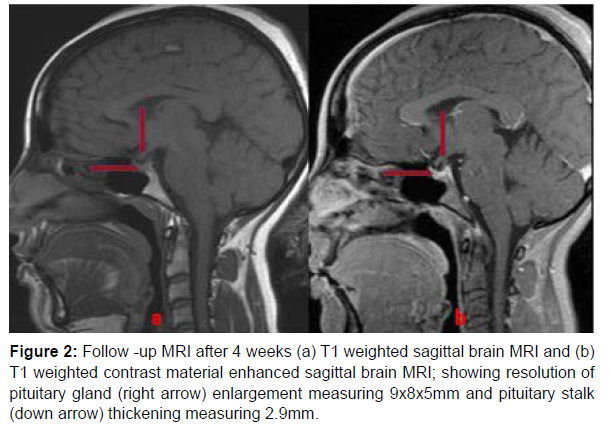
Initial Brain MRI showed diffuse enlargement of the pituitary gland measuring 16x15x14mm and thickening of the pituitary stalk measuring 5.7mm which suggests lymphocytic hypophysitis (Figure 1). Patient was initiated on hormone replacement therapy with Prednisolone 7.5mg PO daily for secondary adrenal insufficiency, and followed by Levothyroxine 25 mcg PO per day for central hypothyroidism. After four weeks of follow up treatment, she showed marked clinical improvement with no headache and started to breast feed her infant. She has also improvement in hormonal axes (Table 2). Control Brain MRI showed resolution of pituitary gland enlargement measuring 9x8x5mm and pituitary stalk thickening measuring 2.9mm (Figure 2). Progressively her prednisolone was reduced to 5mg PO daily and levothyroxine discontinued after normalization of the free thyroxine level (Table 1 and Figure 1).
| Gender | Female |
|---|---|
| Age | 28 |
| Blood Pressure [in mmHg] Pulse rate[beats/min] Thyroid examination Lymph nodes Chest examination Cardiovascular examination |
110/72-120/80 74-80 Normal Normal Normal Normal |
| Neurologic examination | |
| Consciousness | Alert |
| Visual acuity | 6/6 |
| Visual field | Normal |
| Fundus ophthalmoscopy | Normal |
| Cranial nerve examination | Normal |
| Sensory examination | Normal |
| Motor examination | Normal |
Table 1: Physical examination.
Figure 1: Initial MRI (a) T1weighted sagittal Brain MRI (b) T2 weighted axial Brain MRI (c) T1weighted post contrast sagittal Brain MRI; diffuse enlargement of the pituitary gland (right arrow) measuring 16x15x14mm and thickening of the pituitary stalk (down arrow) which show T1 isointense signal and T2 mildly hypointense signal to the cortex; and showing heterogenous avid diffuse enhancement on contrast material enhanced T1 sagittal Brain MRI. These features suggest lymphocytic hypophysitis.
Discussion
Lymphocytic hypophysitis is more common in female than male in a ratio of 6:1 according to P. caturegli [7], and tend to occur at younger age in women [35±13 years] compared to men [45 ± 14years] that is consistent with our case [7]. It is found that significant percentage of cases of lymphocytic hypophysitis occur during third trimester of pregnancy and the first two months in the post-partum period [7,8] which is similar with our patient who presented one month after delivery. One of the common presenting symptoms in the “single center case series” described by Brandon S. Imber et.al, [9] was headache that was found in about 57% of cases [9] and it was the main presentation in our case. In about 80% of cases multiple hormone deficiencies are found in lymphocytic hypophysitis [10] which is a presentation in our case with cortisol, thyrotropin and gonadotropin deficiencies. Inhibition of lactation can be found in about 11% of cases [1,7].
Failed breast feeding was one of the first presentation in our patient possibly associated with relative hypoprolactinemia. Due to pituitary stalk compressive effect some cases may present with mild hyperprolactinemia which is not found in our case. Our patient’s initial presentation of severe headache with difficulty opening the eyes and unresponsiveness to analgesics made us to consider pituitary apoplexy as a possible differential diagnosis as it could present with similar signs and symptoms in the post-partum period. In our case the improved clinical and hormonal responses and the marked Brain MRI normalization to replacement dose of steroid avoided unnecessary neurosurgical management (Table 2 and Figure 2).
| Hormone | Day 1 | Day 7 | Day 23 | Normal range |
|---|---|---|---|---|
| *TSH (mU/L) | <0.09 | 0.0462 | 0.2 | 0.55 - 4.78 |
| **FreeT4 (ng/dL) | 0.69 | 1.43 | 0.80 - 1.76 | |
| Cortisol (ng/dL) | < 2.9 | 4.22 - 22.4 | ||
| ***LH (U/L) | 1.89 | 1.9 - 12.5 | ||
| ****FSH (U/L) | 2.62 | 3.9-12 | ||
| Estradiol pg/mL | 353.73 | 93-575 | ||
| *TSH: thyrotropin; **T4 free: free thyroxine; ***LH: luteinizing hormone; ****FSH: follicle stimulating hormone | ||||
Table 2: Hormonal changes after the start of corticosteroid replacement.
According to the description made by S. khare et al, [12] characteristically cortcotrophs are affected in about 75% of cases lymphocytic hypophysitis but in pituitary adenoma the last hormone to be affected is corticotroph which was the case in our patient with secondary adrenal insufficiency resulted from hypophysitis [8].
Brain MRI is the imaging procedure of choice in the diagnosis of lymphocytic hypophysitis. Currently it is not easy to distinguish specifically hypophysitis from a pituitary adenoma based on radiologic finding and about 40% of patients are misdiagnosed as having pituitary macroadenoma and undergo unnecessary surgery [5,13]. Therefore, based on the presence of clinical features and radiologic signs a scoring system by Gutenberg, A., et al [13] was proposed (Table 3). Here we applied the scoring to our patient individual items were added and a score of −12 was obtained which is suggestive of lymphocytic hypophysitis [13].
| Features | Score | |
|---|---|---|
| 1 | Age less than or equal to 30 | -1 |
| 2 | Current pregnancy or being less than or equal to 6 months postpartum | -4 |
| 3 | An increased stalk size | -5 |
| 4 | Increased gadolinium enhancement | -1 |
| 5 | Loss of pituitary “bright spot” | -2 |
| 6 | Pituitary volume greater than 6cm3 | +2 |
| 7 | Sphenoid mucosal thickening | +2 |
| 8 | Heterogeneous gadolinium enhancement | +1 |
| 9 | Asymmetrical sellar enlargement | +3 |
| Total score >1-suggestive of pituitary adenoma | ||
| Score 0 or less- suggestive of Lymphocytic Hypophysitis. | ||
Table 3: Gutenberg Scoring System.
Lupi et al. [5] reviewed a total of 44 cases of autoimmune hypophysitis treated with glucocorticoids and/or azathioprine. A reduction in the size of the adenohypophysis was found in 84% of patients, the function of the adenohypophysis improved in 45% and that of neurohypophysis in 41% of these patients [5]. In our patient the majority of the hormone deficiency and all the symptoms had improved. The sizes of the pituitary and stalk were normalized following one month treatment with corticosteroid indicating the underlying autoimmune Etiology of lymphocytic hypophysitis and also showing that other inmuno supressive drugs can be used in the management of these cases. The role of corticosteroids in improving compression symptoms and as a replacement in lymphocytic hypophysitis is helpful in avoiding unnecessary transsphenoidal surgery [11]. Even though pituitary tissue biopsy was not done, on the basis of marked clinical response and MRI normalization following to glucocorticoid replacement strongly suggests lymphocytic hypophysitis [12]. There are different explanations why lympocytic hypophysitis occurs during the peripartal period, according to O’Dwyer, et al [11] described the strong association of pregnancy and pituitary autoimmunity with the production of pituitary autoantibodies by patients that recognize a target auto antigen protein identified as alpha-enolase from the placenta. They also described another antibody, the neuronal specific enolase (NSE) which is expressed in both pituitary and placenta cell that establishes the direct link between pituitary and placental autoantigens. This gives a theoretical basis for the occurrence of lymphocytic hypophysitis in the peripartum period though it needs further verification with more studies [11].
Conclusion
Lymphocytic hypophysitis should be considered in the differential diagnosis of women who present with pituitary enlargement during late pregnancy and post-partum period. Close clinical evaluation and monitoring for multiple hormone deficiencies is required. Early treatment with pulse steroids may avoid unnecessary surgery. It is suggested that long-term follow-up with hormonal and MRI studies are necessary.
References
- Rabinovich H, Del Pozo Pico C, Varela da Ousa C (2008) Clinical practice guideline for the diagnosis and treatment of hypophysitis. Endocrinol Nutr 55: 44-53.
- Diego E, Ciudin A, Simo-Servat O, Ortiz A, Gutierrez-Carrasquilla L, et al. (2015) A Case Report of Lymphocytic Hypophysitis Related to Pregnancy. Open Journal of Endocrine and Metabolic Diseases 5: 171.
- Naran J, Can AS (2020) Lymphocytic Hypophysitis. StatPearls [Internet]
- Falorni A, Minarelli V, Bartoloni E, Alunno A, Gerli R (2014) Diagnosis and classification of autoimmune hypophysitis. Autoimmun Rev 13: 412-416.
- Lupi I, Manetti L, Raffaelli V, Lombardi M, Cosottini M, et al. (2011) Diagnosis and treatment of autoimmune hypophysitis: a short review. J Endocrinol Invest 34: e245-e252.
- Faje A (2016) Hypophysitis: evaluation and management. Clin Diabetes Endocrinol 2: 15.
- Caturegli P, Newschaffer C, Olivi A, Pomper MG, Burger PC, et al. (2005) Autoimmune hypophysitis. Endocr Rev 26: 599-614.
- Bellastella A, Bizzarro A, Coronella C, Bellastella G, Sinisi AA, et al. (2003) Lymphocytic hypophysitis: a rare or underestimated disease? Eur J Endocrinol 149: 363-376.
- Imber BS, Lee HS, Kunwar S, Blevins LS, Aghi MK (2015) Hypophysitis: a single-center case series. Pituitary 18: 630-641.
- Molitch ME, Gillam MP (2007) Lymphocytic hypophysitis. Horm Res Paediatr 68: 145-150.
- O’dwyer DT, Clifton V, Hall A, Smith R, Robinson PJ, et al. (2002) Pituitary Autoantibodies in Lymphocytic Hypophysitis Target Both γ-and a-Enolase–A Link with Pregnancy? Arch Physiol Biochem 110: 94-98.
- Khare S, Jagtap VS, Budyal SR, Kasaliwal R, Kakade HR, et al. (2015) Primary (autoimmune) hypophysitis: a single centre experience. Pituitary 18: 16-22.
- Gutenberg A, Larsen J, Lupi I, Rohde V, Caturegli P (2009) A radiologic score to distinguish autoimmune hypophysitis from nonsecreting pituitary adenoma preoperatively. AJNR Am J Neuroradiol 30: 1766-1772.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Mamo AG, Tarekegn G, Mekonnen A, Endale A (2022) Post-partum Lymphocytic Hypophysitis in Ethiopian Woman. J Obes Metab 5: 110. DOI: 10.4172/jomb.1000110
Copyright: © 2022 Mamo AG, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 1899
- [From(publication date): 0-2022 - Apr 04, 2025]
- Breakdown by view type
- HTML page views: 1409
- PDF downloads: 490