Postpartum Depression: Understanding the Silent Struggle of New Mothers
Received: 03-May-2023 / Manuscript No. JCPHN-23-98088 / Editor assigned: 05-May-2023 / PreQC No. JCPHN-23-98088 (PQ) / Reviewed: 19-May-2023 / QC No. JCPHN-23-98088 / Revised: 22-May-2023 / Manuscript No. JCPHN-23-98088 (R) / Published Date: 29-May-2023 DOI: 10.4172/2471-9846.1000410
Abstract
The birth of a child is often described as one of life's greatest joys. However, for many women, this experience can be marred by a condition known as postpartum depression (PPD). PPD is a serious mental health disorder that affects up to 1 in 7 women following childbirth. Despite its prevalence, PPD is often misunderstood and stigmatized, leaving many women to suffer in silence. In this article, we will explore the causes, symptoms, and treatment options for postpartum depression.
Keywords
Postpartum depression; Healthcare; Women
Introduction
Postpartum depression is believed to be caused by a combination of hormonal, psychological, and environmental factors. The rapid changes in hormone levels that occur after childbirth can trigger mood swings and other symptoms of depression. Additionally, new mothers may experience a range of stressors, such as sleep deprivation, physical discomfort, and the demands of caring for a new-born, which can contribute to feelings of overwhelm and hopelessness [1].
Methodology
Psychological factors, such as a history of depression or anxiety, can also increase a woman's risk of developing PPD. Other risk factors for PPD include a lack of social support, financial stress, and a difficult childbirth experience.
Symptoms of postpartum depression
PPD can present in a variety of ways and can range from mild to severe. Some common symptoms of PPD include:
Feelings of sadness, emptiness, or hopelessness
Difficulty sleeping or sleeping too much
Loss of interest in activities that was once enjoyable
Difficulty bonding with the baby
Changes in appetite or weight
Fatigue or loss of energy
Thoughts of self-harm or suicide
It is important to note that many new mothers experience "baby blues," a mild and temporary condition that involves mood swings, anxiety, and tearfulness. However, if these symptoms persist or worsen over time, it may be a sign of PPD [2, 3].
Treatment for postpartum depression
The good news is that postpartum depression is treatable, and with the right care, most women are able to make a full recovery. Treatment options for PPD may include:
Therapy: Cognitive-behavioural therapy (CBT) and interpersonal therapy (IPT) are both effective in treating PPD. These types of therapy can help new mothers identify and change negative thought patterns, develop coping skills, and improve communication with loved ones.
Medication: Antidepressant medications can be helpful in treating PPD. These medications work by balancing the levels of certain chemicals in the brain that affect mood and emotions.
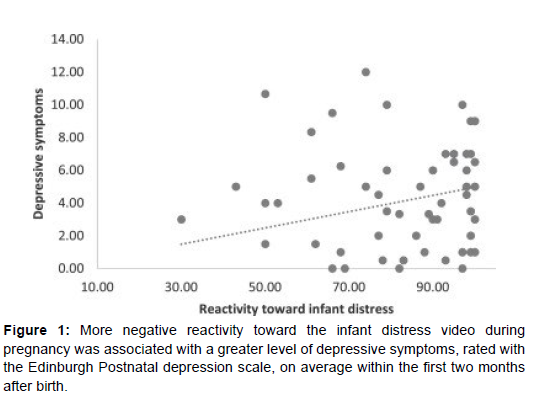
Support groups: Joining a support group for new mothers can provide a safe space for women to share their experiences and receive emotional support from others who are going through similar struggles (Figure 1).
Lifestyle changes: Simple changes such as getting enough sleep, eating a healthy diet, and engaging in regular exercise can also be helpful in managing PPD symptoms [4, 5].
It is important for women with PPD to seek help as soon as possible. Left untreated, PPD can have long-lasting effects on both the mother and the child, including developmental delays and problems with bonding.
Breaking the stigma of postpartum depression
Despite its prevalence, postpartum depression is often stigmatized, leaving many women feeling ashamed or embarrassed to seek help. One of the most effective ways to combat this stigma is to increase awareness and education about PPD. By normalizing the experience of PPD and encouraging women to seek help, we can create a culture that is more supportive and understanding of new mothers [6, 7].
Additionally, healthcare providers can play a critical role in identifying and treating PPD. By routinely screening new mothers for PPD and providing appropriate resources and referrals, healthcare providers.
It is important to note that many women experience a temporary period of mood changes, known as the "baby blues," in the first few weeks after giving birth. However, if these symptoms persist for longer than two weeks or become more severe, it may be a sign of PPD and requires medical attention.
Treatment options for postpartum depression
The good news is that PPD is a treatable condition. Treatment options include therapy, medication, or a combination of both.
Therapy: Talk therapy, or psychotherapy, is often the first line of treatment for PPD. Cognitive-behavioural therapy (CBT) and interpersonal therapy (IPT) are two common types of therapy used to treat PPD. CBT focuses on changing negative thought patterns, while IPT helps women identify and improve relationships that may be contributing to their depression [8,9].
Medication: Antidepressant medication can be effective in treating PPD, particularly for women with moderate to severe symptoms. Selective serotonin reuptake inhibitors (SSRIs) are a type of medication commonly prescribed for PPD. It is important to note that not all medications are safe to use while breastfeeding, so it is essential to consult with a healthcare provider before starting any medication.
Self-care: In addition to therapy and medication, self-care can also play an essential role in treating PPD. Self-care activities may include getting enough sleep, eating a healthy diet, exercising, and finding ways to reduce stress and anxiety.
Becoming a mother can be one of the most joyous and fulfilling experiences of a woman's life. However, the postpartum period can also be a time of great stress and emotional turmoil for some women. Postpartum depression (PPD) is a common mental health disorder that affects many women after giving birth. In this article, we will discuss the causes, symptoms, and treatment options for postpartum depression.
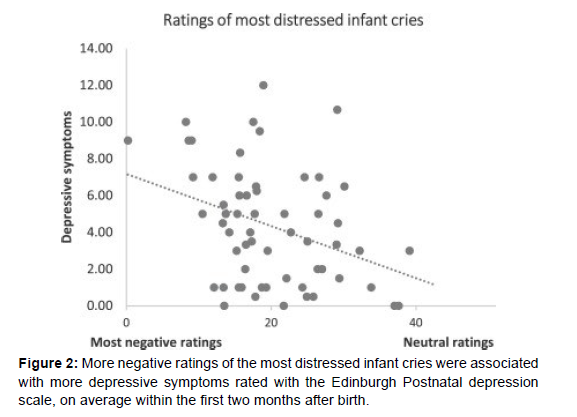
The exact causes of PPD are not fully understood, but it is believed to be a combination of biological, psychological, and social factors.Hormonal changes during pregnancy and childbirth can cause fluctuations in the levels of oestrogen and progesterone, which can affect a woman's mood and emotional well-being. Additionally, the stress and physical demands of caring for a new-born can also contribute to the development of PPD (Figure 2).
Other risk factors for PPD include a history of depression or anxiety, a lack of social support, financial stress, and relationship difficulties. Women who have experienced a traumatic birth or have a history of trauma or abuse are also at an increased risk of developing PPD [10].
Conclusion
Postpartum depression is a common mental health disorder that affects many women after giving birth. The causes of PPD are complex and can include hormonal changes, stress, and social factors. Symptoms of PPD may include feelings of sadness, hopelessness, and worthlessness, as well as changes in appetite and sleep patterns. Treatment options for PPD include therapy, medication, and self-care. It is important for women to seek medical attention if they experience persistent or severe symptoms of PPD. With the right treatment and support, women with PPD [11, 12].
References
- Jha A, Kumar A (2019) Biobased technologies for the efficient extraction of biopolymers from waste biomass. Bioprocess Biosyst Eng 42: 1893-1901.
- Martău GA, Mihai M, Vodnar DC (2019) The Use of Chitosan, Alginate, and Pectin in the Biomedical and Food Sector-Biocompatibility, Bioadhesiveness, and Biodegradability. Polymers 11: 1837.
- Adhikari BB, Chae M, Bressler DC (2018) Utilization of slaughterhouse waste in value-added applications: Recent advances in the development of wood adhesives. Polymers 10: 176.
- Fang Y, Guo S, Phillips GO (2014) Soy proteins: A review on composition, aggregation and emulsification. Food Hydrocoll 39: 301-318.
- Benítez JJ., Castillo PM, del Río JC, León-Camacho M, Domínguez E, et al.(2018) Valorization of Tomato Processing by-Products: Fatty Acid Extraction and Production of Bio-Based Materials. Materials 11: 2211.
- Tran D-T, Lee HR, Jung S, Park MS, Yang J-W (2018) Lipid-extracted algal biomass based biocomposites fabrication with poly(vinyl alcohol) . Algal Res 31: 525-533.
- Damm T, Commandeur U, Fischer R, Usadel B, Klose H (2016) Improving the utilization of lignocellulosic biomass by polysaccharide modification. Process Biochem 51: 288–296.
- Valdés A, Mellinas AC, Ramos M, Garrigós MC, Jiménez A (2014) Natural additives and agricultural wastes in biopolymer formulations for food packaging. Front Chem 2.
- Shankar S, Tanomrod N, Rawdkuen S, Rhim J-W (2016) Preparation of pectin/silver nanoparticles composite films with UV-light barrier and properties. Int J Biol Macromol 92: 842-849.
- da Silva ISV, de Sousa RMF, de Oliveira A, de Oliveira WJ, Motta LAC, et al. (2018) Polymeric blends of hydrocolloid from chia seeds/apple pectin with potential antioxidant for food packaging applications. Carbohydr. Polym 202: 203-210.
- Wei H, Wang EK (2013) Nanomaterials with enzyme-like characteristics (nanozymes): Next-generation artificial enzymes. Chem Soc Rev 42: 6060-6093.
- Gao LZ, Zhuang J, Nie L, Zhang JB, Zhang Y, et al.(2007) Intrinsic peroxidase-like activity of ferromagnetic nanoparticles. Nat Nanotechnol 2: 577-583.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Lyme A (2023) Postpartum Depression: Understanding the SilentStruggle of New Mothers. J Comm Pub Health Nursing, 9: 410. DOI: 10.4172/2471-9846.1000410
Copyright: © 2023 Lyme A. This is an open-access article distributed under theterms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1008
- [From(publication date): 0-2023 - Dec 19, 2024]
- Breakdown by view type
- HTML page views: 917
- PDF downloads: 91