Post-Operative Outcome of Achilles Tendon Injury Treated with Knotless Percutaneous Achilles Repair System
Received: 02-Feb-2018 / Accepted Date: 08-Mar-2018 / Published Date: 15-Mar-2018 DOI: 10.4172/2329-910X.1000263
Abstract
Background: The Achilles tendon is the most frequently ruptured tendon in the body and its incidence is increasing, more so among athletes. Various surgical techniques exist for treating it and one of these is as discussed in this study, Achilles tendon injury treated with Knotless PARS (Arthrex) that allows for earlier weight bearing and mobilization and, therefore, faster rehabilitation and an improved functional outcome.
Aim: The post-operative progress of patients, specifically athletes subset with Achilles tendon injury treated with Knotless PARS is discussed in this article using Newcastle Orthopaedic Foot and Ankle Score (NOFAS).
Methods: We retrospectively evaluated the patients operated on between March 2015 and January, 2017, 19 feet of 19 patients diagnosed with acute Achilles tendon rupture were treated. All clinical outcomes were examined using the Newcastle Orthopaedic Foot and Ankle Score (NOFAS) in patients operated in the last 28 months after the operation. We measured their progress in 3 categories as follows: (1) Improvement in pain and symptoms. (2) Recovery and lifestyle improvement and (3) Motion and activity.
Conclusion: The study suggests that the post-operative progress of patients with Achilles tendon injury treated with Knotless PARS (Arthrex) is strong, but the best results only appear in patients post 12 months of their surgery. We suggest, prospective and comparative studies will help for further research of this subject.
Keywords: Achilles tendon; Knotless PARS; NOFA score; Fiber wire suture; PARS jig; Swivelocks
Introduction
Achilles tendon is the most commonly ruptured tendon in the body and its incidences are ever growing, particularly in atheletes [1-3]. The management of acute ruptures of the Achilles tendon is a controversial subject and hence there is extensive research done on it. Despite this, there is a split verdict on optimal management. The aim of treatment is tendon healing with restoration of function which can be achieved by conservative treatment. Hence, non-operative management believers argue that surgery is avoidable since it includes high risks of infections, wound complications and nerve injury. However, operative management has shown a significant reduction in the risk of rerupture and allows patients to return to sport and work quicker as compared to conservative measures [4-13]. Further, various studies have shown the importance of early mobilization on the tendon healing process, therefore surgery become a preferred choice, particularly in athletes who want to get back to pre-injury level of sports [6].
The object of our study was to determine the improvement in pain, range of motion, activity and symptoms. Also, to study the recovery and lifestyle improvements in patients treated surgically using Knotless Percutaneous Achilles Repair System (PARS).
Methods
We retrospectively evaluated the patients operated between March 2015 and January 2017. 19 feet of 19 patients diagnosed with acute Achilles tendon rupture were treated. The diagnosis of acute Achilles tendon rupture was based on physical findings, including palpation of the defect at the rupture site with tenderness, disappearance of tendon relief, and positive Simmonds-Thompson test. In all patients, an avulsion fracture of the calcaneus at the insertion of Achilles tendon was excluded by plain lateral radiograph of the affected ankle. All patients were informed in detail about conservative and operative therapy, and they selected the treatment method. Informed and written consent from all patients were obtained.
The inclusion criteria for this study were as follow: (1) Patients who were treated surgically by means of knotless PARS, (2) Patients who were injured during athletic activities and hoped to return to athletic activity, (3) Patients with no history of previous surgery on the affected lower extremity, (4) Patients with the healthy contralateral ankle, (5) None of the patients had a predisposition for Achilles tendon rupture, such as history of systemic use of corticosteroids, use of fluoroquinolones, prior injection to the Achilles tendon, or hyperthyroidism.
There were 15 male and 4 female patients with a mean age of 43 years (Range, 23-64 years). The right ankle was affected in 12 patients and the left ankle was affected in 7 patients. Cause of injury was as follows: Soccer in 8 patients, running in 2 patients, and cricket, dancing, hockey, netball, rugby, skiing, surfing and tennis in 1 patient each.
All patients underwent surgery in an average of 22 days of the athletic injury (Range: 5-62 days). None of the patients had a predisposition for Achilles tendon rupture, such as history of systemic use of corticosteroids, use of fluoroquinolones, prior injection to the Achilles tendon, or hyperthyroidism. Any delay in their treatment was usually because of delayed presentation and some delay to operate on an elective list. Delayed presentation to orthopaedic surgeon were mainly because of patient not aware of seriousness of injury, missed diagnosis by local doctor or emergency department or delay in confirming diagnosis with ultrasound imaging.
All clinical outcomes were examined using the Newcastle Orthopaedic Foot and Ankle (NOFA) Score in patients operated in the last 28 months after the operation. We measured their progress in 3 categories as follows: (1) Improvement in pain and symptoms (2) Recovery and lifestyle improvement and (3) Motion and activity. We recorded the number of months passed since their surgery to understand their recovery. We also recorded the intervals between the injury and the date of operation. Furthermore, since all patients sustained the injury during athletic activities and desired an early return to activity, we investigated whether each patient could return to their activities. If so, the intervals between the operation and the time when patients could return to athletic activities.
All statistical analyses were performed using responses to the NOFA questionnaire (Refer to NOFA Questionnaire in Annexure 1). Descriptive statistics were calculated, and all values are expressed as Newcastle Orthopaedic Foot and Ankle (NOFA) Score. Derivation of score is from the response of patients to the Questionnaire.
| Newcastle orthopaedic foot and ankle score questionnaire and calculation | ||||
| Sr.No. | Questions related to post-operative recovery | Yes | No | Sometimes |
| A | Pain and symptoms | |||
| 1 | Do you still experience pain after surgery? | 0 | 10 | 5 |
| 2 | Is your pain constant? | 0 | 5 | 2.5 |
| 3 | Does you experience pain in the evenings? | 0 | 5 | 2.5 |
| 4 | Does your foot feel normal? | 8 | 0 | 4 |
| 5 | Are these symptoms worse post-surgery? | 0 | 6 | 3 |
| 6 | Does your ankle feel stiff? | 0 | 2 | 1 |
| 7 | Does your ankle feel swollen? | 0 | 2 | 1 |
| 8 | Is there any problem with the sensation of your foot? | 0 | 2 | 1 |
| B | Recovery and lifestyle | |||
| 1 | Has your quality of life improved post-surgery? | 4 | 0 | 2 |
| 2 | Do you feel self-conscious about your foot/ankle? | 0 | 2 | 1 |
| 3 | Do you have trouble while balancing? | 0 | 2 | 1 |
| 4 | Do you need any support? | 0 | 2 | 1 |
| C | Motion and activity | |||
| 1 | Did the surgery increase your ability to perform day to day activities? | 6 | 0 | 3 |
| 2 | Are there any limitations in your activities? | 0 | 6 | 3 |
| 3 | Does it hurt when you do light activity? | 0 | 3 | 1.5 |
| 4 | Does it hurt when you do moderate activity? | 0 | 3 | 1.5 |
| 5 | Does it hurt when you do strenuous activity? | 0 | 2 | 1 |
| 6 | Do have any problems when you walk on different surfaces (like inclines, stairs, ladders) | 0 | 5 | 2.5 |
| 7 | Do you have any problems when walking on mildly uneven surfaces (rocks, bumps, etc.)? | 0 | 5 | 2.5 |
| 8 | Do you have any problems when walking on plain/flat surfaces (Sagittal Motion) | 0 | 5 | 2.5 |
| 9 | Does the pain in your foot disturb your sleep? | 0 | 5 | 2.5 |
| 10 | Do you have difficultly when you put on or take off your Shoes and socks? | 0 | 4 | 2 |
| 11 | Do you wear of shoes comfortably? | 3 | 0 | 1.5 |
| 12 | Do you have any pain after wearing these shoes? | 0 | 3 | 1.5 |
Annexure 1: NOFA Questionnaire.
Surgical Technique
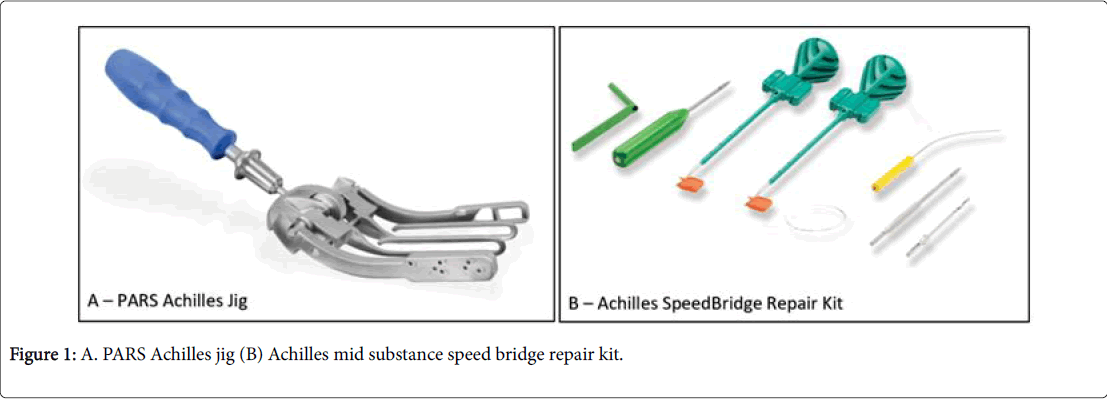
The PARS Achilles Jig and the Achilles midsubstance speedbridge repair kit is used for the procedure (Figure 1).
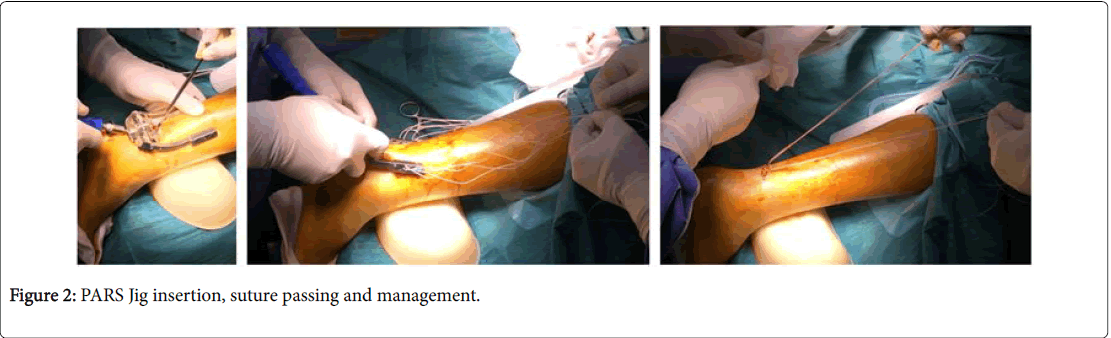
The inner arms of the PARS jig in the paratenon of the Achilles tendon in inserted through the incision (Figure 2). The PARS needle with the nitinol loop is passed through the #1 hole. The white #2 Fiber Wire® suture is pulled through the leg, leaving tails on both sides of equal length. Manual pressure is placed on the tendon, while passing the PARS needle to enhance central placement of the Fiber Wire. The PARS needle with the nitinol loop is passed through the #2 hole. The blue #2 Fiber Wire is pulled through the leg, leaving tails on both sides of equal length. The PARS needle with the nitinol loop is passed through the #3 and #4 holes. The white/green #2 Fiber Wire with loops is pulled through the leg, leaving tails on both sides of equal length. Here, it is ensured that there is one looped end on each side of the leg. The PARS needle with the Nitinol loop is passed through the #5 hole. The white/black #2 TigerWire® suture is pulled through the leg, leaving tails on both sides of equal length. The Jig is then removed. The sutures are organised in the way they were originally placed through the PARS Jig.
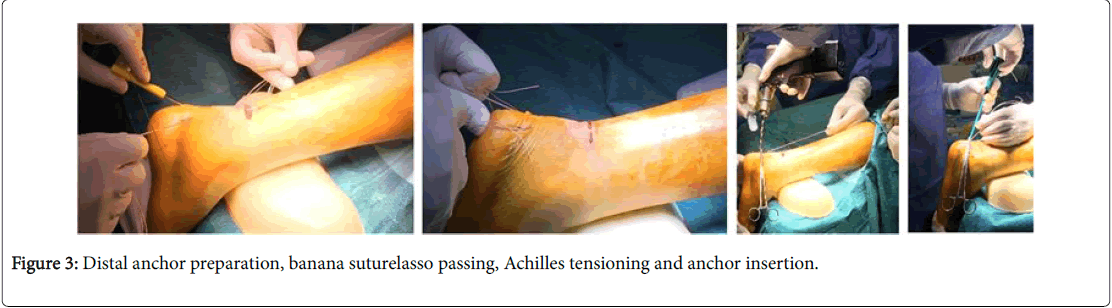
Then, the #2 blue suture is passed under the #3 and #4 looped sutures and back through the loop of the white/green looped suture (Figure 3). The #2 suture is pulled through the Achilles tendon to the other side by pulling on the non-looped side of the white/green looped sutures (#3 and #4). Pull on the #2 suture to lock the stitch in place. Two transverse sutures (#1 and #5) and one locked suture (#2) should now be on the left. Proximal options include #2 Fiber Loop suture or #2 Fiber Wire suture. Two stab incisions are made 1.5 cm apart over the calcaneus near the Achilles insertion and Drilled with the 3.5 mm drill using the drill guide. The tap is used to prepare the holes for the Swive Lock® anchor. The Banana Suture Lasso is passed through distal Achilles tendon and the proximal Fiber Wire® suture is retrieved. The 4.75 mm SwiveLocks is inserted. Note: Tension appropriately and Compare with contralateral foot. This results in a secure knotless repair of the Achilles tendon rupture. Sutures are cut flush with the anchor, and the surgeon performs wound irrigation and layered closure, with absorbable suture, of the paratenon and subcutaneous tissues. After skin closure with nylon suture, resting ankle plantar flexion is assessed and the Thompson test performed. The patient is placed in a well-padded non-weight-bearing plantar flexion splint for incision and initial tendon healing during the first 2 weeks after surgery.
Postoperative Rehabilitation Protocol
Post-operative protocol involves splint or cam boot immobilisation for 12 weeks with 8 weeks splinting in 45 degrees ankle plantarflexion and partial weight bearing. Wound was to be left intact for about 2 weeks before suture removal, and leg could be washed daily and range of motion exercises to the ankle. 8 weeks after surgery the patient was encouraged to fully weight bear in a neutral position in the cam boot. Physiotherapist was commenced at 8 weeks to encourage gait retraining, range of motion ankle exercises, calf strengthening and modalities. Patient was asked to take 300 mg aspirin daily while immobilized in splint or boot, but further anticoagulated if they were at greater risk of thromboembolic phenomenon. Light jogging was encouraged 3 months after the surgery and normal sports 4 to 6 months after surgery depending on physiotherapist’s recommendations.
Results
The mean NOFA score was high in most of the patients (Table 1). 14 out of 19 Patients said that their recovery was good to excellent. 5 out of 19 complained of ongoing pain and balancing issues. The most dramatic improvement averaged at 18 months post the date of the surgery. With the excellent results in those who were operated 19.29 ± 5.02 months ago. Followed with very good results in those operated 17.25 ± 3.5 months ago and good results in those operated 18.67 ± 5.13 months ago. The Results were fair in those operated 8.5 ± 2.12 months ago and poor in those operated 7.33 ± 1.15 months ago. Hence, the studies indicated a direct correlation between the number of months since the surgery and the NOFA score. The patient with a good NOFA score was only after 13 months post the surgery. All 5 Patients amongst the fair and poor NOFA Score bracket were operated as later as 10 months ago. Hence, it appears from the study, that with the passing months their NOFA Score is expected to get better.
| NOFA score range | Recovery | No. of patients out of 19 | Months since surgery | |
|---|---|---|---|---|
| Mean ± Standard deviation | Range | |||
| 90-100 | Excellent | 7 | 19.29 ± 5.02 | 14-28 Months |
| 80-90 | Very Good | 4 | 17.25 ± 3.5 | 13-21 Months |
| 70-80 | Good | 3 | 18.67 ± 5.13 | 13-23 Months |
| 60-70 | Fair | 2 | 8.5 ± 2.12 | 7-10 Months |
| Below 60 | Poor | 3 | 7.33 ± 1.15 | 6-8 Months |
| NOFA: Newcastle orthopaedic foot and ankle. | ||||
Table 1: Post-operative recovery analysis using NOFA Score.
Most patients were able to return to their sporting activities postsurgery (Tables 2 and 3). 10 out of 19 patients returned to their respective sports or alternate sports between 3 to 18 months postsurgery. Out of these 10 patients that returned to sports, 6 returned within 6 months, another 3 within 6-12 months and 1 within 12-18 months of the surgery. The NOFA score was good to excellent amongst these 11 patients. 4 out of the 9 patients indicated a NOFA score between 70 and 90. The reason they did not return to sports was sighted that they were able to return but were unwilling to return due to age or other personal reasons. Rest 5 out of the remaining 9 that did not return to the sports explained that they were still experiencing pain occasionally on exertion. The average number of months passed since their surgery was 8.5 Months (Range 7-10 Months) in patients with fair NOFA Score and 7.2 (Range 6-8 Months) in patients with poor NOFA Score. A patient with a good NOFA score was seen after approximately 13 months post-surgery. This finding supported that a patient needed at least 1 year to develop a Good NOFA Score, but the return to their sporting activity can begin as early as 3 months.
| Return to Sporting Activity | Months taken to Return to Sports post-surgery | No. of Patients | Avg. of Age of Patients | Months passed to date since Surgery Average (Range) | NOFA Score Average (Range) |
|---|---|---|---|---|---|
| Yes | 3 Months | 2 | 37 | 17.00 (13 - 21) | 91.75 (87.5 - 96) |
| 4 Months | 4 | 45.75 | 19.50 (15 - 28) | 88.62 (81 - 100) | |
| 10 Months | 1 | 42 | 20.00 (20 - 20) | 74.00 (74 - 74) | |
| 12 Months | 2 | 54 | 14.50 (14 - 15) | 92.50 (90.5 - 94.5) | |
| 18 Months | 1 | 37 | 22.00 (22 - 22) | 90.00 (90 - 90) | |
| No | - | 9 | 40.67 | 12.89 (6 - 23) | 69.50 (46 - 90) |
| Total | - | 19 | 43.33 | 15.74 (6 - 28) | 79.60 (46 - 100) |
Table 2: No. of People that were able to return to sporting activities explained.
| Results as per NOFA score | No. of patients | Average of NOFA score | Average of age | Average of months since surgery (Range) |
|---|---|---|---|---|
| Excellent | 1 | 90 | 51 | 20 (20 - 20) |
| Very Good | 1 | 86 | 54 | 21 (21 - 21) |
| Good | 2 | 75.3 | 32.5 | 18 (13 - 23) |
| Fair | 2 | 67.8 | 26 | 8.5 (7 - 10) |
| Poor | 3 | 54.5 | 48 | 7.3 (6 - 8) |
| Grand Total | 9 | 69.5 | 40.7 | 12.9 (6 - 23) |
Table 3: Details of Patients that did not return to sports.
Discussion
Treatment options for Acute Achilles Tendon Rupture include conservative and operative management. It’s difficult to reach a consensus on the optimal treatment with good clinical outcomes and no complications [7,8,11,14-17]. Recently, there are several studies that have compared the 2 approaches. The Meta-analysis performed by Soroceanu et al. [16] did 10 randomized controlled trials and reported that the re-rupture rates were equal in both surgical and nonsurgical patients. However, when functional rehabilitation with early range of motion was used, surgical patients returned to work 19.16 days sooner. Another research conducted by Willitis et al. [17] on 144 patients who underwent accelerated rehabilitation, including early weight-bearing and early range of motion exercises with or without surgical intervention and reported no differences in the re-rupture rate, ankle range of motion, and calf circumference or function. However, the plantar flexion ratio at 1 and 2 years after treatment showed significant differences in favour of the surgical group. This was contradicted by Jones et al. [8] study that researched 1085 patients and reported that surgical repair significantly reduced the re-rupture rate compared to non-operative treatment. Similar conclusion was drawn in the Wilkins et al. [17] randomized study of 677 patients. Hence, from the above studies, we see that the surgical approach would be more optimal than the conventional approach.
Next came the question of the effectiveness of open repair versus percutaneous repair for an acute Achilles tendon rupture. From a comparative paper by Krueger and David et al. [18] that aimed at solving the controversy over which repair is superior, with focused questions on which type of surgery is better in providing the best overall patient outcome, open or percutaneous repair, in physically active men and women with acute Achilles tendon ruptures, concluded that “percutaneous repair is the best option for Achilles tendon surgery when it comes to the physically active population. Percutaneous repair has faster surgery times, less risk of complications, and faster recovery times over having an open repair, although it is acknowledged that every patient has a different situation and best individual option may vary patient to patient.” This was in lines with the study by Cottom et al. [19] that investigated the biomechanical strength of 3 different techniques for Achilles tendon repair in a cadaveric model. The results of the study showed “a clear trend toward a stronger construct in Achilles repair using a knotless suture anchor technique, which might translate to a faster return to activity and be more resistant to an early and aggressive rehabilitation protocol.”
Achilles tendon ruptures are common in the elite and recreational athlete and most often occur in the non-insertional region of the tendon complex [20-22]. Therefore, most surgeons involved in the treatment of athletes with acute Achilles tendon rupture agree that those who desire an early return to athletic activities tend to recommend surgical therapy to enable earlier weight bearing and mobilization, lessen the risk of re-rupture and therefore, faster rehabilitation and an improved functional outcome [16,23]. Additionally, soft tissue problems have been one of the main complications described in the literature following operative management [24,25]. Knotless Pars is a minimally invasive technique that intends to reduce this complication [26,27]. Its minimal incision reduces risk of wound complications and it provides the ability to create a locking stitch, making it stronger [26].
The review studies by Ververidis et al. [3] illustrated that in thirteen studies, including 670 patients, re-rupture rate was very low with the most frequent complication being sural nerve damage. Average functional outcomes were reported satisfying with 91.4% patients continuing to practice sports after surgery. Furthermore, 78–84% returned to the same or higher sports level. Average time of return was 18 weeks in 9 studies. We used an in-house designed questionnaire to analyse improvements in patients post-surgery. Contradictory to the above report, our study did not have any patients with nerve injury complication. We did not have any patients report any other complications such as infection or re-rupture till date. It was seen that the symptomatic relief and range of motion was successfully gained as early as 3 months, but the Lifestyle improvement was a challenge and took a long time for most patients. The average NOFA score was high in most of the patients (Table 1). 74% Patients said that their recovery was good to excellent. These patients reported that they could return to the same or higher level of sports, which is in line with the previous study. Rest of the 26% complained of ongoing pain and balancing issues. Many of these answered that despite their ability to return to sports, they chose not to simply because of the lack of confidence. We excluded them from the section of people who could return to sports for better authenticity of our results. Hence, studies indicated that the longer were the number of months since the surgery, the NOFA score improved. The most significant improvement averaged at 18 months post the date of the surgery. The patient with a good NOFA score was only after 13 months post the surgery. All 5 Patients amongst the Fair and Poor NOFA Score bracket were operated as late as 10 months ago. Hence, it appears, that with the passing months their NOFA Score is expected to get better. A repeat analysis of the further progress and a revised NOFA score of these 4 patients will depict if the complete recovery time in all aspects of the NOFA Score is above 12 months.
Conclusion
In Conclusion, the study suggests that the post-operative progress of patients with Achilles Tendon Injury treated with Knotless PARS is excellent, but the best results appear in patients post 12 months of their surgery.
Declaration of Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Leppilahti J, Puranen J, Orava S (1996) Incidence of achilles tendon rupture. Acta Orthop Scand 67: 277–279.
- Maffuli N, Waterston SW, Squair J, Reaper J, Douglas AJ (1999) Changing incidence of achilles tendon rupture in Scotland: A 15-year study. Clin J Sports Med 9: 157–160.
- Ververidis AN, Kalifis KG, Touzopoulos P, Drosos GI, Tilkeridis KE, et al. (2015) Percutaneous repair of the achilles tendon rupture in athletic population. J Orthop 13: 57–61.
- Bhandari M, Guyatt GH, Siddiqui F, Morrow F , Busse J , et al. (2002) Treatment of acute achilles tendon ruptures: A systematic review and meta-analysis. Clin Orthop Relat Res 400: 190–200.
- Cetti R, Christiansen SE, Ejsted R, Jensen NM, Jorgensen U (1993) Operative versus nonoperative treatment of achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med 21: 791–799.
- Holms C, Kjaer M, Eliasson P (2015) Achilles tendon rupture treatment and complications: A systematic review. Scand J Med Sci Sports 25: 1–10.
- Jiang N, Wang B, Chen A, Dong F Yu B (2012) Operative versus nonoperative treatment for acute achilles tendon rupture: A meta-analysis based on current evidence. Int Orthop 34: 765–773.
- Jones MP, Khan RJ, Carey Smith RL (2012) Surgical interventions for treating acute achilles tendon rupture: Key findings from a recent cochrane review. J Bone Joint Surg Am 94: 1-6.
- Khan RJ, Fick D, Keogh A, Crawford J, Brammar T, et al. (2005) Treatment of acute achilles tendon ruptures. A meta-analysis of randomized, controlled trials. J Bone Joint Surg Am 87: 2202–2210.
- Lo IK, Kirkley A, Nonweiler B, Kumbhare DA (1997) Operative versus nonoperative treatment of acute achilles tendon ruptures: A quantitative review. Clin J Sport Med 7: 207–211.
- Wilkins R, Bisson LJ (2012) Operative versus nonoperative management of acute achilles tendon ruptures: A quantitative systematic review of randomized controlled trials. Am J Sports Med 40: 2154–2160.
- Wong J, Barrass V, Maffuli N (2002) Quantitative review of operative versus non operative management of achilles tendon ruptures. Am J Sports Med 30: 565–575.
- Zhao HM, Yu GR, Yang YF, Zhou JQ, Aubeeluck A (2011) Outcomes and complications of operative versus non-operative treatment of acute achilles tendon rupture: A meta- analysis. Chin Med J 124: 4050–4055.
- McWilliam JR, Mackay G (2016) The internal brace for midsubstance achilles ruptures. Foot Ankle Int 37: 794–800.
- Byrne PA, Hopper GP, Wilson WT, Mackay GM (2017) Knotless repair of achilles tendon rupture in an elite athlete: Return to competition in 18 weeks. J Foot Ankle Surg 56: 121-124.
- Soroceanu A, Sidhwa F, Aarabi S, Kaufman A, Glazebrook M (2012) Surgical versus nonsurgical treatment of acute achilles tendon rupture: A meta-analysis of randomized trials. J Bone Joint Surg Am 94: 2136-2143.
- Willits K, Amendola A, Bryant D, Mohtadi NG, Giffin JR, et al. (2010) Operative versus nonoperative treatment of acute achilles tendon ruptures: A multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg Am 92: 1767-2775.
- Krueger H, David S (2016) The effectiveness of open repair versus percutaneous repair for an acute achilles tendon rupture. J Sport Rehab 25: 404-410.
- Cottom JM, Baker JS, Richardson PE, Maker JM (2017) Evaluation of a new knotless suture anchor repair in acute achilles tendon ruptures: A biomechanical comparison of three techniques. J Foot Ankle Surg 56: 423-427.
- Rompe JD, Furia JP, Maffulli N (2008) Mid-portion achilles tendinopathy-current options for treatment. Disabil Rehabil 30: 1666–1676.
- Egger AC, Berkowitz, MJ (2017) Achilles tendon injuries. Curr Rev Musculoskelet Med 10: 72-80.
- Krill MK, Borchers JR, Hoffman J, Krill ML, Hewett T (2017) Effect of position, time in the season and playing surface on achilles tendon ruptures in NFL games: A 2009-10 to 2016-17 review. Phys Sportsmed 45: 259-264.
- Metz R, Kerkhoffs GM, Verleisdonk EJ, van der Heijden GJ (2007) Acute Achilles tendon rupture: Minimally invasive surgery versus non operative treatment, with immediate full weight bearing. Design of a randomized controlled trial. BMC Musculoskelet Disord 8: 108.
- Gulati V, Jaggard M, Al-Nammari SS, Uzoigwe C, Gulati P, et al. (2015) Management of achilles tendon injury: A current concepts systematic review. World J Orthop 6: 380–386.
- Pedowitz D, Kirwan G (2013) Achilles tendon ruptures. Curr Rev Muskuloskelet Med 6: 285–293.
- Hsu AR (2016) Limited incision knotless achilles tendon repair. Am J Orthop 45: 487-492.
- Clanton TO, Haytmanek CT, Williams BT, Civitarese DM, Turnbull TL, et al. (2015) A biomechanical comparison of an open repair and 3 minimally invasive percutaneous achilles tendon repair techniques during a simulated, progressive rehabilitation protocol. Am J Sports Med 43: 1957-1964.
Citation: Batra AV, O’Sullivan J, Nicholson D, Rao P (2018) Post-Operative Outcome of Achilles Tendon Injury Treated with Knotless Percutaneous Achilles Repair System. Clin Res Foot Ankle 6: 263. DOI: 10.4172/2329-910X.1000263
Copyright: © 2018 Batra AV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8415
- [From(publication date): 0-2018 - Apr 19, 2025]
- Breakdown by view type
- HTML page views: 7351
- PDF downloads: 1064