Polyostotic Fibrous Dysplasia of Maxillofacial Region: A Case Report
Received: 19-Dec-2017 / Accepted Date: 10-Jan-2018 / Published Date: 17-Jan-2018 DOI: 10.4172/2376-032X.1000224
Abstract
Conditions in which normal bone is replaced with fibrous tissue containing abnormal bone or cementum constitute group of pathologies bone dysplasias. These pathologies should be differentiated from tumours, because the treatments of these pathologies are very different.
Types of Fibrous dysplasia are monostotic, polyostotic or may occur as a component of McCune-Albright syndrome and Mazabraud syndrome. The most commonly affected bones are long bones, skull bones and ribs are. We present a case of polyostotic fibrous dysplasia in a 25 years old male patient.
Keywords: Bone dysplasias; Fibroosseous lesion; Maxilla; Mandible; Femur
Introduction
The pathologic lesions of Fibrous Dysplasia are a genetic non-inherited condition caused by missense mutation in the GNAS1 gene on chromosome 20.
The occurrence is equal proportions in males and females, usually during the first two decades of life.
If fibrous dysplasia is considered with bone tumors, then they comprises nearly 1% of primary bone tumors and 5%-7% of benign bone tumors [1,2].
Fibrous Dysplasia usually occur in childhood or early adolescence, more than two third of patients had onset of this pathologic condition before 20 years of age.
The time difference between onset of symptoms and clinical presentation varied from months to years in various articles.
Most of patients remained undiagnosed for a long period of time and may present later with maxillofacial pathologic lesions equivalent to our case [1,2]
Case Presentation
A male patient 25 years of age reported to our department of Oral Medicine and Radiology, NIMS Dental College, with a chief complaint of absence of some teeth which he want to get it replaced and also complains of disfigurement of the left side of face since approximately 15 years.
He was apparently alright 8 years before, but afterwards he gradually felt loosening of his teeth which, with time exfoliated.
Patient also noticed gradual enlargement of the prominence of left cheek bone along with the growth over the lower left jaw since 15 years.
Now patient noticed that the bone growth is stagnant since 2 years.
Medical history revealed patient has taken orthopaedic consultation few months back, for the reason that he feels intermittent pain on walking, climbing stairs and sitting on knees.
No significant finding was noticed in the family regarding similar kind of problems in his parents or siblings.
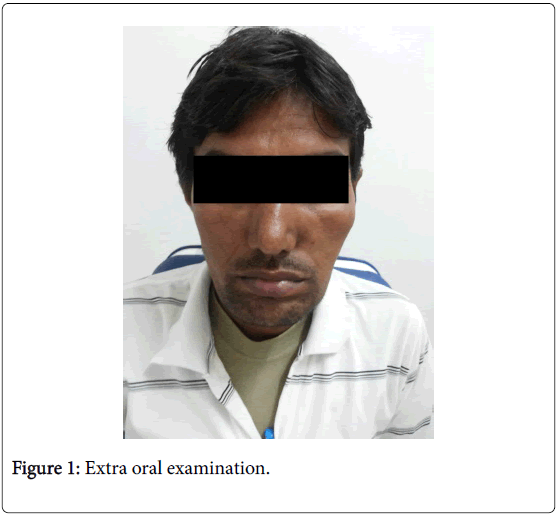
Extra oral examination revealed asymmetrical face with abnormally enlarged left malar prominence, similar lesion measuring about 2 cm in diameter present over the body of the left mandible (Figure 1).
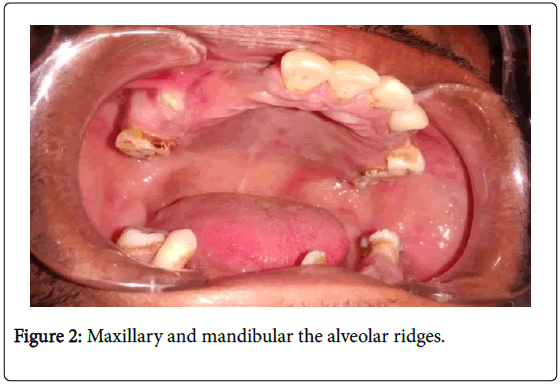
On palpation swelling was non tender and bony hard in consistency. Intra orally there were multiple missing teeth in both maxillary and mandibular the alveolar ridges (Figure 2).
On the basis of above findings the case was provisionally diagnosed as Bony dysplasia of left side of the face along with Partially edentulous upper and lower alveolar ridges.
The differential diagnosis of Fibrous Dysplasia, Paget’s disease and Osteoma of jaws was made.
Following which, Radiographic and Heamtological investigations were advised. IOPA, Occlusal (Figure 3) and OPG revealed multilocular radiolucencies with expansion of buccal cortical plate in relation to left body of mandible.
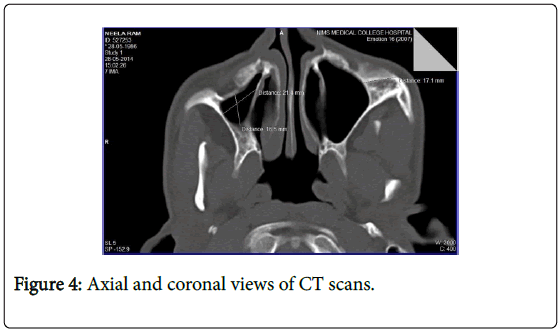
Axial and coronal views of CT scans revealed enlargement of left body of Zygoma (Figure 4).
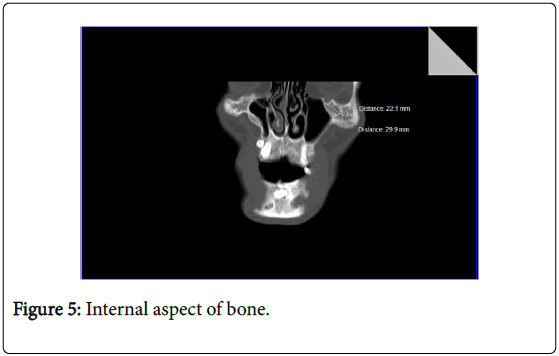
The internal aspect of bone showed abnormal trabeculae pattern with more radiopacity mimicking ground glass appearance (Figure 5).
Axial, Coronal and Panoramic views of CT mandible shows multilocular radiolucency involving body of the mandible bilaterally. There is expansion of cortical plates of the body of the mandible with multiple intraosseous radiolucent areas resembling the cyst surrounded with sclerotic rim.
These radiolucent areas gave the Hounsfield Unit of 800-1000 as compared to the 1800 Hounsfield Unit of regular cancellous bone indicating that normal cancellous bone is being replaced by abnormal fibrous tissue. Radiograph of pelvic region revealed multilocular areas in femoral head and iliac bone.
Biopsy was performed from left body of mandible which revealed ‘C’ shaped bony trabeculae not lined by osteocytes and osteoblasts, surrounded by fibrous connective tissue indicating that normal cancellous bone is being replaced by abnormal fibrous tissue.
Haematological investigations revealed high levels of serum calcium (11.45 mg/dl) and high levels of serum alkaline phosphatase (343.4 IU/L).
Considering the clinical manifestations, conventional radiographic and CT scan finding along with histopathological picture the above findings are suggestive of polyostotic fibrous dysplasia.
Discussion
Etiology of fibrous dysplasia has been related with a mutation in the GNAS1 gene that encodes the alpha subunit of the stimulatory G protein-coupled receptor, Gsα, and is located at chromosome 20q13.2-13.3.1. Their is activating mutations that occurs postzygotically, replacing the arginine residue amino acid with either cysteine or histidine amino acid. Cells which derive from the mutated cells manifest the dysplastic changes [3].
Fibrous Dysplasia is considered as "benign lesion, probably developmental in nature, characterized by presence of fibrous connective tissue with a characteristic whorled pattern and containing trabeculae of immature non-lamellar bone". Some authors defines fibrous dysplasia of craniofacial bones "as a benign, non-neoplastic intramedullary cellular proliferation of fibroblasts, with formation of irregular trabeculae of bone and or ovoid calcifications that shows indistinct, non-encapsulated borders" [4-6].
It was first described in 1891, by von Recklinghausen as fibrous dysplasia of bones under the term 'Osteitis fibrosacystica'. Another author Freund in 1934 named FD as 'osteitis fibrosa localizata/disseminata'.
In 1937 Jacobson in his extensive review of jaw bone lesions considered it as ‘Fibrous Dystrophy' whereas Albright in 1937 named it as Albright's syndrome, which constitute triad of polyostotic fibrous dysplasia, cutaneous pigmentation and endocrine disturbances.
Another author in 1938 Lichtenstein coined the term 'Fibrous Dysplasia of bone' and described it as a different entity of unknown etiology. In 1942 Lichtenstein and Jaffe' named according to clinical manifestations for fibrous dysplasia that is solitary (monostotic) and multiple (polyostotic) forms. Jaffe' in 1958, suggested term 'Fibroosseous Dysplasia' for fibrous dysplasia [4-6].
Patients with FD have bone deformity and facial asymmetry was more common compared to normal patients. The high incidence of bone deformities was mainly due to delayed presentation. Bones that are most commonly involved were maxilla and mandible in skull region followed by femur, tibia, humerus and ribs [6].
Polyostotic fibrous dysplasia has its onset mainly in children younger than 10 years of age and the lesions grow with the child and stabilize after puberty. The ratio of occurrence of polyostotic to monostotic fibrous dysplasia is 3:7. Gender prevalence of monostotic and polyostotic fibrous dysplasia is equal.
In patients with polyostotic disease, the most commonly involved bones are the craniofacial bones, ribs, and metaphysis or diaphysis of the proximal femur or tibia and the lesions are often found on one side of the body the monostotic presentation is more frequent, and lesions enlarge in proportion to skeletal growth [7-9].
The occurrence of polyostotic is less. But some adolescence patients have widespread polyostotic fibrous dysplasia may have severe deformities. The lesions Polyostotic lesions often continue to enlarge after skeletal maturity and causes progressive deformity and increase in pathologic fractures [8-10]. Patients with early fibrous dysplasia have radiolucent with either ill-defined or well defined borders and may have unilocular or multilocular lesions as seen in our case.
When the lesions mature, the bony defects acquire a mixed radiolucent/radiopaque appearance and latter stage fibrous dysplasia exhibits mottled radiopaque patterns, often described as resembling ground glass (in our case it is seen in left zygoma), orange peel, or fingerprints, with ill-defined borders which were blending into the normal adjacent bone [11,12].
Sometimes radiolucent regions resembling cysts may occur in mature lesions of fibrous dysplasia. These are bone cavities that appear to simple bone cysts as similarly found in present case. In cases of polyostotic form, there will be increases in alkaline phosphatase and osteocalcin mostly; in our case also alkaline phosphatase was raised [11,12].
Fibrous dysplasia has histologic features of delicate trabeculae of immature bone, with no osteoblastic rimming, enmeshed within a bland fibrous stroma of dysplastic spindle shaped cells without any cellular features of malignancy.
Ratio of fibrous tissue to bone ranges from fields that are totally fibrous to fields filled with dysplastic trabeculae. Degree of haziness shown radiographically in given fibrous dysplasia lesion directly correlates with its underlying histopathologic condition.
The areas with more radiolucent lesions were composed of predominantly fibrous tissue; on the other hand more radiopaque lesions contain greater proportion of woven bone [13,14]. Lesions of fibrouis dysplasia were diagnosed based on characteristic radiological findings showing bone scans and characteristic pathological findings on histopathology.
Sometimes bone lesions particularly in skull regions are not accessible to biopsy. So in those cases the diagnosis rests on classical radiological findings [14].
Conclusion
Fibrous dysplasia is an uncommon benign bone disease, although severe and devastating cases have been described. The main complications of FD are pathologic fracture, secondary aneurysmal bone cyst formation, and rarely malignant change. Oral physician should have proper knowledge and do all the investigations to diagnose such types of cases in initial stages to prevent any kind of complications which may occur later.
References
- Parekh SG, Rao DR, Ricchetti E, Lackman RD (2004) Fibrous dysplasia. J Am Acad Orthop Surg 12: 305-313.
- Sargin H, Gozu H, Bircan R, Sargin M, Avsar M, et al. (2006) A case of McCune-Albright syndrome associated with Gs alpha mutation in the bone tissue. Endocr J 53: 35-44.
- Feller L, Wood NH, Khammissa R, Lemmer J, Raubenheimer EJ (2009) The nature of fibrous dysplasia. Head Face Med 5: 22.
- Mahajan S, Kamboj M, Baoz K (2005) Maxillofacial fibrous dysplasia. Indian J Dent Res 16: 151-152.
- Lichtenstein L (1938) Polyostotic fibrous dysplasia. Arch Surg 36: 874-898.
- McCune D, Bruch H (1937) Osteodystrophia fibrosa: Report of a case in which the condition was combined with precocious puberty, multiple pigmentation of the skin and hyperthyroidism. Am J Dis Child 52: 745-748.
- Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, et al. (2005) Harrison’s Principles of Internal Medicine (16th edn.). McGraw-Hill, New York.
- Alam A, Chander BN (2003) Craniofacial fibrous dysplasia presenting with visual impairment. Med J Armed Forces India 59: 342-343.
- Yetiser S, Gonul E, Tosun F, Tasar M, Hidir Y (2006) Monostotic craniofacial fibrous dysplasia: The Turkish experience. J Craniofac Surg 17: 62-67.
- Lustig LR, Holliday MJ, McCarthy EF, Nager GT (2001) Fibrous dysplasia involving the skull base and temporal bone. Arch Otolaryngol Head Neck Surg. 127: 1239-1247.
- Panda NK, Parida PK, Sharma R, Jain A, Bapuraj JR (2007) A clinicoradiologic analysis of symptomatic craniofacial fibro-osseous lesions. Otolaryngol Head Neck Surg 136: 928-933.
- Grasso DL, Guerci VI, Di Emidio P, De Vescovi R, Ukmar M, et al. (2006) Dizziness as presenting symptom of monostotic fibrous dysplasia. Int J Pediatr Otorhinolaryngol Extra 1: 138-141.
- DiCaprio MR, Enneking WF (2005) Fibrous dysplasia. Pathophysiology, evaluation, and treatment. J Bone Joint Surg Am 87: 1848-1864.
- Fitzpatrick KA, Taljanovic MS, Speer DP, Graham AR, Jacobson JA, et al. (2004) Imaging findings of fibrous dysplasia with histopathologic and intraoperative correlation. ARJ Am J Roentgenol 182: 1389-1398.
Citation: Agarwal V (2018) Polyostotic Fibrous Dysplasia of Maxillofacial Region: A Case Report. J Interdiscipl Med Dent Sci 6: 224. DOI: 10.4172/2376-032X.1000224
Copyright: ©2018 Agarwal V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5061
- [From(publication date): 0-2018 - Mar 31, 2025]
- Breakdown by view type
- HTML page views: 4192
- PDF downloads: 869