Case Report Open Access
Pneumatosis Intestinalis in Patient with Relapsing Polychondritis
Si-Ho Kim, So Ree Kim, Jiyu Kim, Heejung Kim, Sung Won Park, Jinmyeong Oh and Hyemin Jeong*Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- *Corresponding Author:
- Hyemin Jeong
Division of Rheumatology, Department of Medicine
Samsung Medical Center, Sungkyunkwan University School of Medicine,
06351, 81 Irwon-ro, Gangnam-gu, Seoul, South Korea
Tel: 82234103439
Fax: 82234103849
E-mail: fly707@gmail.com
Received date: June 08, 2017; Accepted date: June 15, 2017; Published date: June 22, 2017
Citation: Kim SH, Kim SR, Kim J, Kim H, Park SW, et al. (2017) Pneumatosis Intestinalis in Patient with Relapsing Polychondritis. J Gastrointest Dig Syst 7:511. doi:10.4172/2161-069X.1000511
Copyright: © 2017 Kim SH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Relapsing polychondritis (RP) predominantly involves cartilaginous structures, but systemic vasculitis is also associated with RP. A 44-year-old man with RP visited the emergency department for incidentally detected free air in a chest X-ray. He was diagnosed with pneumotosis intestinalis (PI). PI is rare disease in which gas forms between the bowel walls. He was successfully treated with bowel rest and empirical antibiotics. This paper reports a case of PI in a RP patient.
Keywords
Polychondritis; Relapsing; Pneumatosis intestinalis; Glucocorticoids
Introduction
Relapsing polychondritis (RP) involves recurrently and progressively proteoglycan-rich organs and was first described in 1923 as "Polychondropathia" [1]. Yun et al. reported first RP case in Korea [2]. Meanwhile, pneumatosis intestinalis (PI) refers to the presence of gas within the submucosa or subserosa of the bowel well [3].
In 2007, a RP patient who presented PI was reported in Korea for the first time in the world [4]. We have then experienced a second PI case in a patient with RP. We suspected an association between RP, the episode of PI, and possibly steroid use as well. We examined the case of pneumatosis intestinalis in a 44-year-old male of RP patient.
Case Report
A 44-year-old man who has been treated for relapsing polychondritis (RP) for 2 years visited Samsung Medical Center emergency department (ED) with free air observed in a chest X-ray in December 2015. His RP presented with loss of sight in his left eye caused by severe scleritis and uveitis in December 2013. One month later, he developed swelling in both ears and was diagnosed with RP after a biopsy of ear cartilage. Having suffered from recurrent scleritis and uveitits, he took a moderate dose of steroid for a long time. At first, methotrexate was prescribed to spare steroids, but cyclophosphamide was prescribed as methotrexate could not be maintained due to liver enzyme elevation and flare-up of diseases. After six months use of cyclosphophamide, cyclosphophamide was switched to azathiopurine. The patient also presented with a history of diabetes mellitus.
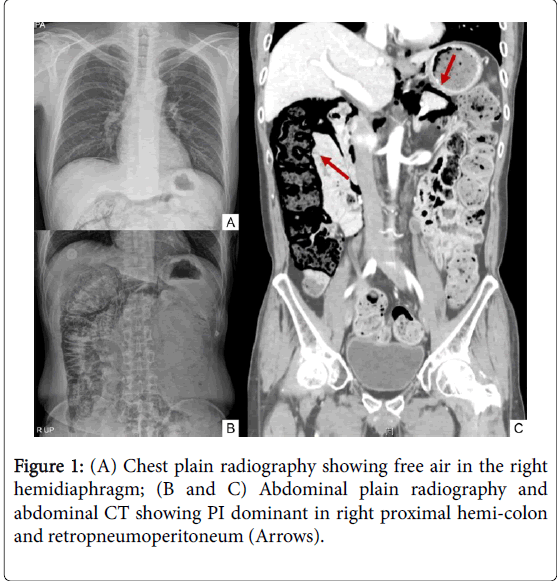
In October 2015, as his RP involved tracheal cartilage, he received a high-dose steroid treatment. Two months later, steroids were decreased to 20 mg, once daily. At that time, he was admitted to a local medical center to control high blood sugar levels. In a chest X-ray at admission, free air was observed in the right hemi-diaphragm (Figure 1A). He was then referred to our institute for proper management. In the ED, the patient`s blood pressure was 150/104 and his pulse rate was 104 beats/ minutes. His temperature was 36.9°C.
He had no gastrointestinal symptoms. Physical examination revealed tympanic sound on percussion without peritoneal irritation signs. In the abdominal X-ray, there was air in the retroperitoneal space (Figure 1B). Abdominal computed tomography (CT) revealed Pneumatosis coli involving cecum within the ascending and transverse colon accompanied by pneumo-retroperitoneum without evidence of colonic perforation (Figure 1C). We could not find any significant abnormalities in his blood test. Acute-phase reactants, such as Creactive protein (CRP) and erythrocyte sedimentation rate (ESR), were also normal (CRP 0.08 mg/dl, ESR 13 mm/hour). Through multidisciplinary discussion among rheumatologists, gastroenterologists and surgeons, physicians decided to apply empirical antibiotics and the patient was treated conservatively considering his stable vital signs and absence of signs of peritoneal irritation, even though pneumo-peritonum was observed. After two weeks of bowel rest and maintenance of intravenous fluid support, a follow-up CT showed decreased luminal air in the colon. He was discharged from the medical center with a tolerable soft diet, without any complication. Until now, he has taken azathioprine and low dose steroid, and there is no recurrence of PI.
Discussion
Several clinical conditions have been known to be associated with pneumatosis intestinalis (PI). According to its etiology, PI can be divided into idiopathic or secondary PI related to numerous gastrointestinal and non-gastrointestinal diseases [5]. Necrotizing enterocolitis in a premature neonate is the most representative cause of PI. Other intestinal disorders, such as intestinal ischemia, multiple endoscopic procedures, and inflammatory bowel disease have been observed causes of PI. Pulmonary disorders, including chronic obstructive pulmonary disease, asthma, and mechanical ventilation are also well-known causes of PI. Some medications and conditions disturbing patient’s immunity are also related to PI, such as connective tissue disorder, solid organ or bone marrow transplantation, steroid, chemotherapy and immunosuppressants [3,6,7].
In our case, long-term use of steroids was given to our patient to manage recurrent scleritis and uveitis. There is a hypothesis that steroids weaken intestinal wall by inducing the atrophy of lymph node in the intestine [4,7]. On the other hand, there is a suspicion that it is not the steroid alone, but rather underlying diseases that led to patients taking steroids were related to PI [3].
As said above, connective tissue diseases can be related to PI. Systemic sclerosis is the most common connective tissue disease accompanied by PI. There has been published cases of inflammatory myositis, multiple connective tissue disorder, polyarteritis nodosa, and systemic lupus erythematous with PI [3,8]. In RP, both specific T-cell clones responding to cartilage proteoglycans and circulating antibodies that denature type II and IV collagens are suspicious pathologic mechanisms of RP. RP with systemic vasculitis can be represented in 25 to 35% of the RP patients, involving cardiovascular, renal, skin and nerve vasculature [1]. We cannot give an explicit explanation as to why PI occurs in RP patients, however, considering many reported cases of PI with other connective tissue disorders, systemic vasculitis in RP might induce PI in those patients.
PI may be asymptomatic. However, it may be presented with symptoms of a life-threatening event [9]. Treatment of this unique condition depends on initial illnesses which cause PI. Even though free-air is seen in radiological image, if there is no apparent communication between bowel lumen and peritoneal space, such a case be considered as a benign condition. If a patient has signs of clinical collapse or forecasting signs of it, such as gas in the hepatic portal venous system, surgeons should decide operative management considering the high possibility of clinical deterioration [10].
Conclusion
We report the second case of PI in RP patient who was successfully treated with bowel rest and empirical antibiotics. Steroids are an important causative drug in PI, but we can also deduce RP itself might be involved in developing PI. When we meet RP patients with abdominal pain, especially those who are long-term steroid users, we should keep in mind the possibility of PI even though his or her symptoms may be mild.
References
- Sharma A, Gnanapandithan K, Sharma K, Sharma S (2013) Relapsing polychondritis: A review. ClinRheumatol 32: 1575-1583.
- Yun HJ, Yoo DH, Ahn KM, Park SS (1988) A case of relapsing polychondritis. Korean J Med 34:555-561.
- Heng Y, Schuffler MD, Haggitt RC, Rohrmann CA (1995) Pneumatosisintestinalis: A review. Am J Gastroenterol90:1747-1758.
- Kwok SK, Seo SH, Kim HS, Ju JH, Yoon CH, et al. (2007) Pneumatosiscystoidesintestinalis in relapsing polychondritis.ClinRheumatol26:1565-1567.
- Koss LG (1952) Abdominal gas cysts (pneumatosiscystoidesintestinorumhominis); An analysis with a report of a case and a critical review of the literature. AMA Arch Pathol53:523-549.
- Knechtle SJ, Davidoff AM, Rice RP (1990) Pneumatosisintestinalis. Surgical management and clinical outcome. Ann Surg212:160-165.
- Day DL, Ramsay NK, Letourneau JG (1988) Pneumatosisintestinalis after bone marrow transplantation. AJR Am J Roentgenol151:85-87.
- Dovrish Z, ArnsonY, Amital H, Zissin R (2009) Pneumatosisintestinalis presenting in autoimmune diseases: A report of three patients. Ann N Y AcadSci1173:199-202.
- Jamart J (1979) Pneumatosiscystoidesintestinalis. A statistical study of 919 cases. ActaHepatogastroenterol (Stuttg) 26:419-422.
- Itazaki Y, TsujimotoH, Ito N, Horiguchi H, Nomura S, et al. (2016) Pneumatosisintestinalis with obstructing intussusception: A case report and literature review. World journal of gastrointestinal surgery 8:173-178.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 3970
- [From(publication date):
June-2017 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 3175
- PDF downloads : 795