Short Communication Open Access
Pityriais Amiantacea: Brief Literature Review and Pratical Experience
Gustavo Moreira Amorim1,2*, Dâmia Leal Vendramini Amorim2, Eduardo Mastrangelo Marinho Falcão1,3 and Nurimar Conceição Fernandes11Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
2Institute of Dermatology Professor Rubem David Azulay, Rua Santa Luzia, Rio de Janeiro, Brazil
3Institute Oswaldo Cruz, Manguinhos, Rio de Janeiro, Brazil
- *Corresponding Author:
- Gustavo Moreira Amorim
Federal University of Rio de Janeiro
Rio de Janeiro, Brazil
Tel: +55 21 39382580
E-mail: gustavomoreiraamorim@hotmail.com
Received date: April 25, 2017; Accepted date: June 15, 2017; Published date: June 17, 2017
Citation: Amorim GM, Amorim DLV, Falcão EMM, Fernandes NC (2017) Pityriais Amiantacea: Brief Literature Review and Pratical Experience . Cosmetol & Oro Facial Surg 3:117.
Copyright: © 2017 Amorim GM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cosmetology & Oro Facial Surgery
Short Communication
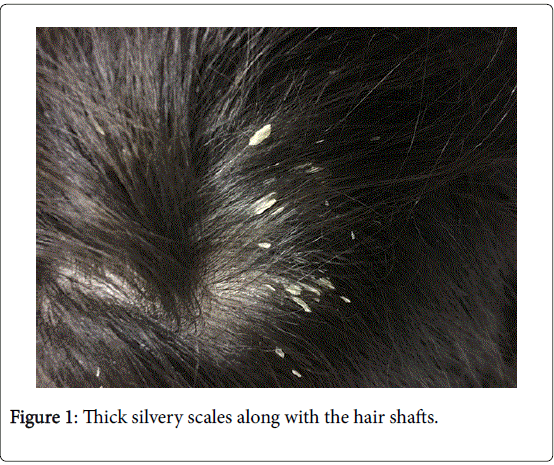
Pityriasis Amiantacea (PA) can be understood as an intense inflammatory reaction pattern that affects the scalp, secondary to different dermatoses that usually evolve this region [1]. Described by Alibert in 1832, it is characterized by the presence of thick silvery scales, strongly adhered to tufts of hair. The scales are arranged in an overlapping manner like flakes of asbestos, justifying its name amiantaceus [1,2]. Genetically predisposed patients, suffering from some kind of scalp dermatoses, when submitted to determine environmental factors like poor hygiene and secondary superficial infection can develop PA. Although primary trigger of this reaction pattern is still unknown, making the complete etiopathogenesis unclear [3].
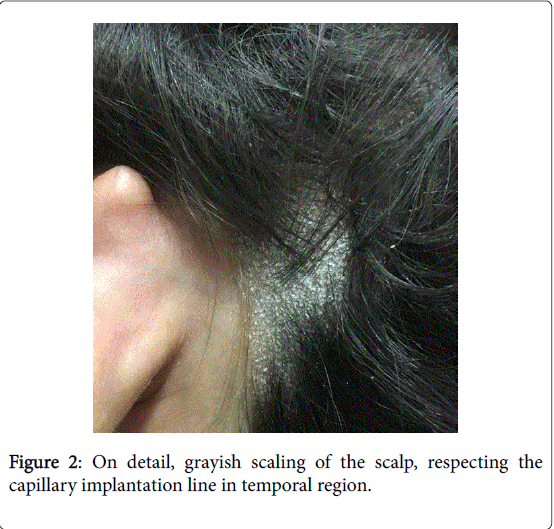
Epidemiologic data are scarce, being hard to determined incidence or prevalence. It can occur at any age, but it seems to be more common in children. A female predominance is reported also [3,4]. Seborrheic dermatitis, psoriasis and tinea capitis are the main underlying conditions, but atopic dermatitis Darier disease and even as an adverse effect of tumour necrosis fator-alpha inhibitor therapy were also reported [4-7]. Clinically the crusts are flattened, silver, firmly attached to the scalp, enveloping a tuft of several hairs. When removed, many hairs come out very easily along with the crust. The exposed skin surface is erythematous, sometimes with a purulent exudate. In general, a few plaques can be identified, most commonly on parietal region, although in severe cases the entire scalp can be evolved. Nonscarring alopecia usually follow the clinical findings but in rare cases, of long evolution and poor therapeutic response, scarring alopecia may occur [3,4]. Syndromic diagnosis of PA can be made on clinical bases, since clinical exam is very characteristic. Dermoscopy can be useful to complement clinical exam, since it magnifies the clinical features and demonstrates the correlation of the scales with the asbestos fibers [1,8]. The propaedeutic sequence is directed to the diagnosis of the underlying condition. Dermoscopy itself can be a great tool, since patterns to tinea; seborrheic dermatitis and psoriasis were already described [9]. It is imperative that the mycological examination of scales and hair shaft be performed, aiming to confirm or exclude tinea capitis. Some authors speculate that the overgrowth of staphylococcus aureus in the scalp could be part of PA pathogenesis. Positive cultures were found in the absolute majority of the cases studied by Abdhel- Hamid et al. So bacterial gram and culture tests can be done, complementing diagnosis and also guiding treatment, perhaps [4].
Histopathology is not a fundamental diagnostic criterion for PA, since it usually displays hyperkeratosis, parakeratosis, acanthosis, and some level of spongiosis. But it may help the etiological diagnosis [1]. Treatment can be challenging and sometimes disappointing. The options available include keratolytic agents, antiseborrheic shampoos and topical corticosteroids. Systemic corticosteroids can be a second line treatment for non-responders, as well as systemic antibiotic with staphylococcus-specific spectrum in cases of documented infection [1,3,4].
In our practice, specifically at our pediatric dermatology clinic, we reviewed in a previous published article 7 cases of PA. It was a retrospective cross-sectional study including charts of patients attended and followed in a period of 8 years. Inclusion criteria for PA were: silvery or yellowish scales encircling hair shafts; chronic course and negative direct mycological examination and culture from scale and/or hair samples. In those 7 cases, we observed a female predominance (5/7), with a mean age 9 years (standard deviation: SD: 2,8). Clinically, itching was present in all 7 patients and 1 patient evolved with cicatricial alopecia.
Seborrheic dermatitis was the underline cause in all 7 patients. Ketoconazole shampoo was the main therapy for the entire sample, always associated with a keratolytic agent (our preference was for 2% salicylic acid in mineral oil, applied 20 minutes before bath) and gentle mechanic removal of the crusts with a soft hairbrush. Two of the seven patients use topical corticosteroids along with the main therapy, but for shorter period comparing with ketoconazole. All 7 patients responded completely after a mean time of 6,4 months (SD: 2,6). But for that, good treatment adherence is fundamental and to accomplish that, extensive orientation of the patient and its family is needed (Figures 1 and 2) [10].
Since it was first described in 1832, little new information has been published about the epidemiology and pathophysiology of PA. With this letter approaching this subject, we seek to draw attention to the recognition of this condition.
References
- Fitzpatrick TB, Wolff K, Goldsmith LA, Katz SI, Gilcherest BA, et al. (2008) Dermatology in general medicine. 7th (ed). New York: Mcgraw-Hill Medical.
- Moon CM, Schissel DJ (1999) Pityriaisamiantácea. Cutis 63: 169-170.
- Gupta LK, Khare AK, Masatkar V, Mittal A (2014) Pityriasisamiantácea. Indian Dermatol Online J 5: S63-S64.
- Abdel-Hamid IA, Agha AS, Moustafa YM, El-Labban AM (2003) Pityriasisamiantacea: A clinical and etiopathologic study of 85 patients. Int J Dermatol 42: 260-264.
- Ginarte M, Pereiro Jr. M, Fernández-Redondo V, Toribio J (2000) Pityriasisamiantacea as manifestation of tinea capitis due to microsporumcanis. Mycosis 43: 93-96.
- Hussain W, Coulson IH, Salman WD (2009) Pityriasisamiantácea as the sole manifestation of darier´s disease. ClinExpDermatol 34: 554-556.
- Ettler J, Wetter DA, Pittelkow MR (2012) Pityriaisisamiantacea: A distinctive presentation of psoriasis associated with tumour necrosis fator-alpha inhibitor therapy. ClinExpDermatol 37: 639-641.
- Verardino GC, Macedo PM, Azulay-Abulafia L, Jeunon T (2012) Pityriasisamiantacea: Clinical-dermatoscopic features and microscopy of hais tufts. Na Bras Dermatol 87: 142-145.
- Lallas A, Kyrgidis A, Tzellos TG, Apalla Z, Karatolias A, et al. (2012) Accuracy of dermoscopic criteria for the diagnosis of psoriasis, dermatites, lichen planus and pityriaisrósea. Br J Dermatol 166: 1198-1205.
- Amorim GM, Fernandes NC (2016) Pityriaisamiantacea: A study of seven cases. An Bras Dermatol 91: 694-696.
Relevant Topics
- Blepharoplasty
- Bone Anchored Hearing Aids
- Chemical peel
- Cleft Surgery
- Congenital Craniofacial Malformations
- Cosmetic Facial Surgery
- Craniofacial Surgery
- Dental Orofacial Surgery
- Dentoalveolar Surgery
- Head and Neck Reconstruction
- Injectable Cosmetic Treatments
- Lip Reconstruction
- Mandibular Nerve Surgery
- Maxfax Surgery
- Maxillofacial Surgery
- Neck Liposuction
- Oral and Maxillofacial Surgery
- Oral Surgery Surgeon
- Orofacial Surgery Braces
- Pediatric Maxillofacial Surgery
- Rhytidectomy
- Sleep Apnea Orofacial Surgery
- Temporomandibular Joint Disorders
- Upper Jaw Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 3028
- [From(publication date):
June-2017 - Jul 18, 2025] - Breakdown by view type
- HTML page views : 2172
- PDF downloads : 856