Pilomyxoid Astrocytoma - An Unusual Catastrophic Presentation in a Toddler with Myriad Imaging Features Solving the Dilemma of Being Called as Pilocytic Astrocytoma
Received: 30-Apr-2020 / Accepted Date: 18-May-2020 / Published Date: 25-May-2020 DOI: 10.4172/2167-7964.1000319
Abstract
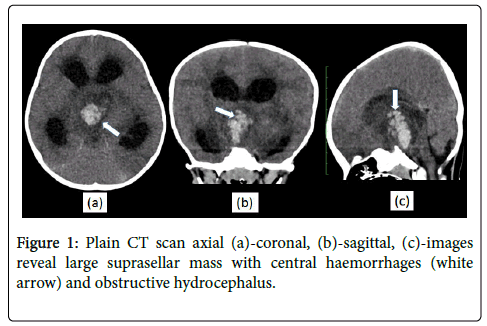
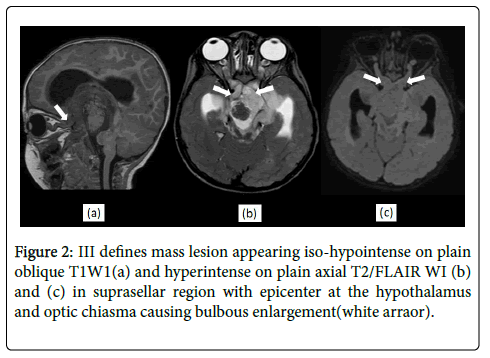
Pilomyxoid astrocytoma (PMA) is one of the rare primary CNS tumors of the pediatric age group which is a histological variant of pilocytic astrocytoma (PA) with poor prognosis. We present a case of 18 months old child presented with sudden onset of unconsciousness for a few hours. On computed tomography (CT) and magnetic resonance imaging (MRI) there was a large infiltrating mass with central haemorrhage seen in the suprasellar region with epicenter at hypothalamus-optic chiasma. There was one satellite nodule seen in the left anterior temporal lobe in a perisylvian location with leptomeningeal enhancement in left Sylvian fissure suggesting cerebrospinal fluid (CSF) dissemination. Based on these distinctive features, the presumed diagnosis was given as PMA also confirmed on histopathological examination after surgery. A palliative shunting to relieve hydrocephalous followed by debulking surgery was performed which is one of novel kind of treatment plans in such rare cases. In this way, few characteristic radiological features along with acute clinical presentation and combination treatment plan in toddler make our case of PMA unique which has not been reported in the literature yet.
Keywords: Pilomyxoid astrocytoma; Haemorrhage; Hypothalamusoptic chiasma; CSF dissemination
Abbreviations
PMA: Pilomyxoid Astrocytoma; CT: Computed Tomography; MRI: Magnetic Resonance Imaging; CSF: Cerebrospinal Fluid; WHO: World Health Organization
Introduction
Pilomyxoid astrocytoma is described as a rare WHO grade II tumor, accepted as a variant of pilocytic astrocytoma in the World Health Organization (WHO) classification of central nervous system tumors in 2007 [1] which is usually found at the hypothalamic- chiasmatic region [2].
Its clinical presentation can be a variable bearing myriad of symptoms like poor feeding, growth and mental retardation, seizures, nystagmus, weight loss however the sudden onset of unconsciousness in toddler probably due to haemorrhage was seen in our case making it different from previous literature.
PMA is an emerging entity and very few case reports and papers are available. So, its cases should be reported in the literature to understand its behavior which would help in treatment purposes.
Case Report
One and a half-year-old female child came with complaints of unconsciousness for six-seven hours. There was an episode of vomiting with reduced feed before unconsciousness. There was no other significant history. Developmentally the child was doing well. On admission, the patient was hemodynamically stable with poor Glasgow coma score. Systemic central nervous system examination revealed normal muscle tone while the deep tendon reflexes were not elicited. Pupils were unequally dilated. The pupillary reaction was sluggish bilaterally. Fundus examination showed disc pallor. The child was kept on oxygen. She was started on antibiotics and antivirals considering some infective etiology as the preliminary diagnosis. She had two episodes of seizures during the hospital stay.
Routine investigations including complete blood count, renal function test, liver function test, serum electrolytes and urine routine with microscopy were within normal limits. No Electrolyte imbalance was detected, and no growth was found on blood culture.
CSF examination findings were normal with no pus cells, no organism, No growth on Culture. GeneXpert of CSF and gastric lavage showed no mycobacterium tuberculosis bacilli.
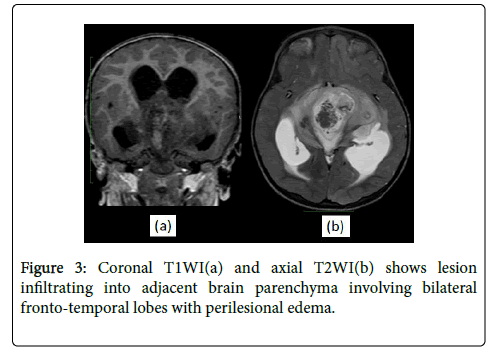
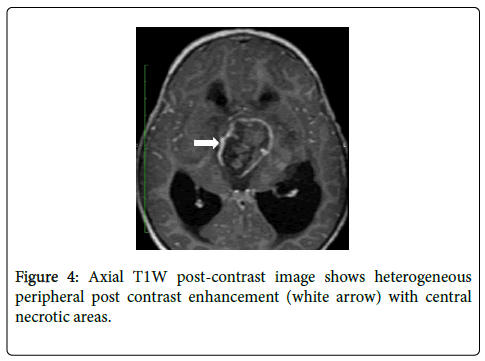
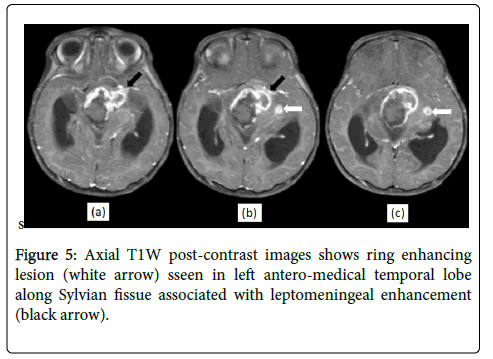
An emergency CT scan was performed on admission which revealed a large suprasellar infiltrating mass with central haemorrhages (Figure 1) and diagnosis of suprasellar craniopharyngioma was given. Later the patient was taken for an MRI brain scan for further evaluation of the mass. MRI scan of the brain with contrast was performed on Philips 1.5T. MRI revealed an ill-defined mass lesion appearing hyperintense on T2 and iso-hypointense on T1 WI in the suprasellar region with epicentre at the hypothalamus and optic chiasma causing bulbous enlargement of the same (Figure 2). It was infiltrating into the adjacent brain parenchyma involving bilateral frontotemporal lobes (Figure 3). Posteriorly it extended into the interpeduncular cistern which is widened. Moderate hydrocephalus was present secondary to compression of lateral ventricles were seen. Perilesional oedema was seen in bilateral frontal and temporal lobes extending into the gangliothalamic regions and midbrain and pons. Inferiorly the lesion was extending into the pre-pontine cistern. Both optic nerves were markedly tortuous. Blooming was seen on the GRE sequence within the lesion representing intertumoral hemorrhage. The lesion showed heterogeneous peripheral post-contrast enhancement with central necrotic areas (Figure 4). Another ring-enhancing lesion was seen in the left anteromedial temporal lobe along Sylvian fissure associated with leptomeningeal enhancement (Figure 5) suggesting CSF dissemination.
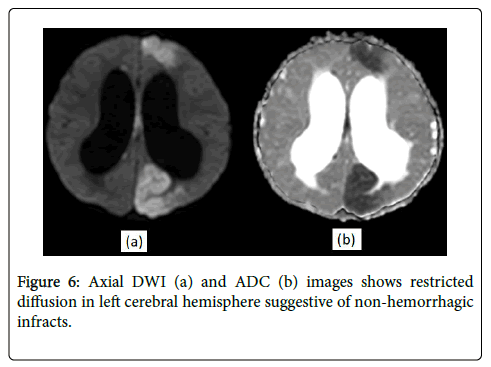
Non-haemorrhagic infarcts were seen in bilateral cerebral hemispheres secondary to mass effect/encasement of vessels (Figure 6).
CSF beta-human chorionic gonadotropin levels and alphafetoprotein levels were within normal limits ruling out craniopharyngioma. Considering imaging findings of an infiltrating aggressive neoplastic lesion with epicentre at the optic chiasm and hypothalamus along with intratumoral haemorrhage with CSF dissemination the diagnosis of PMA was given.
The patient was given palliative treatment in the form of VP shunting to relieve obstructive hydrocephalus. The post-procedural Glasgow coma scale score was improved.
After further stabilization, the patient was taken for surgical excision of the mass where partial debulking was done and the sample sent for histopathology.
On gross examination, the tumour was flimsy, mildly vascular, grayish coloured with areas of haemorrhages within. No clear plane could be identified between the tumour and normal brain parenchyma hence partial excision of the tumour was performed with a sample sent for histopathology. Histopathology report showed monotonous piloid cells with thin processes seen in a myxoid background. Focally perivascular arrangement of cells was noted. No definite eosinophilic granuloma bodies were seen. These findings were consistent with pilomyxoid astrocytoma (WHO grade II).
Discussion
Pilomyxoid astrocytoma is a primary CNS tumor that is known to be a histological variant of pilocytic astrocytoma. Most found before the age of four years, mean age being 18 months however it has been reported in adults in a few previous literatures.
Although PMAs may occur anywhere along the neuraxis, a most common location of the tumor is a hypothalamic-chiasmatic axis extending into the suprasellar cistern [3].
A glistening appearance caused by the myxoid component is common which is also the reason for its patchy heterogeneous enhancement along with non-enhancing areas representing necrosis [4].
Pilomyxoid astrocytoma differs from pilocytic astrocytoma both clinically and histo-pathologically with some differentiating features on imaging modality. Photomicrograph shows that the tumor is strongly positive for glial fibrillary acidic protein, confirming its astrocytic origin. Rosenthal fibers and the characteristic biphasic pattern of pilocytic astrocytoma are absent. Instead, PMA consist of monomorphic piloid tumor cells embedded in a striking, mucopolysaccharide-rich myxoid matrix. The neoplastic cells often display an angiocentric pattern that some investigators consider almost pathognomonic of PMA) [5]. Because of these histopathological respective imaging findings are found.
Compared with PAs, PMAs are more often solid with intratumoral haemorrhage and necrosis being more common. PMAs are known for a more aggressive infiltrating type of course with a high recurrence rate and poor prognosis. CSF dissemination is common with PMA, so the entire neuraxis should be imaged prior to surgical intervention.
Because of these features, it is very crucial identifying an astrocytoma as PMA for patient management and may justify more aggressive treatment. But the involvement of pilomyxoid astrocytoma in literature is very less and knowledge of its behavior is stunted. Its cases should be reported in the literature to understand its behavior which would help in treatment purposes.
In our case, there are multiple novel findings noted in both clinical and radiological behavior of the tumor. First, the age of our patient was just 18 months and presentation were acute onset of unconsciousness which has not been reported elsewhere as of now. Secondly, it was large infiltrating mass with massive intratumoral haemorrhage been noted associated with severe mass effect on vessels causing ischemia and ventricles causing obstructive hydrocephalus. Thirdly, most striking features were CSF dissemination along left Sylvian fissure with satellite nodule in left temporal lobe which is known for this tumor however rarely reported. Forth, our patient was managed both palliatives to relieve hydrocephalous followed by debulking surgery to relieve mass effects which turned out to be lifesaving in this case as the patient improved clinically after that.
Conclusion
PMA is one of a lesser-known entity in radiology due to lack of adequate literature however few peculiar imaging features like hypothalamus-chiasmatic location, CSF dissemination and intratumoral haemorrhages in younger age group help pointing towards the diagnosis. In our case child was managed by a combination of palliative treatment and surgery which also emerges as new advances in the therapeutic approach of these patients.
PMA remains a novel concept and its increased awareness by radiologists would help in differentiating it from the common pilocytic astrocytoma which would be a boon for the literature as well as for patients.
Declarations
Funding
NIL
Conflicts of interest/Competing interests
NONE
References
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, et al. (2007) The 2007 WHO classi cation of tumours of the central nervous system. Acta Neuropathol 114: 97-109.
- Tihan T, Fisher PG, Kepner JL, Godfraind C, McComb RD, et al. (1999) Pediatric astrocytomas with monomorphous pilomyxoid features and a less favorable outcome. J Neuropathol Exp Neurol 58: 1061-1068.
- Komotar RJ, Mocco J, Carson BS, Sughrue ME, Zacharia BE, et al. (2004) Pilomyxoid astrocytoma: A review. Med Gen Med 6: 42.
- Lee IH, Kim JH, Suh YL, Eo H, Shin HJ, et al. (2011) Imaging characteristics of pilomyxoid astrocytomas in comparison with pilocytic astrocytomas. Eur J Radiol 79: 311-316.
- Abdelzaher E (2020) Pilocytic astrocytoma - grade I. PathologyOutlines.com website.
Citation: Karuna A, Manali P, Nitesh P, Deepak P (2020) Pilomyxoid Astrocytoma - An Unusual Catastrophic Presentation in a Toddler with Myriad Imaging Features Solving the Dilemma of Being Called as Pilocytic Astrocytoma. OMICS J Radiol 9: 1000319. DOI: 10.4172/2167-7964.1000319
Copyright: © 2020 Karuna A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2821
- [From(publication date): 0-2020 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 1958
- PDF downloads: 863