Review Article Open Access
Physiotherapy of Operative of Myocardial Revascularization Post-Surgery
Debora Nunes Silva1, Fernanda de Paula Cordeiro1*, Lucas Sávio da Cruz Rodrigues1, Marina Fonseca Lelis1, Hermogenes de Carvalho Paiva Neto2 and Paulo Eduardo Santos Avila31Deapartment of physiotherapy, University of Amazonia, Brazil
2Department of Urban Development and Environment, University of Amazonia, Brazil
3Department of Biotechnology, Federal University of Para, Brazil
- *Corresponding Author:
- Fernanda de Paula Cordeiro
University of Amazonia Center for Biological and Health Sciences
Av Alcindo Cacela Belém, Pará 66060-000, Brazil
Tel: 091 992312102
E-mail: nandocacordeiro@hotmail.com
Received date: March 29, 2017; Accepted date: April 29, 2017; Published date: May 06, 2017
Citation: Silva DN, Cordeiro FP, Rodrigues LSC, Lelis MF, Neto HCP, et al. (2017) Physiotherapy of Operative of Myocardial Revascularization Post-Surgery. J Nov Physiother 7:349. doi: 10.4172/2165-7025.1000349
Copyright: © 2017 Silva DN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Abstract
Introduction: Myocardial infarction (MI) is defined by total interruption of coronary flow, resulting in ischemia and myocardial necrosis. In MI, diastolic function of the left ventricle is immediately altered, since part of the diastole is an energy-dependent procedure.
Objective: To analyze, through a systematized review, the effect of physical therapy treatment in the postoperative period of myocardial revascularization.
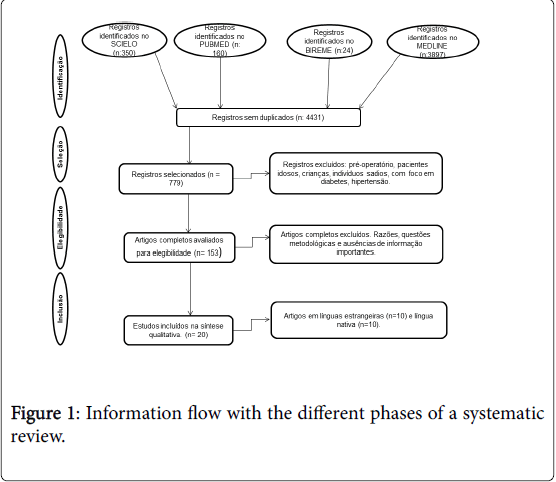
Methodology: The tool used to analyze the selected articles was the list of PRISMA recommendations. We analyzed original researches published in English and Portuguese in the last ten years, using the SCIELO, PUBMED, BIREME, MEDLINE databases.
Results: 100 articles were selected, with inclusion and exclusion criteria, being chosen only 20 articles, 10 of Portuguese language and 10 of foreign language.
Conclusion: Cardiac rehabilitation protocols, involving the association of conventional physiotherapy with stimulators and other techniques, such as PEEP, TENS, CPAP, muscle training, deep breathing exercises, provide a satisfactory and immediate result to individuals.
Keywords
Myocardial revascularization; Post-surgery care; Physical therapy; Respiratory exercises
Introduction
Cardiovascular diseases are the main causes of death in developed countries, and their occurrence has increased epidemically in developing countries. In a research involving 115,021 cardiac surgeries (CC), they found an overall mortality rate of 8%, most of them occurring in the PO period, with pulmonary complications being one of the most prevalent causes [1].
Myocardial infarction (MI) is defined by total interruption of coronary flow, resulting in ischemia and myocardial necrosis. In MI, diastolic function of the left ventricle is immediately altered, since part of the diastole is an energy-dependent procedure. It is probable that patients with a higher degree of diastolic dysfunction show a decrease in functional capacity proportionally to their severity [2].
The relationship of heart disease and its influence on the respiratory system shows that cardiac compromise and the surgical process cause pulmonary complications [3]. Patients who undergo CABG often develop pulmonary dysfunctions, such as atelectasis, restrictive ventilatory disorder, and hypoxemia [4].
Cardiorespiratory physiotherapy works to minimize these complications generated by cardiac surgery [3]. Gaining space acting precociously in both the preoperative and postoperative periods, using pulmonary re expansion techniques, bronchial hygiene techniques, and flow and volume augmentation techniques [4].
The objective of this article was to analyze, through a systematized review, the effect of physical therapy treatment in the postoperative period of myocardial revascularization with focus on respiratory improvement, better gas exchange and a better quality of life.
Methodology
The tool used to analyze the selected articles was the list of PRISMA recommendations, the purpose to help authors improve the reporting of systematic reviews and Meta-analyzes. We analyzed original researches published in English and Portuguese in the last ten years, with reference to databases SCIELO, PUBMED, BIREME, and MEDLINE. In order to select studies with greater scientific evidence, we only consider controlled clinical trials. The search strategy considered the following keywords; Myocardial Revascularization, Post-operative Care, Physical Therapy, Respiratory Exercises.
The search strategy used was broad and resulted in 4431 titles speaking about myocardial revascularization. Of these, 779 selected were excluded by the title because they did not present the inclusion criteria. We included research on physiotherapy in myocardial revascularization. And we excluded the work that was not related to revascularization. Of the 153 remaining studies, they were discarded for methodological reasons and lack of important information. Thus, 20 studies were included for qualitative synthesis, in which they presented all the inclusion criteria, with relevant and extremely important information for the research. Thus, 10 articles were of Portuguese language and 10 of foreign language (Figure 1).
Discussion
Patients undergoing coronary artery bypass graft surgery may be predisposed to acquire complications in the cardiovascular and respiratory systems, as a consequence of secondary dysfunctions such as induction of anesthesia, thus triggering ventilation and perfusion disorders promoting a closure of the airways [4].
The experiences of heart disease and surgery change the way you live, work, and understand the process that is happening to each patient. According to the interviews, people who went through the health-disease process report that they manipulate the knowledge, standards, values and beliefs that guide their practices [5].
It was observed that one of the common alterations in this procedure is atelectasis, since they are diagnosed through radiological exams and are linked to aggravation of gas exchange and decrease of pulmonary volumes, resulting in restriction of functional capacity and pulmonary complacency [4].
In order to promote a balance and improvement in the clinical picture of each individual, physiotherapeutic intervention was used in cardiac rehabilitation programs involving a multidisciplinary team that meets the needs required [6].
Post-operative physiotherapy aims to treat the pulmonary complications, performed through physiotherapeutic maneuvers and non-invasive respiratory device, aiming to improve respiratory mechanics, pulmonary expansion and bronchial hygiene [7].
According to Araujo [8], cardiac rehabilitation reduces mortality rates, myocardial revascularization and improves the quality of life, biochemical profile, and increase in physical fitness, evolution in functional capacity and gain in hemodynamic, physiological and autonomic parameters.
Cardiac rehabilitation programs in post-myocardial revascularization patients include muscle training, transcutaneous electrical nerve stimulation - TENS, effects of PEEP, the role of electro analgesia in respiratory function, the use of EPAP by face mask, CPAP, deep breathing exercises and spirometry. Treatment varies with a frequency of two to three times a day, with a series of ten repetitions of breathing exercises.
According to Matheus [5] respiratory muscle training was effective in recovering tidal volume and vital capacity in the threshold training group, which was done in 47 patients and was divided into two groups: the study group with 23 patients and the control group with 24 Patients, for Ferreira [9] the results are similar with the use of the threshold, but there was no difference in PEmax and PImax in the postoperative period, only improvement was observed in the preoperative period.
In the Barros study [10] performed with 38 patients with respiratory muscle training treatment, it was observed that there were alterations in Pimax, PEmax, VC and PEF in subjects submitted to immediate postoperative surgery and it was verified that in the group submitted to revascularization without To perform the muscular training showed a different behavior, already those submitted to the muscular training was noticed that a reestablishment of the ventilation functionality occurred at the moment of the hospital discharge, returning its parameters to the values initially observed, before the surgery.
In a study of 149 patients, the physical exercise performed in the cardiovascular physical therapy protocol was effective, promoting changes in heart rate, without causing any clinical complications [11].
A survey conducted by Aikawa [12], with 86 patients, developed a protocol with combination of aerobic exercises and resistance exercises. The weight of the dumbbells and ankles were determined according to the profile of each patient. The improvement of the functional capacity was the main result that the research obtained.
In the protocol that Botega [13] elaborated, with 14 patients, consisted of a group of low-impact exercises for upper and lower extremity and walking exercise, performed in the pre- and postoperative period. Heart rate, systolic blood pressure, diastolic blood pressure, mean arterial pressure, double product, and EPI score were assessed before and after training. The result was satisfactory, but lower than expected, with only an increase in heart rate in the individual analysis.
In the treatment with EENT (Transcutaneous Electric Nerve Stimulation), it was effective in the management of postoperative pain in cardiac surgery, avoiding the excessive use of analgesic as well as in the improvement of respiratory muscle strength and especially in PEmax [14]. Considering the results of the studies analyzed, we observed the efficacy of certain procedures used in the postoperative period, since pain control becomes essential for the patient, since the pain stimuli pre-dispose to a greater suffering of the postoperative complications.
For Luchesa, [15] although electro analgesia helped in the pain effect, it did not react in the improvement of peak expiratory flow, forced vital capacity and forced expiratory volume in the first second of patients undergoing cardiac.
According to Graetz [16], the respiratory complications present in the postoperative period of cardiac surgery are frequent, with emphasis on atelectasis, pneumonias, hypoxemia and pleural effusions. However, it was verified that the use of PEEP promoted a lower incidence of atelectasis and lower reductions in some Spiro metric values in patients submitted to myocardial revascularization when compared to nonperforming respiratory physiotherapy.
In the Sena [17] study performed with Twenty-eight patients, the effect of PEEP with the use of non-invasive mechanical ventilation was observed, which proved to be efficient, since it significantly reduces the need for reintubation and the need for tracheostomy in patients with respiratory failure, Oxygenation and reducing respiratory work.
Among the protocols performed in the articles is the deep breathing exercise compared to spirometry. According to Renault [4] the research was performed with 36 patients, but no significant differences were observed in maximal respiratory pressures, spirometric variables and oxygen saturation among patients submitted to deep breathing exercises and incentive spirometry in the postoperative period of myocardial revascularization surgery.
For Renault 1, deep breathing exercise techniques (BET) are easy techniques, however, incentive spirometry has not been shown to be more effective than respiratory physiotherapy alone, in reducing pulmonary complications, in hospital stay and in pulmonary function. ERPs consist of slow and uniform nasal breathing aimed at increasing pulmonary expansion, increasing diaphragmatic demand and improving recovery of function.
According to Mendes [18], the research carried out on the use of CPAP in 16 patients after cardiac surgery concluded that there were
In Mendes's research [19], the treatment with RPPI and physiotherapeutic intervention was performed in 21 patients, where 8 performed the exercise with RPPI and 13 with intervention. When comparing the two interventions, it was concluded that there was no superiority between the applied techniques. important changes in lung function, strength, and thoraco abdominal mobility. However, there was no difference in the results comparing the CPAP/RPPI with the physiotherapeutic intervention.
Positive airway expiratory pressure by face mask (EPAP) is used in the postoperative period of cardiac surgeries, however, its hemodynamic effects have not been clearly studied. According to Sena [16], in the study carried out with EPAP by Facial Mask in Cardiac Post-operative Hemodynamics, 31 patients were selected, who tolerated EPAP well and resulted in an increase in right and left ventricular filling pressure measurements, as well as in blood pressure average.
As for Cavalli [20], since the prevalence of cardiac surgeries is high and entails high costs due to secondary complications, he hears the need to describe a new underwater EPAP device in which 17 individuals were evaluated, where they obtained results indicating that underwater EPAP improves saturation Of oxygen, helps in the removal of secretions through collateral ventilation and expectoration, improves pulmonary auscultation, reduces the main complaint by the progressive increase of the thoracic mobility, making.
In a study of 39 patients divided into two groups, where the first group performed one physical therapy session per day and the second group performed three physiotherapy sessions during the hospital recovery, it was found that multiple physical therapy sessions per day Offers patients better psychosocial conditions and less morbidity [21].
It can be concluded that cardiac rehabilitation protocols, involving the association of conventional physiotherapy with stimulants and other techniques, such as PEEP, TENS, CPAP, EPAP, muscle training, deep breathing exercises, provide a satisfactory and immediate result to individuals.
References
- Renault JA, Val RC, Rossetti MB (2008) Respiratory physiotherapy in pulmonary dysfunction after cardiac surgery. Rev Bras Cir Cardiovasc
- Diniz LS, Gomes DAP, Neves VR, Silva MG, Nunes MCP, et al. (2013) Relation between functional capacity and diastolic function in the recent infarction. Fisioter. Pesqui.
- Morsch KT, Lequisamo CP, Camargo MD, Coronel CC, Mattos W, et al. (2009) Ventilatory profile of patients undergoning CABG sugery. Rev Bras Cir Cardiovasc 24: 180-187.
- Renault JA, Val RC, Rossetti MB, Neto MH (2009) Comparison between deep breathing exercises and incentive spirometry after CABG surgery. Rev Bras Cir Cardiovasc 24: 165-172.
- Cavalcante ES, Magario R, Conforti CA, Cipriano Junior G, Arena R, et al. (2014) Impact of Intensive Physiotherapy on Cognitive Function after Coronary Artery Bypass Graft Surgery. Rev Arq Bras Cardiol 103:391-397.
- Matheus GB, Dragosavac D, Trevisan P, Costa CE, Lopes MM, et al. (2012) Inspiratory muscle training improves tidal volume and vital capacity after CABG surgery. Rev Bras Cir Cardiovasc27:362-369.
- Cavenaghi S, Ferreira LL, Marino LHC, Lamari NM (2011) Respiratory physiotherapy in the pre and postoperative period of myocardial revascularization surgery. Rev Bras Cir Cardiovasc 26: 455-461.
- Benetti M, Araujo CLP, Santos RZ (2010) Cardiorespiratory Fitness and Post-Infarction Quality of Life in Different Exercise Intensities. Brazilian Society of Cardiology.
- Ferreira PE, Rodrigues AJ, Evora PR (2009) Effects Of An Inspiratory Muscle Rehabilitation Program In The Postoperative Period Of Cardiac Surgery.ArqBras Cardiol 92: 275-282.
- Barros GF, Santos CS, Granado FB, Costa PT, Limaco RP, et al. (2010) Respiratory muscle training in myocardial revascularization. Rev Bras Cir Cardiovasc 25: 483-490.
- Hiss MDBS, Neves VR, Hiss FC, Silva E, Borghi A, et al. (2012) Safety of Early Physical Therapy Intervention after Acute Myocardial Infarction Fisioter. Mov25:153-163.
- Aikawa P (2014) Cardiac Rehabilitation in Patients Undergoing Myocardial Revascularization Surgery. Rev Bras Med Sport 20: 1.
- Botega FS (2010) Cardiovascular behavior during rehabilitation after coronary artery bypass grafting. Rev Bras Cir Cardiovasc 25: 4.
- Lima PM, Farias RT, Carvalho AC, da Silva PN, Filho NAF, et al. (2011) Transcutaneous electrical nerve stimulation after coronary artery bypass graft surgery. Rev Bras Cir Cardiovasc26: 591-596.
- Luchesa CA, Greca FH, Guarita-Souza LC, Santos JLV, Aquim E (2009) The role of electroanalgesia in patients undergoing coronary artery by-pass surgery. Rev Bras Cir Cardiovasc24:391-396.
- Graetz JP, Moreno MA (2015) The effectiveness of positive end-expiratory pressure after coronary artery bypass grafting. Fisioterpesqui 22: 1.
- Sena ACBS, Ribeiro SP, Condessa RL, Vieira SRR (2010) Positive Airway Pressure by Face Mask in Cardiac Post-operative Hemodynamics. Rev Bras Cir Cardiovasc 95: 5.
- Mendes RG, Cunha FV, Pires Di Lorenzo VA, Catai AM, Borghi-Silva AA (2005) Influence of physiotherapeutic intervention techniques and continuous positive airway pressure (cpap) in the postoperative period of cardiac surgery. Brazilian Journal of Physical Therapy 9: 297-303.
- Mendes RG, Borgbi-Silva A (2006) Efficacy of the physiotherapeutic intervention associated or not to intermittent positive pressure breathing (rppi) after cardiac surgery with extracorporeal circulation. Rev Physiotherapy in Motion 19: 73-82.
- Cavalli F, Nohama P (2013) New underwater EPAP device in the postoperative period of myocardial revascularization surgery. Rev FisioterMov 26:37-45.
- Vila VSC, Rossi LA, Costa MCS (2008) Heart disease experience of adults undergoing coronary artery bypass grafting surgery. Rev SaúdePública42: 4.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 2875
- [From(publication date):
June-2017 - Mar 31, 2025] - Breakdown by view type
- HTML page views : 2054
- PDF downloads : 821