Review Article Open Access
Physiotherapy and Head and Neck Cancers
Vipin Goel*, Hemant Nemade, KVVN Raju and CS RaoDepartment of General Surgery, Bidar Institute of Medical Science, Bidar, Karnataka, India
- Corresponding Author:
- Dr. Vipin Goel
Department of General Surgery
Bidar Institute of Medical Science
Bidar, Karnataka, India
Tel: 919844115040
E-mail: vipinrgoel@gmail.com
Received Date: January 09, 2017; Accepted Date: February 15, 2017; Published Date: February 22, 2017
Citation: Goel V, Nemade H, Raju KVVN, Rao CS (2017) Physiotherapy and Head and Neck Cancers. J Nov Physiother 7:337. doi: 10.4172/2165-7025.1000337
Copyright: © 2017 Goel V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Novel Physiotherapies
Review on Head and Neck Cancers
Among all Cancers, head and neck cancers constitute the majority of cases in developing country like India. Over 200,000 cases of head and neck cancer occur each year in India [1]. Head and neck cancers include oral cancers, pharyngeal cancers, laryngeal cancers, salivary gland cancers, cancers involving the skin of head and neck region, etc. Treatment for head and neck cancer involves surgery, radiotherapy and chemotherapy. Surgery involves excision of tumor from a primary site with margin, including dissection of the cervical lymph nodes in most of cases, with or without removal of the sternocleidomastoid muscle, jugular vein and spinal accessory nerve depending on disease burden. Defect created by surgery often requires immediate reconstruction using local, regional or free flaps.
Surgery followed by reconstruction has many acute and chronic complications [2]. With radiotherapy added during treatment either upfront or post operatively adds to morbidities already patient is at risk. Acute complications are wound infections, chyle leak, flap necrosis, donor site morbidity and medical morbidities, such as cardiac problems, deep vein thrombosis, etc. Chronic complications include shoulder pain/dysfunction, neck stiffness, edema, trismus, etc. Loss of motor innervation to the sternocleidomastoid and Trapezius, results in loss of mobility and strength of the shoulder leading into reduced cervical range of motion [3]. Skin complications include cervical contracture, pain, thickening and edema of tissue (lymphedema). Other complications include, restricted mouth opening and ankylosis of the temporomandibular joint. The sequela of the disease and the treatment interferes with the patient’s quality of life.
Physiotherapy plays major role in rehabilitation of head and neck cancer survivors [4]. It prevents and/or treats multiple complications arisen because of treatment. Physiotherapy helps cancer survivors in restoring them physically, emotionally and socially.
Complications and physiotherapy management
Shoulder pain and weakness [5,6]: Neck dissection is associated with various shoulder dysfuctions such as shoulder droop, scapular dyskinesia, trapezius atrophy, loss of shoulder abduction and shoulder and neck pain which was first described by Ewing and Martin [7].
• Prevention of frozen shoulder through the active and assisted range of motion (ROM).
• Strengthening of scapular elevators and retractors.
• Neuromuscular retraining of shoulder girdle muscles.
• Preservation of Trapezius muscle tone through electrical stimulation.
• Providing shoulder support allowing recovery of the Levator scapulae.
• Use of orthosis giving support to shoulder.
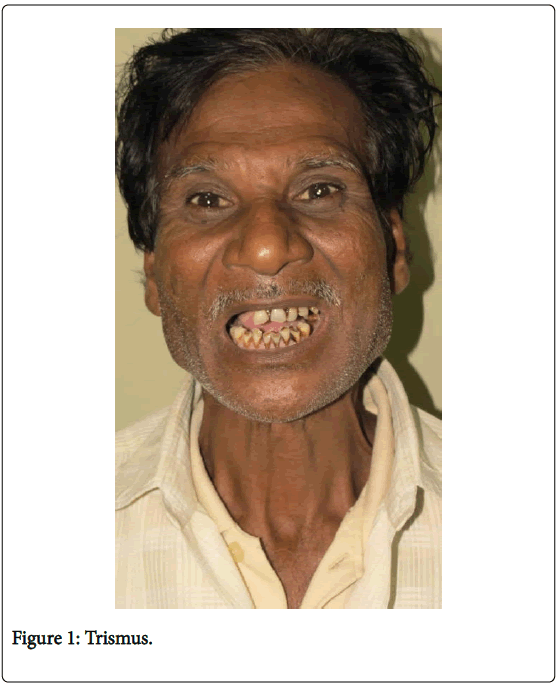
Trismus/temporomandibular joint dysfunction (Figure 1) [8,9]:
• Mouth-opening exercises (oro-motor exercises).
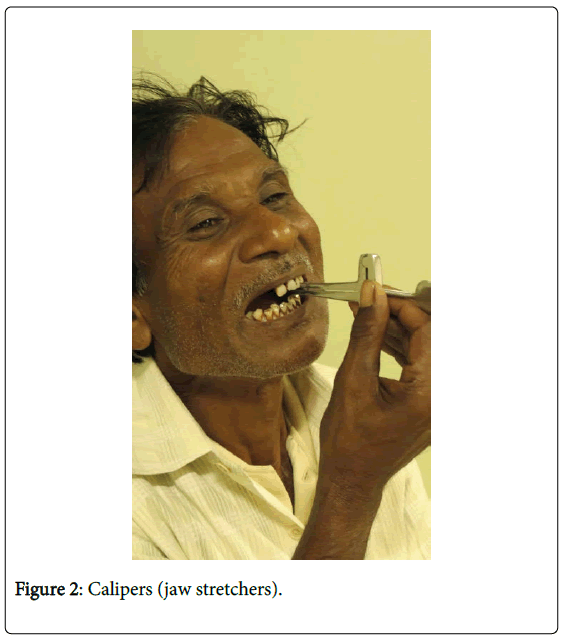
• Use of jaw stretchers by increasing mouth opening (Figure 2).
• Diet modification, incorporating more semi-solid food.
• Use of moist heat to relax muscles.
• Dynamic splinting
• Avoiding excessive heat or cold to skin.
• Sequential manual lymphatic drainage.
• Use of compression garments.
• Avoiding smoking as tobacco intervenes in wound healing.
• Nutritional advice keeping in mind positive protein balance.
Swallowing difficulty [12,13]:
• Diet modification and motivation.
• Weight recording and close watch on weight loss.
• Maintaining tongue strength and mobility.
• Laryngeal muscles exercises.
• Mendelson's maneuver (holding the larynx in its most supine position during swallowing, for 2-3 sec during each swallow).
Respiratory complications and Deep vein thrombosis:
Oral cancer ablative surgery mostly involves excision of the muscles and mucosa required for the swallowing. The resultant handicap produces risk of aspiration and respiratory complications. Since most of these patients are smokers and with compromised respiratory function, it is important to initiate chest physiotherapy and ambulation early in post-operative period.
Pain [14]:
• Use of oral and parental analgesics.
• Exercises, active or passive mobilization techniques.
• Postural and positioning education.
• Heat or cold massage therapy.
• TENS (Transcutaneous Electrical Nerve Stimulation).
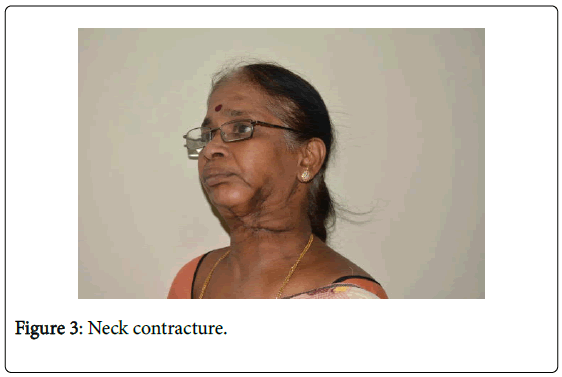
Cervical contracture (Figure 3) [15]:
• Active and active-assisted ROM in all planes of neck motion.
• Additional stretch during end-range by exerting pressure with the contralateral hand.
• Postural modifications with help of visual aids.
• Self-massage to augment the efficacy of ROM activities.
• Compression garments: helping by applying compression.
Conclusion
Once cancer patient is cured by primary treatment modality most patients experience some physical impairment resulting in a physical disability [16]. This aspect of treatment is most neglected among all treating physicians, especially in third world countries.
It’s our responsibility to ensure that all cancer patients regain maximum function, making them to return to all former duties. The exact functional deficits should be identified and proper rehabilitation should be started immediately. Preventive aspects of rehabilitation should be taught to the patient long before the patient develops symptoms. Multidisciplinary rehabilitation should be made an integral part of the total management of the head and neck cancer.
References
- Cancela MDC, Voti L, Guerra-Yi M, Chapuis F, Mazuir M, et al. (2010) Oral cavity cancer in developed and in developing countries: Population based incidence. Head Neck32: 357-367.
- Wilgen CPV, Dijkstra PU, Laan BFVD, Plukker JT, Roodenburg JL (2004) Morbidity of the neck after head and neck cancer therapy. Head Neck26: 785-791.
- Cappiello J, Piazza C, Nicolai P (2007) The spinal accessory nerve in head and neck surgery. Curr Opin Otolaryngol Head Neck Surg 15:107-111.
- Rashleigh L (1996) Physiotherapy in palliative oncology. Aust J Physiother 42:307-312.
- Lauchlan DT, Mccaul JA, Mccarron T, Patil S, Mcmanners J, et al. (2011) An exploratory trial of preventative rehabilitation on shoulder disability and quality of life in patients following neck dissection surgery. Eur J Cancer Care 20: 113-122.
- Akgun K, Aktas I, Uluc K (2008) Conservative treatment for late-diagnosed spinal accessory nerve injury. Am J Phys Med Rehabil87:1015-1021.
- Ewing MR, Martin H (1952) Disability following radical neck dissection; an assessment based on the postoperative evaluation of 100 patients. Cancer5:873-883.
- Dijkstra PU, Sterken MW, Pater R, Spijkervet FK, Roodenburg JL (2007) Exercise therapy for trismus in head and neck cancer. Oral Oncol43:389-394.
- Shulman DH, Shipman B, Willis FB (2008)"Treating trismus with dynamic splinting: A cohort, case series". Adv Ther 25: 9-16.
- Linnitt N, Davies R (2007) Fundamentals of compression in the management of lymphedema. Br J Nurs 16:588.
- Piso DU, Eckardt A, Liebermann A, Gutenbrunner C, Schafer P, et al. (2001) Early rehabilitation of head-neck edema after curative surgery for orofacial tumors. Am J Phys Med Rehabil 80:261-269.
- Mittal BB, Pauloski BR, Haraf DJ, Pelzer HJ, Argiris A, et al. (2003) Swallowing dysfunction-preventative and rehabilitation strategies in patients with head-and-neck cancers treated with surgery, radiotherapy, and chemotherapy: a critical review. Int J Radiat Oncol Biol Phys 57:1219-1230.
- Carroll WR, Locher JL, Canon CL, Bohannon IA, McColloch NL, et al. (2008) Pretreatment swallowing exercises improve swallow function after chemoradiation. Laryngoscope118:39-43.
- Breivik H, Cherny N, Collett B, de Conno F, Filbet M, et al. (2009) Cancer-related pain: A pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol 20:1420-1433.
- Glastonbury CM, Parker EE, Hoang JK (2010) The postradiation neck: Evaluating response to treatment and recognizing complications. AJR Am J Roentgenol 195:w164-171.
- Cheng A, Schmidt BL (2008) Management of the N0 neck in oral squamous cell carcinoma. Oral Maxillofac Surg Clin North Am20:477-497.
Relevant Topics
- Electrical stimulation
- High Intensity Exercise
- Muscle Movements
- Musculoskeletal Physical Therapy
- Musculoskeletal Physiotherapy
- Neurophysiotherapy
- Neuroplasticity
- Neuropsychiatric drugs
- Physical Activity
- Physical Fitness
- Physical Medicine
- Physical Therapy
- Precision Rehabilitation
- Scapular Mobilization
- Sleep Disorders
- Sports and Physical Activity
- Sports Physical Therapy
Recommended Journals
Article Tools
Article Usage
- Total views: 5718
- [From(publication date):
April-2017 - Jul 19, 2025] - Breakdown by view type
- HTML page views : 4733
- PDF downloads : 985