Research Article Open Access
Physician Attitudes on the Provision of Palliative Care in Puerto Rican Emergency Departments
Melissa Rosado Rivera* and Fernando Soto Torres
Department of Emergency Medicine, University of Puerto Rico, San Juan, Puerto Rico, USA
- *Corresponding Author:
- Melissa Rosado Rivera
Department of Emergency Medicine
University of Puerto Rico, San Juan
Puerto Rico, USA
Tel: 787-485-1133
Fax: 787-750-0930
E-mail: melirosa_26@yahoo.com
Received date: Octomber 24, 2014, Accepted date: December 9, 2014, Published date: December 17, 2014
Citation: Rivera MR, Torres FS (2015) Physician Attitudes on the Provision of Palliative Care in Puerto Rican Emergency Departments. J Palliat Care Med 5:201. doi:10.4172/2165-7386.1000201
Copyright: © 2015 Rivera RM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: Although many institutions in the United States have incorporated palliative care practices in their emergency departments, very little has occurred in Puerto Rico. Information regarding palliative care training of emergency medicine physicians in Puerto Rico is unclear and most physicians have poor or no access to palliative care services for their patients. This study explores the perceptions and barriers encountered by practicing emergency physicians in providing palliative care in Puerto Rican Emergency Departments.
Methods: A survey was administered to physicians attending the American College of Emergency Physicians Puerto Rico Chapter annual Convention. Attending physicians and residents from the University of Puerto Rico School of Medicine validated the survey tool via a “content validity” approach. Participants were asked to respond to Likert scaled statements with options that ranged from “Strongly Agree” to “Strongly Disagree”. The statements addressed physician comfort level with provision of palliative care and discussion of end of life issues, as well as barriers encountered by providers such as time constraints, fear of lawsuits, and lack of access to specialists among others.
Results: Of the 85 physicians at the convention 59 provided surveys available for review for a response rate of 70%. Of those surveyed, 35% reported feeling some level of discomfort at providing palliative care in the ED and 39.6% agreed or strongly agreed that their lack of training in palliative care affects their ability to provide this service. In addition, 81% lack access to palliative care specialists/ teams in the emergency department. However, 82.8% agreed or strongly agreed that palliative care is an important competence for emergency physicians.
Conclusions: Despite recognizing palliative care as an important competence, emergency physicians in Puerto Rico reported insufficiencies in training, decreased level of comfort, and lack of access to specialists in palliative care. Efforts to enhance physician training and provide palliative care resources must be pursued in order to improve the quality of care given to patients visiting Puerto Rican Emergency departments.
Keywords
Palliative care; PuertoRico; Physician training; Emergency medicine; Palliative medicine; End of life; Physician comfort
Introduction
Palliative care is defined by the Center to Advance Palliative Care as “specialized medical care for people with serious illness. It is focused on providing… relief of symptoms, pain, and stress from serious illness” with the “goal of improving the quality of life of both the patient and the family” [1]. Palliative medicine achieves improvement of quality of life and relief of pain by establishing efficient communication of the patient’s goals and by integrating conventional treatments with aggressive management of symptoms [2]. Patient and family satisfaction has been shown to increase with early palliative care interventions and can also reduce hospital stay and total costs [2].
Emergency medicine was incepted as a specialty because of a need to care for patients seeking immediate and emergent medical attention. Therefore, traditionally, emergency physicians are trained in management of acute conditions with the goal of live saving. As a result, management of death and end-of-life issues has a lower priority over treatment strategies that preserve life. Palliation of patient symptoms has not been a focus of ER physician training. It was not until recently that the demand for palliative care in the ER became an issue. Because our older patient population has acutely risen, palliative medicine was recognized as a subspecialty of emergency medicine in 2006 [3]. In Puerto Rico, 14.5% of the population was 65 years of age or older in 2010 [4]. If we compare these findings to the previous census we observe an increase of a little more than 3% over ten years. This is significant to emergency physicians because this represents increased ER visits by older patients. These patients are more likely to suffer from chronic and debilitative medical conditions that make them ideal candidates for palliative care.
Because patients suffering from serious illness and their families can experience stressful and overwhelming moments during the disease process, including sudden respiratory distress, severe pain, vomiting, and confusion among others, the first point of access is often the ER. The emergency staff evaluating these patients has the opportunity to identify and intervene early. Unfortunately, most patients die in the hospital setting despite their wish to die at home [5]. Centers where palliative specialists are available provide the opportunity or patients to establish their preferences for care. Patient can work the palliative team to coordinate the aggressiveness of treatment, symptom management and place of death. In a study by Paris and Morrison, palliative care consultation was associated with increased hospice use, decreased hospital death and increased death at home [6].
Despite the acceptance of the importance of palliative care in the emergency setting, its definitive role continues to develop [7]. The integration of palliative care in emergency medicine has not been without its challenges. Emergency physicians often focus their attention on the patients dying in an acute and unexpected or “spectacular” death and neglect the patients dying the “subtacular” end of life deaths [8]. Emergency physician training has traditionally focused on life saving interventions and not the palliation of patient symptoms [9].
In addition to this fixed view of the role of the emergency physician, limited knowledge of palliative care, physician attitudes and perspectives of palliative care, time constraints, difficult environment and ineffective communication with patients, families and providers have been identified as barriers to the provision of palliative care in the emergency department [7,9]. Working in the emergency department can be stressful. The constant flow of patients, crowding, limited resources and poor interpersonal relationships has been found to create significant stress in the emergency nurses [10]. Physician stress has also been associated with patient suffering. Physicians dealing with the stress of the dying patient in an attempt to separate themselves from the situation and can become uncompassionate and neglectful of the patient’s needs [11].
Although many institutions in the United States have incorporated palliative care practices in their emergency departments, very little has occurred in Puerto Rico. Currently there is only one hospital that has a Palliative Care Unit: Veteran's Administration. Emergency physicians in Puerto Rico have little or no training in palliative care and poor access to palliative care services for their patients. There is also no information regarding emergency physicians’ perceptions and perceived barriers to palliative care in emergency departments in Puerto Rico. This study attempts to discover the current physician perceptions and perceived barriers encountered in emergency departments in Puerto Rico. Understanding physician perceptions and barriers to palliative care in Puerto Rico will enable future interventions to overcome these barriers and improve physician and staff training.
Methods
We administered a survey to physicians attending the American College of Emergency Physicians Puerto Rico Chapter Annual Convention The survey was created using items described in a previous survey by Meo, et al. and Schroeder, et al. [12]. Three attending physicians and four residents from the University of Puerto Rico School of Medicine who did not participate in the final survey validated the survey tool via a “content validity” approach [13].
At inscription, each participant was approached by one of the authors or an assistant to fill in the short survey. Participants were assured a priori that there were no coding elements or identity markers on the survey instrument and all answers would remain anonymous, confidential, and only to be used in aggregate. Survey respondents were assured that only the primary investigators would review the data and participation was voluntary.
Demographic data collected included age, gender, and educational information. Professional data included years of experience, number of potential palliative interventions per week, and academic versus private practice. Participants were asked to respond to Likert-scaled statements on the topic of palliative care. The Likert scale used was the following: Strongly Disagree=1, Disagree=2, Neutral=3, Agree=4, Strongly Agree=5. Palliative care was defined as “an approach that improves the quality of life of patients and their families facing life-threatening illness, through the prevention and relief of suffering by impeccable assessment and treatment of pain and physical, psychosocial and spiritual issues.” The statements addressed physician comfort level with provision of palliative care and discussion of end of life issues, as well as barriers encountered such as time constraints, fear of lawsuits, and lack of access to specialists among others.
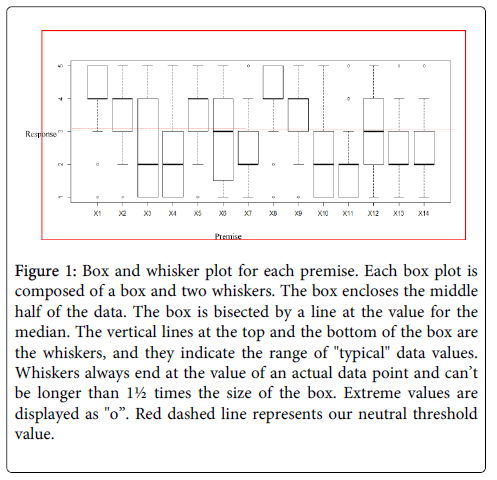
Statistical analysis was performed using R 3.0.1. Mean and standard deviations were calculated. Box and whisker plots were obtained for each of the premises in order to determine distribution and range of responses. We also performed an ANOVA to compare physician comfort level in regards to years of experience. A copy of the survey is provided in Appendix A. The Institutional Review Board for the University of Puerto Rico School of Medicine approved this study.
Results
Of the 85 physicians present in the American College of Emergency Physicians Puerto Rico Chapter Convention, 59 participated in the survey for an overall response rate of 70%. Participant’s ages ranged from 27-74 years with a mean age of 43.8 ± 12 years. Of the 59 surveyed, 54.2% identified themselves as male. Of those who responded, 76.4% identified themselves as catholic while the other 24.4% where mainly protestant and 6.8% of all surveyed did not respond. In addition, 74.6% identified themselves as emergency medicine physicians, 10.2% as emergency residents while the other 15.3% where general practitioners or other subspecialties such as pediatricians or family practitioners. Demographic information is presented in Table 1.
| Gender | ||
|---|---|---|
| Female | Male | |
| 27 | 32 | |
| Age (mean) | 39.26 | 47.38 |
| Medical Specialty | ||
| ER Residents | 6 | |
| Emergency Physician | 44 | |
| Other | 9 | |
| Religion | ||
| Atheist | 2 | |
| Catholic | 42 | |
| Protestant | 7 | |
| None | 5 | |
Table 1: Demographic Information.
Mean responses and standard deviations are presented in Table 2. A box and whisker plot demonstrating distribution of responses for each premise is presented in Figure 1.
| Premise* | Mean | Standard Deviation |
|---|---|---|
| 1 | 4.12 | ±0.95 |
| 2 | 3.54 | ±1.04 |
| 3 | 2.69 | ±1.50 |
| 4 | 2.27 | ±1.22 |
| 5 | 3.66 | ±1.04 |
| 6 | 2.69 | ±1.34 |
| 7 | 2.47 | ±1.12 |
| 8 | 4.1 | ±1.01 |
| 9 | 3.58 | ±1.18 |
| 10 | 2.17 | ±1.07 |
| 11 | 2.02 | ±0.94 |
| 12 | 2.92 | ±1.26 |
| 13 | 2.59 | ±1.10 |
| 14 | 2.42 | ±1.05 |
Table 2: Mean response values for the Likert scaled survey. 1Palliative care is an important competence for an emergency medicine physician; 2I have a clear idea of the role of palliative care in the emergency department; 3Emergency medicine physicians are trained to save lives and not to manage death; 4My workplace has protocols or services addressing end of life and palliative care issues; 5 I feel comfortable providing palliative care in the emergency department; 6 Palliative care should be the responsibility of the patients primary care physician and not the emergency physician; 7Palliative care should have a lower priority in the busy emergency department; 8There is lack of access to palliative care specialists/ teams in the emergency department; 9 Having no access to communication with the primary care physician affects my ability to provide palliative care in the emergency department; 10I have difficulty discussing end of life issues with patients and/or their families; 11I cannot identify patients who may need palliative care in the emergency department; 12 My lack of training in palliative care affects my ability to provide this service; 13 Fear of lawsuits leads me away from offering palliative alternatives to potential candidates; 14I have sufficient time during my shift to provide palliative care in the emergency department. Likert scale used: Strongly Disagree=1, Disagree=2, Neutral=3, Agree=4, Strongly Agree=5
Figure 1: Box and whisker plot for each premise. Each box plot is composed of a box and two whiskers. The box encloses the middle half of the data. The box is bisected by a line at the value for the median. The vertical lines at the top and the bottom of the box are the whiskers, and they indicate the range of "typical" data values. Whiskers always end at the value of an actual data point and can’t be longer than 1½ times the size of the box. Extreme values are displayed as "o”. Red dashed line represents our neutral threshold value.
The role of palliative care was evaluated with the survey statements [1-3,6,7]. Of those surveyed, 82.8% (mean 4.12 ± 0.95) acknowledged palliative care as an important competence and 60% (mean 3.54 ± 1.04) reported having a clear understanding of its role in the ED. In addition, 36% (mean 2.69 ± 1.50) of those surveyed reported that ER physicians are trained to save lives and not manage death and 32% (mean 2.69 ± 1.34) feel that palliative care is the responsibility of the primary care physician and not the emergency physician. Over 60% (mean 2.47 ± 1.12) of the participants surveyed reported disagreeing or strongly disagreeing that palliative care should have a low priority in the busy ED.
The barriers to providing palliative care were evaluated with the survey statements [4,8,9,11-14]. Over 60% (mean 2.27 ± 1.22) reported no access to palliative care services or established protocols. Nearly 40% (mean 2.92 ± 1.96) agreed or strongly agreed that their lack of training in palliative care affects their ability to provide this service. In addition, 81% (mean 4.1 ± 1.01) lack access to palliative care specialists or teams in the emergency department and 63% (mean 3.58 ± 1.15) identify primary care physician inaccessibility as a barrier to provision of palliative care. Time was also reported as a barrier by 63% (2.42 ± 1.05) of participants. Only, 18% (mean 2.59 ± 1.10) reported fear of lawsuits as a barrier. Finally, less than 10% (mean 2.02 ± 0.94) reported difficulty with identifying potential palliative care candidates.
The comfort level with palliative care was evaluated with the survey statements 5 and 10. Of those surveyed, 35% (mean 3.66 ± 1.54) reported feeling some level of discomfort at providing palliative care in the ED and 14% (mean 2.17 ± 1.07) experience difficulty when discussing end of life issues. We performed an ANOVA to assess participant’s comfort level in relation to their years of experience. We observed that there is a statistically significant difference (p<0.001) in comfort level when compared with years of experience. Those with more years of experience report increased level of comfort when providing palliative care.
Discussion
The emergency physician has the unique opportunity to identify and intervene with patients who qualify for palliative care in a way that can significantly alter the service they receive. But, in order to adequately do so, ED physicians must be properly trained and have access to the necessary resources. Physicians surveyed reported numerous barriers when providing palliative care in the ED. Barriers identified include poor access to the primary care physician, time constraints and lack of training. Similar to results found by Grudzen et al. the physicians in our study reported that working in the busy ED creates time constraints that force them to rank palliative care as a lower priority 9. Unfortunately, even though physicians may want to dedicate time to these patients they are often too occupied to do so.
In addition, despite easily recognizing candidate patients in the ED, most physicians reported lack of palliative care teams/specialists and/or protocols. This is alarming because although possible candidate patients are identified, physicians are unable to treat them effectively due to a lack of resources.
Furthermore, almost 40% of those surveyed admit that their lack of training in palliative care is a barrier to the care these patients receive. These results identify a need for further training in a significant proportion of physicians working in Puerto Rican ED’s. Limited training in palliative care is not only a barrier in Puerto Rico but has been identified as a barrier elsewhere. In a study involving HIV specialists and oncologists treating HIV patients, Peretti-Watel et al. discovered a need to provide training in palliative care as HIV patients were being undertreated for pain due to misconceptions with morphine use and timing of initiation of palliative care measures [14]. Smith et al. also report that residents felt their training with pain management in the ED was deficient and requested increased training on the topic [3]. These results are also similar to results by Meo et al. where residents interviewed identify low levels of formal training in palliative care and request further training [7].
Mierendorf and Gidvani describe the skills physicians need to care for these patient in the ED. Physicians must know how to identify patients requiring palliative care, be emotional sympathetic to the needs of the patient and their families, know how to manage patient symptoms effectively, recognize and actively treat the dying patient, involve palliative specialists and obtain spiritual support when needed [15]. Physician training needs to address each of these areas in order to provide quality care for palliative patients visiting emergency departments.
The majority of those surveyed (82.8%) acknowledge palliative care as an important competence. They also recognize their responsibility in providing palliative care. Although not emergency physicians, in a study performed by Vejlgaard et al., physicians in Denmark also reported accepting the importance of palliative medicine for patient care and the active role the physician plays in assuring and providing this treatment [16]. Given the team approach to patient care physicians across a broad variety of specialties understand that they are all responsible for knowing the skills needed for palliative care and emergency doctors in Puerto Rico are not the exception.
Despite the majority of physicians surveyed recognizing their role in palliative medicine and its importance for patient care, approximately 33% believe that palliative care is the responsibility of the primary care physician. This finding is not unique to Puerto Rican ED’s. In a study performed by Grudzen et al, when interviewed some emergency physicians report that discussing end of life care and patient goals should be the responsibility of the patient’s primary care physician [9]. These results are contrary to Vejlgaard’s findings where 10% reported they would rather leave the responsibility of palliative care to someone else [16]. Our findings suggest that one third of the physicians working in Puerto Rican ED’s are less likely to perform palliative medicine because they don’t recognize providing palliative care as their obligation. Thulesius et al. discovered that education of staff significantly improved attitudes toward end of life care and we believe initiatives to educate physicians working in Puerto Rican ED’s will help change these attitudes and contribute to improvements in patient care [17].
The majority of participants surveyed identified themselves as Catholic. Religious affiliation and culture have been found to affect physician decisions. In a study in European ICU’s, significant differences were reported for the type of end of life decisions, times to therapy limitation and death and discussion of decisions with patient families depending on the physicians religious affiliation of culture [18]. Although we cannot draw any definite conclusions from this study, it does force us to questions if physician’s religious affiliation and culture could be another barrier to patient care. Further studies must be undertaken to clarify these findings.
Even though most reported feeling comfortable providing palliative services in the ED, over one third report discomfort when treating these patients. Grudzen et al. report that physicians discomfort with managing these patients is a barrier and recommend education in palliative medicine as a means to improve patient treatment [9]. We found that comfort was associated with years of experience. Those surveyed with more years of experience responded feeling comfortable providing palliative care more often than those with less years of experience. If we take into account that 40% report deficiencies in training, these findings suggest that comfort level is currently being established by experiences via trial and error and not as a result of adequate training and education. Unfortunately, this study does not allow an assessment of whether or not those who report comfort providing palliative care are actually proficient when performing the task. Just because they believe they are effective when treating these patients does not mean that they actually are.
Our findings are significant because they provide the first look into the perceptions and experiences of physicians working in emergency departments in Puerto Rico with palliative care. These results identify the issues that need to be addressed in Puerto Rican ED’s and can serve to guide interventions to improve physician training, resource allocation and public policy changes.
Limitations
The results of this study may be limited as the participants represent a small sample of physicians working in Puerto Rican ED’s. These results may not necessarily reflect all physicians working in Puerto Rican ED’s attitudes or perceptions of palliative care and may not be generalized to areas outside of Puerto Rico. This study also overwhelmingly involved participants who recognized themselves as emergency medicine physicians and only a small percent of general practitioners. As there is a large number of general practitioners working in Puerto Rican ED’s we feel there could be a selection bias as the survey was administered at the ACEP Puerto Rico chapter’s annual emergency medicine convention where emergency physicians are more likely to be present. In addition, the survey tool used a Likert scale that limits the possible responses and participants were not provided with the opportunity to write in other options. Additional barriers or attitudes may not have been identified due to the limited nature of the survey tool. Participant’s level of training and knowledge of palliative care was not formally assessed and results relied on self-reports. Responders self –reports on comfort or proficiency with palliative care does not necessarily translate to effectiveness when providing this care.
Conclusion
Need for Emergency physician training and education on the topic of palliative care continues to escalate as our elderly population continues to grow. With each passing day, Puerto Rican ED’s receive more and more patients who are candidates for palliative care and it is our responsibility to assure them these services. Physician’s working in Puerto Rican ED’s, recognize the importance of palliative care but unfortunately lack training, protocols, and palliative care teams/specialists. Future interventions to improve physician training and promote the establishment of palliative care services must be undertaken.
References
- Hall KL, Rafalson L, Mariano K, Michalek A (2014) Evaluation of Hospital-Based Palliative Care Programs. Am J HospPalliat Care .
- Beemath A, Zalenski RJ (2009) Palliative emergency medicine: resuscitating comfort care? Ann Emerg Med 54: 103-105.
- Smith AK, Fisher J, Schonberg MA, Pallin DJ, Block SD, et al. (2009) Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann Emerg Med 54: 86-93, 93.
- U.S. Census Bureau. (2010) Puerto Rico Commonwealth characteristics
- Pritchard RS, Fisher ES, Teno JM, Sharp SM, Reding DJ, et al. (1998) Influence of patient preferences and local health system characteristics on the place of death. SUPPORT Investigators. Study to understand prognoses and preferences for risks and outcomes of treatment. Journal of the American Geriatric Society 46: 1242-1250.
- Paris J, Morrison RS (2014) Evaluating the effects of inpatient palliative care consultations on subsequent hospice use and place of death in patients with advanced GI cancers. J OncolPract 10: 174-177.
- Meo N, Hwang U, Morrison RS (2011) Resident perceptions of palliative care training in the emergency department. J Palliat Med 14: 548-555.
- Bailey C, Murphy R, Porock D (2011) Trajectories of end-of-life care in the emergency department. Ann Emerg Med 57: 362-369.
- Grudzen CR, Richardson LD, Hopper SS, Ortiz JM, Whang C, et al. (2012) Does palliative care have a future in the emergency department? Discussions with attending emergency physicians. J Pain Symptom Manage 43: 1-9.
- Oliveira JD, Achieri JC, Pessoa Júnior JM, de Miranda FA, Almeida Md (2013) [Nurses' social representations of work-related stress in an emergency room]. Rev Esc Enferm USP 47: 984-989.
- Whitehead PR (2014) The lived experience of physicians dealing with patient death. BMJ Support Palliat Care 4: 271-276.
- Schroder C, Heyland D, Jiang X, Rocker G, Dodek P; Canadian Researchers at the End of Life Network (2009) Educating medical residents in end-of-life care: insights from a multicenter survey. J Palliat Med 12: 459-470.
- Panacek EA (2008) Survey-based research: general principles. Air Med J 27: 14-16.
- Peretti-Watel P, Bendiane MK, Galinier A, Lapiana JM, Favre R, et al. (2004) Opinions toward pain management and palliative care: comparison between HIV specialists and oncologists. AIDS Care 16: 619-627.
- Mierendorf SM, Gidvani V (2014) Palliative care in the emergency department. Perm J 18: 77-85.
- Vejlgaard T, Addington-Hall JM (2005) Attitudes of Danish doctors and nurses to palliative and terminal care. Palliat Med 19: 119-127.
- Thulesius H, Petersson C, Petersson K, Håkansson A (2002) Learner-centred education in end-of-life care improved well being in home care staff: a prospective controlled study. Palliat Med 16: 347-354.
- Sprung CL, Maia P, Bulow HH, Ricou B, Armaganidis A, et al. (2007) The importance of religious affiliation and culture on end-of-life decisions in European intensive care units. Intensive Care Med 33: 1732-1739.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13935
- [From(publication date):
January-2015 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 9402
- PDF downloads : 4533