Physician Assisted Suicide for Terminally Ill Patients: An Argumentative Essay
Received: 28-May-2018 / Accepted Date: 14-Jun-2018 / Published Date: 21-Jun-2018 DOI: 10.4172/2165-7386.1000337
Abstract
Dying process is too often needlessly protracted by these medical technology is consequently marked by incapacitations, intolerable pain, and indignity. Physician assisted suicide defines as knowingly and intentionally providing a person with the knowledge or means or both required to commit suicide, including counseling about lethal doses of drugs, prescribing such lethal doses or supplying the drugs. Therefore, the aim of this paper is to create an argumentative essay to argue the use of physician assisted suicide for terminally ill patients as a last resort to end their suffer and end their life, while taking the legal and ethical points of view of opponents and proponents into consideration.
Keywords: Palliative care; End of life care; Medical Care; Suicide
Introduction
The recent advance of the life -saving interventions and mechanical devices, that result from the medical technology has prolong dying process, which raise need to end of life care [1]. Dying process is too often needlessly protracted by these medical technology is consequently marked by incapacitations, intolerable pain, and indignity [2]. Terminally ill patient commonly experience unremitted and intolerable pain despite optimal pain management [3]. In these situations, physician assisted suicide is sometime applied, which is controversial legally and ethically issue [4]. Physician assisted suicide used interchangeably with physician assisted death and assisted suicide, is suicide undertaken with the aid of another person, sometime a physician (American Heritage Dictionary Entry). Which means knowingly and intentionally providing a terminally ill patient with the knowledge or means or both required to commit suicide, which also usually include counseling about lethal doses of certain drugs either by prescribing, supplying such lethal drugs or both [5]. Among countries that permit physician assisted suicide, person who has been diagnosed as terminally ill and who physically suffer from unresolved symptoms with life expectancy of 6 months or less can request from the physician to prescribe and/ or supply a lethal dose to self-administered to end his/her life [6].
The main causes to request physician assisted suicide among terminally ill patients according to cohort study conducted in Switzerland, were 56.7% cancer, nervous system causes 20.6%, and mood disorder (mental or behavioral disorder) 2.8%, among terminally ill patient who aged (25-64 years), compared with terminally ill patients who aged (65-94 years) cancer 40.8%, circulatory 15.2%, and nervous system causes 11.3% [7]. The Hippocratic Oath includes the unambiguous statement “I will not give a lethal drug to anyone if I am asked, nor will I advise such a plan” [8]. An argumentative assay is a writing method, challenging communication task that calls upon sophisticated cognitive and linguistic abilities, where the writer takes a position and tries to convince the reader to perform an action or to adopt a point of view regarding a controversial issue [9]. Therefore, the aim of this paper is to create an argumentative essay to argue the use of physician assisted suicide for terminally ill patients as a last resort to end their suffer and end their life, while taking the legal and ethical points of view of opponents and proponents into consideration.
Physician assisted suicide defines as “knowingly and intentionally providing a person with the knowledge or means or both required to commit suicide, including counseling about lethal doses of drugs, prescribing such lethal doses or supplying the drugs” [10]. Physician assisted suicide is considered the most controversial end of life practice according to its ethical acceptability and the desirability of legalization [11]. Netherlands’s physicians have applied physician assisted suicide since 1977, then it has done legally since 1992 [12]. Also, Oregon legalized physician assisted suicide in 1997 [13]. According to Oregon’s Death with Dignity Act, the patient who request physician assisted suicide should be; an adult with 18 years old or more, capable to make and communicate the health decision, diagnosed with terminal illness that will lead to death within six months, and an Oregon resident [14]. The purpose of this literature review is to discuss the opponent’s and proponent’s points of view related to physician assisted suicide, from the legal and ethical sides.
Legal Arguments
Opponents
Physician assisted suicide is illegal in china under Article 232 “whoever intentionally commits homicide shall be sentenced to death, life imprisonment or fixed term imprisonment of not less than 10 years; if the circumstances are relatively minor, he shall be sentenced to fixed-term imprisonment of not less than 3 years but not more than 10 years”, and Article 233 “whoever negligently causes death to another person shall be sentenced to fixed-term imprisonment of not less than 3 years but not more than 7 years; if the circumstances are relatively minor, he shall be sentenced to fixed-term imprisonment of not more than 3 years, except as otherwise specifically provided in this Law” of the Criminal Law of People’s Republic of China [15].
In Turkey, physician assisted suicide is illegal under Article 84 any person who commits, helps, supports, or encourages a person for suicide is punched with imprisonment from 2-5 years [16]. In United Kingdom, assisted suicide is also illegal under Suicide Act 1961 [17]. In Jordan, physician assisted suicide is not of the physician duties according to article number 3 “it is not permissible to terminate the life of a patient who is suffering from incurable and insurmountable disease and whether accompanied by pain, either directly or indirectly, except brain death, according to the scientific conditions approved by the Medical Association” [18].
Proponents
Physician assisted suicide has been legalized in Switzerland since 1942 and is accessible for noncitizens, and according to swizz law assisting suicide is punishable just if done for “whoever, from selfish motives, induces another to commit suicide or assists him therein shall be punished, if the suicide was successful or attempted, by confinement in a penitentiary for not more than five years or by imprisonment” article 115 of the penal code of Switzerland [19]. In 1994 voters in Oregon approved the Death with Dignity Act, which allowing a physician to prescribe a lethal dose that self-administers voluntarily by the terminally ill patient, the patient and the physician who follow the requirements of the act are protected from criminal prosecution [20].
In 2008, Washington Death with Dignity Act passed with the same to Oregon law [21]. Also in 2013, Vermont Patient Choice and Control at the End of Life Act has been in effect [22,23]. In 2016, California’s physician assisted dying law took effect according to the End of Life Option Act [24]. Also, in Finland, is not a crime and connected to end of life care [24].
Ethical Arguments
Opponents
The ethical principles of beneficence (working to achieve the patient’s best interest), nonmaleficence (avoidance of harm), patient autonomy respect, as well as promotion of justice and fairness (American College of Physicians Ethics, Professionalism, and Human Rights Committee, 2013). Both of the profession and ethical traditions emphasize care and comfort, and physician shouldn’t intentionally participate in ending a person’s life [25].
Proponents
Some patients may get benefit from physician assisted suicide, and for dying patients, the motivation for requesting physician assisted suicide may not be physical pointless suffering but loss of autonomy (97.2%), in ability to engage in enjoyable activities (88.9%), loss of dignity (75%) [26]. Dying process could be beneficial in order to spiritual and existential healing through relational and personal wholeness growth, also individual learning process for the patients, their families, and those who caring for them [27].
Argumentative Statement
Physician assisted suicide is inconsistent with some of ethical principles such as nonmaleficence. Similarly, in laws of many countries physician assisted suicide is illegal. Therefore, the author refutes the use of physician assisted suicide for terminally ill patients in order to end their suffering and end their life, and use palliative care instead it.
Legal Defense
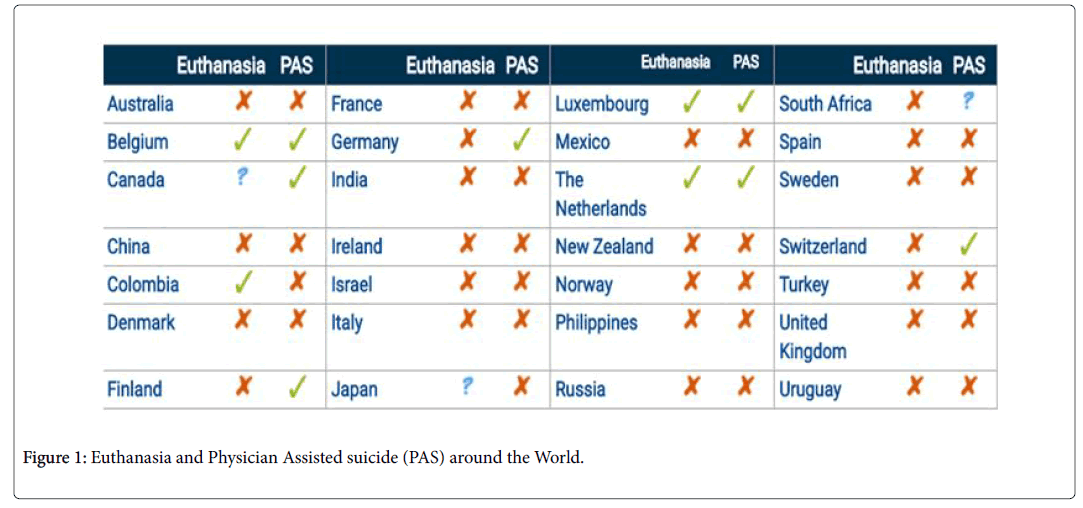
According to the position of the American Medical Association physician assisted suicide is fundamentally inconsistent with the physician's professional role, their position consistent to the medical constitution and duties of the physician and profession in Jordan. Physician assisted suicide for terminally ill patients is illegal in many countries (Figure 1). In Oregon, the incidence of physician assisted suicide has been increased from 0.6 in 1000 deaths to 3 in 1000 deaths in 1998 and 2014 respectively [28].
Ethical Defense
In the last revised of The International Code of Medical Ethics in the section which under the name of duties of physicians to patients states that "A physician shall always bear in mind the obligation to respect human life" [29]. Also, patient autonomy must be respect from physician but also must be balanced with other ethical principles [30]. From the religious perspectives, physician assisted suicide is morally wrong as it showed clearly in the Holy Quran in Surah 5-ayah 32 (AlMaeda) “That was why We wrote for the Children of Israel that whoever killed a soul, except for a soul slain, or for sedition in the earth, it should be considered as though he had killed all mankind; and that whoever saved it should be regarded as though he had saved all mankind. Our Messengers brought those proofs, then many of them thereafter commit excesses in the earth by the Catechism of the Catholic Church, "God is the creator and author of all life."
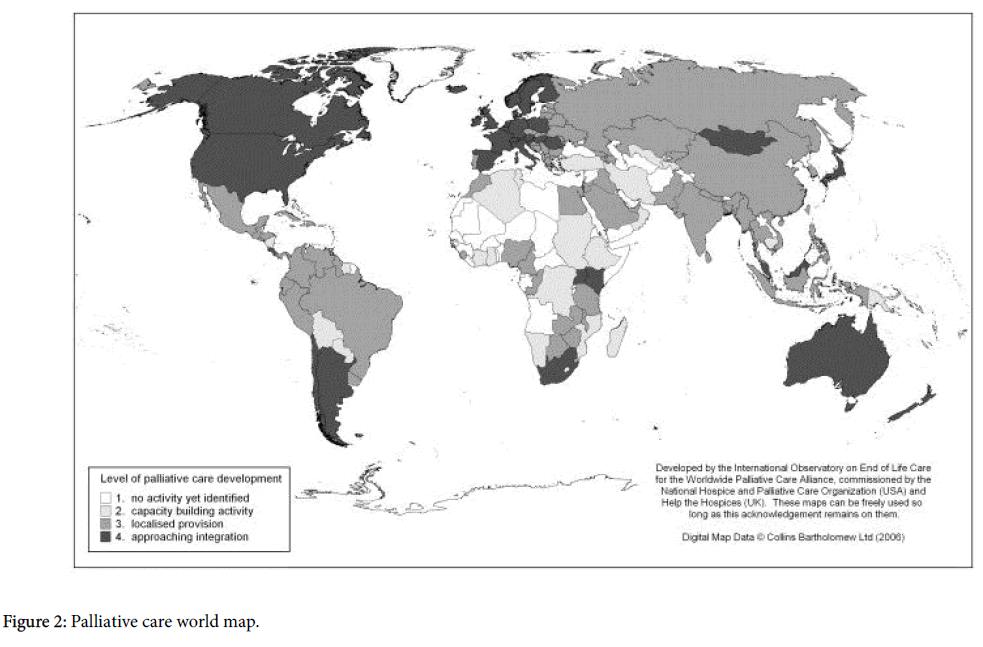
Physician assisted suicide is associated with female gender with situations indicate emotional vulnerability such as living alone, and being divorced [7]. Which may explain the large increase in physician assisted suicide incidence of 3 in 1000 deaths to 11 in 1000 deaths found in 2001 and 2013 respectively [31]. Furthermore, terminally ill patients with depression in Oregon have obtained prescriptions for lethal medication [32]. Also physician assisted suicide has been associated with 6.3% increase in the total suicide rates in the US [33]. All these information may indicate malpractice related to physician assisted suicide. Palliative care is intended to im prove the quality of life of patients diagnosed with an incurable life-limiting illness and their families, that offered by a multidisciplinary team [34]. Palliative care is available in many countries around the world, especially those that legalized the use of physician assisted suicide (Figure 2).
According to a study conducted in US in 2015 about palliative care and use it among terminally ill patients, they found that 90% of US people don’t know about palliative care, after told the definition, more than 90% say they would request it for themselves and for their family members in such cases [35].
Therefore, the author composed the following recommendations related to use of palliative care for terminally ill patients instead of physician assisted suicide:
• Palliative care is a crucial medical option for treating symptoms among terminally ill patients, which also could extends to their families.
• Improve and develop palliative care programs and target vulnerable patients or groups (uninsured, the poor and elderly people).
• Adequate services related to palliative care must be made available in all setting where terminally ill patients received care.
• Respect competent patient’s right to accept or reject any medical care.
• Investment to improve and develop palliative care and end-of-life care through research and training.
• Conducting courses and seminars to educate patients' families about possible options which available in palliative care, in order to increase public awareness about palliative care options.
In addition, palliative care can address a broad range of issues, integrating an individual’s and family’s specific needs such as; emotions which accompanies the disease journey, spiritual needs, and practical needs (advance directive).
Summary and Conclusion
The purpose of this paper was to create an argumentative essay to refute the use of physician assisted suicide for terminally ill patients as a last resort to end their suffer and end their life, while taking the legal and ethical points of view of opponents and proponents into consideration, and use palliative care instead it [36-38].
Physician assisted suicide for terminally ill patients is a controversial issue, with a lot of ethical, legal, and moral concerns. In the light of material covered above, we against the use of physician assisted suicide to end patients suffering, instead of that palliative care can provide wide range of care for those patients as well as their families. So that there are need to improve and develop palliative care programs, also increase organizational and societal awareness about palliative care options for terminally ill patients.
References
- Hadders H (2009) Enacting death in the intensive care unit: Medical technology and the multiple ontologies of death. Health 13: 571-587.
- McMurray RJ, Clarke OW, Barrasso JA, Clohan DB, Epps CH, et al. (1992) Decisions near the end of life. JAMA 267: 2229-2233.
- Weiss SC, Emanuel LL, Fairclough DL, Emanuel EJ (2001) Understanding the experience of pain in terminally ill patients. The Lancet 357: 1311-1315.
- Materstvedt LJ, Clark D, Ellershaw J, Forde R, Gravgaard AMB, et al. (2003) Euthanasia and physician-assisted suicide: A view from an EAPC Ethics Task Force. Palliat Med 17: 97-101.
- Canadian Medical Association (2014) Euthanasia and assisted death (update 2014). CMA Policy: 1-4.
- Shankaran V, LaFrance RJ, Ramsey SD (2017) Drug price inflation and the cost of assisted death for terminally ill patients-death with indignity. JAMA Oncol 3: 15-16.
- Steck N, Junker C, Maessen M, Reisch T, Zwahlen M, et al. (2014) Suicide assisted by right-to-die associations: A population based cohort study. Int J Epidemiol 43: 614-622.
- Hulkower R (2016) The history of the Hippocratic Oath: Outdated, inauthentic, and yet still relevant. Einstein J Biol Med 25: 41-44.
- Nippold MA, Ward-Lonergan JM (2010) Argumentative writing in pre-adolescents: The role of verbal reasoning. Child Lang Teaching Ther 26:238-248.
- Canadian Medical Association (2007) CMA Policy-Euthanasia and Assisted Suicide (Update 2007).
- Raus K, Sterckx S, Mortier F (2011) Is continuous sedation at the end of life an ethically preferable alternative to physician-assisted suicide? Am J Bioeth 11: 32-40.
- Dieterle JM (2007) Physician assisted suicide: A new look at the arguments. Bioethics 21: 127-139.
- Chin AE, Hedberg K, Higginson GK, Fleming DW (1999) Legalized physician-assisted suicide in Oregon-the first years’ experience. N Engl J Med 340: 577-583.
- National People's Congress of the People's Republic of China “Criminal Law of the People's Republic of Chinaâ€.
- United Nations Office on Drugs and Crime “Turkey Criminal Code†(2004).
- UK Legislation "Coroners and Justice Act 2009," legislation.gov.uk, 2009
- The Medical Constitution and Duties of the Physician and Profession 1989.
- Schwarzenegger C (2005) Patient’s Right Council Switzerland. “Criminal Law and Assisted Suicide in Switzerland†2: 1-6.
- https://www.oregon.gov/oha/PH/PROVIDERPARTNERRESOURCES/EVALUATIONRESEARCH/DEATHWITHDIGNITYACT/Pages/index.aspx
- https://www.doh.wa.gov/YouandYourFamily/IllnessandDisease/DeathwithDignityAct
- Ministry of Social Affairs and Health, "Human Dignity, Hospice Care and Euthanasia," etene.fi, Jan. 1, 2012
- Gaylin W, Kass LR, Pellegrino ED, Siegler M (1988) Doctors must not kill. JAMA 259: 2139-2140.
- Loggers ET, Starks H, Shannon-Dudley M, Back AL, Appelbaum FR, et al. (2013) Implementing a death with dignity program at a comprehensive cancer center. N Engl J Med 368: 1417-1424.
- Mount BM, Boston PH, Cohen SR (2007) Healing connections: On moving from suffering to a sense of well-being. J Pain Symptom Manage 33: 372-388.
- Ganzini L (2014) Lessons from legalized physician-assisted death in Oregon and Washington. Palliative Care and Ethics: 266.
- Callahan D (1992) When Selfâ€Detertnination Runs Amok. Hastings Center Report 22: 52-55.
- Bosshard G, Zellweger U, Bopp M, Schmid M, Hurst SA, et al. (2016) Medical end-of-life practices in Switzerland: A comparison of 2001 and 2013. JAMA Int Med176: 555-556.
- Ganzini L, Goy ER, Dobscha SK (2008) Prevalence of depression and anxiety in patients requesting physicians’ aid in dying: Cross sectional survey. BMJ 337: a1682.
- Jones DA, Paton D (2015) How does legalization of physician assisted suicide affect rates of suicide? Southern Med J 180: 599-604.
- Australia PC (2005) Standards for providing quality palliative care for all Australians. Palliative Care Australia.
- Kelley AS, Morrison R S (2015) Palliative care for the seriously ill. N Engl J Med 373: 747-755.
- Cook D, Swinton M, Toledo F, Clarke F, Rose T, et al. (2015) Personalizing death in the intensive care unit: The 3 Wishes Project: A mixed-methods study. Ann Intern Med 163: 271-279.
- Farnan JM, Snyder LS, Worster BK, Chaudhry HJ, Rhyne JA, (2013) Online medical professionalism: Patient and public relationships: policy statement from the American College of Physicians and the Federation of State Medical Boards. Ann Intern Med 158: 620-627.
- The American Heritage Dictionary of the English Language (2018) Assisted suicide.
Citation: Ababneh AMT (2018) Physician Assisted Suicide for Terminally Ill Patients: An Argumentative Essay. J Palliat Care Med 8: 337. DOI: 10.4172/2165-7386.1000337
Copyright: © 2018 Ababneh AMT. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 29013
- [From(publication date): 0-2018 - Apr 28, 2025]
- Breakdown by view type
- HTML page views: 27781
- PDF downloads: 1232