Research Article Open Access
Physical and Functional Limitations in US Older Cancer Survivors
Prachi P Chavan1, Satish K Kedia2 and Xinhua Yu1*1Division of Epidemiology, Biostatistics, & Environmental Health, School of Public Health, University of Memphis, TN, USA
2Division of Social & Behavioral Sciences, School of Public Health, University of Memphis, Memphis, TN, USA
- *Corresponding Author:
- Xinhua Yu
Division of Epidemiology, Biostatistics, & Environmental Health
School of Public Health, University of Memphis, TN, USA
Tel: +1-901-678-3433
Fax: +1-901-678-1715
E-mail: xyu2@memphis.edu
Received date: June 30, 2017; Accepted date: July 20, 2017; Published date: July 25, 2017
Citation: Chavan PP, Kedia SK, Yu X (2017) Physical and Functional Limitations in US Older Cancer Survivors. J Palliat Care Med 7:312. doi: 10.4172/2165-7386.1000312
Copyright: © 2016 Chavan PP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: The ability to independently perform daily activities is a crucial component of quality of life among older cancer survivors. However, many cancer survivors face difficulties performing their daily activities for living an independent life. The purpose of this study was to evaluate whether physical and functional status significantly decreased in cancer survivors compared to people without cancer.
Methods: The Medicare Current Beneficiary Survey (MCBS) is a nationally representative longitudinal study for the entire aged Medicare beneficiaries. Data from 2006 to 2010 were used for analysis of this study. Design-based descriptive analysis and logistic models with adjusted survey weights were performed. To ensure comparability between cancer and non-cancer older adults, propensity score weighting was developed using logistic regressions.
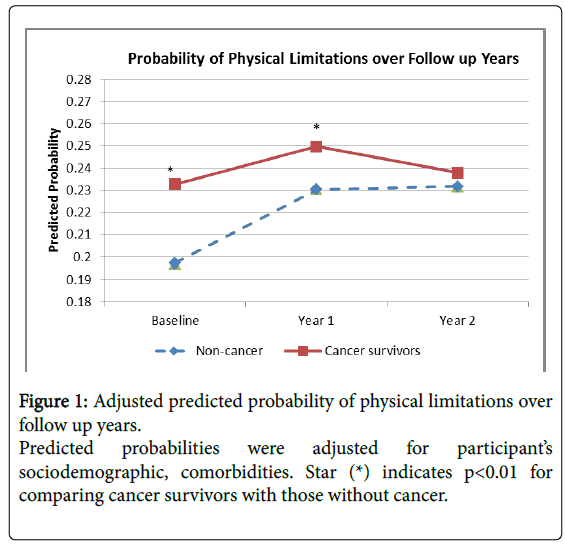
Results: The final sample consisted of 11,533 participants. Cancer survivors had more limitations compared to non-cancer individuals: physical limitations (23.3% vs. 19.7%, p=0.006), activity daily living limitations (ADL) (7.7% vs. 5.8%, p=0.02), and instrumental activity of daily living limitations (IADL) (13.5% vs. 11.0%, p=0.02. The odds ratio (OR) for cancer survivors compared to non-cancer individuals was 1.62 (95% CI: 1.28-2.06) for physical limitations, 1.08 (95% CI: 0.72-1.62) for ADL, and 1.30 (95% CI: 0.97-1.73) for IADL. There was a one year lag in functional limitations resulting in one year loss of physical capabilities among cancer survivors. However, these differences between cancer and non-cancer participants decreased over the follow-up year (p=0.01).
Conclusion: Cancer survivors have higher prevalence of physical and functional limitations compared to noncancer individuals. Such disparities in functional limitations impact the independent functioning of these survivors. Healthcare professionals need to recognize potential for debilitating functional abilities among cancer survivors and address their needs. Our findings extend our understanding of the burden of physical and functional limitations in cancer survivors and call for action from health care providers.
Keywords
Cancer survivors; Older adults; Medicare; Functional limitations; ADL; IADL; Quality of life
Introduction
More Americans now live with cancer than before, with 15.5 million cancer survivors in 2016 and an estimated 20.3 million by 2026 [1]. Almost two-thirds of them are 65 years or older [2]. Older adult cancer survivors are challenged not only by cancer-related treatment complications, comorbidities, and psychosocial impairments but also by age-related physical degeneration and functional limitations [3]. For example, older female cancer survivors who underwent surgical treatment reported more functional limitations than non-cancer females, which led to restricted independence in daily activities and lower quality of life [4].
Physical, functional, and psychosocial well-beings are important components of health-related quality of life [5]. Physical and functional limitations refer to the inabilities to perform essential daily tasks for living a worthwhile life at home. We classified activities like walking, lifting, stooping, and sitting as physical activities; activities of daily living (ADL) was classified by activities such as using toilet, dressing, bathing, eating, and walking around the house; and instrumental activities of daily living (IADL) was classified by activities such as using telephone, doing housework, preparing meals, paying bills, and shopping. Together these activities fulfill the basic human needs. Also, physical and functional limitations are inter-dependent. More physical limitations may lead to increased ADL and IADL, whereas limitations in ADL and IADL may cause social isolation and negligence in personal health, which may result in worse physical and mental health outcomes [6]. In addition, other factors such as comorbidities and lack of caregivers may also affect the extent and the quality of daily living activities [7]. Patient satisfaction with medical care and quality of life differ based on severity of functional limitations. Knowledge about patient’s activity of daily living could provide helpful insight into their quality of life [8].
Previous studies have explored physical and functional limitations among cancer survivors [9-11], demonstrating that elderly individuals who were less engaged in physical activities were at increased risk of having functional limitations [5,12]. However, most previous studies were based on cross-sectional study designs or examined the functional limitation as summary indices [13,14]. Some earlier studies did not adequately address the comparability between cancer survivors and non-cancer older adults regarding age, comorbidities, and other confounders based on modern causal inference framework [15,16]. A thorough understanding of physical and functional limitations among elderly cancer survivors may shed new light on targeted improvement in their quality of life.
In this study, we will examine physical and functional limitations among older adult cancer survivors using propensity score weighting to ensure comparability between those with and without a history of cancer diagnosis. We hypothesized that older cancer survivors have more physical and functional limitations and increased deterioration of functional status compared to non-cancer older adults.
Methods
Study cohort
We used the Medicare Current Beneficiary Survey (MCBS) data from the year 2006 to 2010. The MCBS is a nationally representative longitudinal, stratified, multi-stage survey of the entire aged Medicare beneficiaries, administered by the Centers for Medicare and Medicaid Services (CMS). Three interviews are conducted each year over a period of four years to track health status changes and health care use among older adult Medicare beneficiaries [17]. The MCBS conducts interviews using a questionnaire version appropriate to the setting based on whether the sample person resides at home or in a long-term care facility. In Fall season of each year, one third of survey participants are rotated out and replaced by an equivalent number of new participants. The representative MCBS sample is selected through a three-stage process, the first stage includes selection of primary sampling units consisting of metropolitan statistical areas or clusters of non-metropolitan counties. The second stage includes sampling of zip code clusters with primary sampling units and in the third stage beneficiaries are sampled within the zip code clusters. The MCBS oversamples individuals less than 65 years of age and greater than 80 years of age to increase the precision estimates of the above mentioned three groups. In this study, we used information on demographic and socioeconomic characteristics, health status, and physical and functional limitations of participants collected during each Fall round of the survey. Information collected in other rounds mainly focuses on access to health care and health care utilization during the year, thus was not used in this study.
We restricted our study cohort to participants aged 65 years or older (n=22,915 at baseline), and excluded people who were diagnosed with cancer within one year prior to the baseline survey, those who developed new cancer during the study period (n=821), and those who died during the survey years (n=1,458) because they might have different disabilities and health needs. Further, we included only those with at least one follow up interview during the study period, i.e., those who interviewed in Fall rounds of the year and had additional interviews the following year (n=11,632). Thus, some participants had three visits while some only had two. Those with missing values in functional limitations (n=99) were also excluded. Since the MCBS is a multi-stage survey design, it provides sample weights to adjust for the non-response rate. The sum of these sample weights provides an unbiased estimate of the total number of individuals in the target population. They are interpreted as the number of individuals in the target population and what each sample participant is estimated to represent. Our final sample consisted of 11,533 participants, representing a weighted total of 48,517,805 aged Medicare beneficiaries.
Measuring physical and functional limitations
Each year the MCBS measures self-reported physical and functional limitations activities of daily living and instrumental activities of daily living [18] (Table 2). Each limitation domain includes five or six items, and each item is measured on a five-point scale. Based on the measurement questionnaire we classified physical limitations as difficulty in stooping/crouching/kneeling, walking ¼ miles, reaching/ extending arms above shoulder, lifting/carrying 10 lbs., and writing/ handling objects; ADL limitations included difficulty in bathing, dressing, walking in the house, eating, getting in and out of chair or bed, and using toilet; and IADL limitations included difficulty in using telephone, shopping, doing light house work, preparing meals, and paying bills. The distribution of score in each item was highly skewed, typically only 10-20% scored “a lot of difficulty (4)” and “not able to do it (5)”. The summary score was highly skewed as well. Thus, we did not create a measurement scale based on summary score which is often used in model adjustment. We classified any item response with a score of 4 or 5 as having a limitation. We then further classified having two or more limitations in each domain as having a functional limitation. Participants having at least one ADL or IADL limitations were defined as having ‘any functional limitations’.
Measuring demographic variables, cancer status, and comorbidities
The MCBS collects socio-demographic and health status information during the face-to-face interviews. We included sociodemographic characteristics such as, age at baseline survey (recoded as 65-74, 75-84, and 85 or older), gender, income (<$15,000, $15,000 - $30,000, and ≥ $30,000), and race/ethnicity (recoded as Caucasian, African-American and Other).
History of cancer diagnosis was assessed in questions such as “ever told having a non-skin cancer”, “had a cancer past year” and body part (site) of cancer. Consistent with the definition adopted by National Cancer Institute, we defined cancer survivors as those having survived cancer from the time of cancer diagnosis until end of life [19]. Those with non-melanoma skin cancer were not considered cancer survivors because of the non-invasiveness of cancer.
The number of comorbidities was based on the number of selfreported clinical conditions, including heart disease, stroke, arthritis, chronic obstructive pulmonary disease (COPD), paralysis/amputation, bone disease, diabetes, hypertension, psychiatric disorder, neurological disease including dementia and Alzheimer’s disease, recorded as yes or no on the questionnaires. Multiple chronic conditions were defined as having two or more of the above chronic conditions, excluding hypertension due to its high prevalence. This is similar to other comorbidity measures such as Charlson’s Index in which hypertension is not considered [20].
Statistical analysis
We adopted the potential outcome causal inference framework [21] and employed propensity score methods to obtain a correct estimate of average differences in physical and functional limitations between cancer survivors and people without cancer. We generated a quadratic term age2 to determine the effect of age on the outcome based on each year. We included the squared term in the analyses because each year’s age effect might be non-linearly related to the cancer status of individuals. The age2 was to capture the complicated relationship between age and cancer status. Specifically, we first conducted a logistic regression using baseline data with cancer status as the dependent variable, and age, age2, race, sex, income level, and all comorbidities as predictors. In addition, as suggested by Du Goff et al. [22], the survey stratum and survey weight were also included as predictors in logistic regression but were not weighted in the model for propensity score analysis. The propensity score (P), i.e., the estimated probability of potentially having a cancer diagnosis for all participants, was estimated from logistic regression as follows:
We then calculated a new weight as the product of the original MCBS cross-sectional sampling weight and 1/P for cancer survivors, or 1/(1-P) for people without cancer. This new weight discounted more on those participants who were in the tails of propensity score distributions. In addition, we also multiplied the new weight with the average P for cancer survivors or the average 1-P for people without cancer to correct the outliers in the new weights. All analyses were then weighted by the final weight.
The distributional balance of socio-demographic characteristics and comorbidities between cancer survivors and people without cancer was assessed using weighted mean and standard error (SE) for continuous variables, and weighted frequency and percentage for categorical variables, using t test and Rao-Scott χ2 test, respectively. The weighted prevalence of various limitations by cancer status was compared using Rao-Scott χ2 test as well. The independent effect of cancer status on each of the limitations was estimated at the baseline with separate multivariate logistic regression models adjusting for sociodemographic characteristics and comorbidities. The average predicted marginal probabilities of having limitations in each year were similarly estimated using logistic regression, adjusting for socio-demographic characteristics and comorbidities.
All analyses were based on the multi-stage survey design with appropriate subpopulation (domain) analysis and with the above new weights using SAS version 9.4 (SURVEYFREQ, SURVEYMEANS, and SURVEYLOGISTIC). A more stringent p value for statistical significance (p<0.01) was used to take account of multiple comparisons in Table 2 and 3.
Results
There were 17.6% of participants who were diagnosed with cancer at least one year before the baseline survey. As shown in Table 1, the goal of balancing measured confounders between participants with and without cancer was achieved. There was no significant difference in socio-demographic characteristics and comorbidities by cancer status after propensity score weighting. The weighted mean age was 75 years, about 58% of participants were females, 8% were African Americans, and 24% lived with a median income <$15,000 for both groups. Except for bone diseases, there was no statistical difference in the prevalence of various self-reported comorbidities. About 58% of cancer survivors had multiple chronic conditions and overall cancer survivors had a slightly higher prevalence of medical comorbidities.
| Characteristics | Cancer survivors (weighted: 17.6%) N=1,890 | People with no cancer (weighted: 82.4%) N=9,643 | P-value |
|---|---|---|---|
| Age (Mean,SE) | 74.6(0.20) | 74.7(0.07) | 0.6 |
| 65 to 74 | 55.4 | 54.4 | 0.68 |
| 75 to 84 | 35.4 | 35.5 | |
| ≥ 85 | 10.2 | 10.1 | |
| Gender | |||
| Male | 42 | 43.4 | 0.41 |
| Female | 58 | 56.6 | |
| Race/ethnicity | |||
| Caucasian | 86.5 | 87.4 | 0.43 |
| African American | 7.8 | 8.1 | |
| Other | 5.7 | 4.6 | |
| Income (per year) | |||
| <$15,000 | 24 | 23 | 0.63 |
| $15,000 to $30,000 | 33.8 | 33.4 | |
| ≥ $30,000 | 42.2 | 43.6 | |
| Comorbidities | |||
| Heart Disease | 40.8 | 41.3 | 0.76 |
| Stroke | 9.9 | 9.8 | 0.84 |
| Arthritis | 62.2 | 59 | 0.03 |
| COPD | 16.3 | 15.2 | 0.23 |
| Paralysis/Amputation | 3.9 | 3 | 0.04 |
| Bone Disease | 26.9 | 22.7 | 0.004 |
| Diabetes | 18.9 | 18.1 | 0.51 |
| Hypertension | 67.4 | 65.4 | 0.23 |
| Neurological disease | 9.7 | 9.3 | 0.63 |
| Psychological disease | 10.2 | 9.1 | 0.28 |
| Multiple chronic conditions (≥ 2) | 58.1 | 56.7 | 0.38 |
| Site of Cancer | |||
| Lung | 3.8 | NA | - |
| Breast | 29.2 | NA | - |
| Prostate | 22.5 | NA | - |
| Colon | 11.9 | NA | - |
| Kidney | 2.4 | NA | - |
| Other cancer | 30.2 | NA | - |
Cancer survivors: Unweighted N=1,890; Weighted N=8,523,945; People without cancer: Unweighted N=9,643; Weighted N=39,993,860. Hypertension was not counted in classifying multiple chronic conditions due to its high prevalence.
Table 1: Demographic characteristics of elderly medicare survivors and individuals without cancer.
Table 2 presents the weighted prevalence of physical, ADL and IADL limitations at the baseline survey by cancer status. Older cancer survivors were more likely to experience limitations in all three domains than those without cancer. Cancer survivors had higher prevalence of having two or more physical limitations (23.3% vs. 19.7%, p=0.006), and increased prevalence in all physical limitations except for difficulty in walking and writing. Difficulty in stooping was the most common physical limitation, seen in 30.9% of cancer survivors. Similarly, cancer survivors had slightly higher prevalence of ADL limitations compared to non-cancer participants (7.7% vs. 5.8%, p=0.02), Limitations such as difficulty in preparing meals (p=0.002) and shopping (p=0.008) were found to be statistically significant. Cancer survivors were also more likely to have IADL limitations (13.5% vs. 11.0%, p=0.02), especially difficulties in bathing, using the toilet and getting in and out of bed or chair. When ADL and IADL were combined, cancer survivors were significantly more likely to have ‘any functional limitations’ than people without cancer (16.1% vs. 13.1%, p=0.008).
| Functional Limitations | Cancer survivors (weighted %) | People without cancer (weighted %) | P-value |
|---|---|---|---|
| Two or more physical limitations | 23.3 | 19.7 | 0.006 |
| Difficulty in stooping/crouching | 30.9 | 26.3 | 0.0005 |
| Difficulty in walking ¼ miles | 23.4 | 21.2 | 0.11 |
| Difficulty in reaching/extending | 8.9 | 6.1 | 0.0008 |
| Difficulty in lifting 10 lbs. | 14.9 | 11.8 | 0.003 |
| Difficulty in writing/handling objects | 4.1 | 4.5 | 0.47 |
| Two or more IADL limitations | 7.7 | 5.8 | 0.02 |
| Difficulty in using telephone | 5.3 | 4.4 | 0.18 |
| Difficulty in doing light housework | 7.4 | 5.6 | 0.02 |
| Difficulty in preparing meals | 6.2 | 3.9 | 0.002 |
| Difficulty in shopping | 9.1 | 6.8 | 0.008 |
| Difficulty in paying bills | 3.5 | 2.8 | 0.24 |
| Two or more ADL limitations | 13.5 | 11 | 0.02 |
| Difficulty in bathing | 8.5 | 6.8 | 0.03 |
| Difficulty in dressing | 4.9 | 4.4 | 0.42 |
| Difficulty in eating | 1.5 | 1.2 | 0.33 |
| Difficulty in walking in the house | 21.4 | 19.3 | 0.11 |
| Difficulty in using toilet | 4.2 | 3.1 | 0.05 |
| Difficulty in getting in and out of bed or chair | 11.8 | 9.3 | 0.01 |
| Any functional limitation | 16.1 | 13.1 | 0.008 |
Table 2: Physical, Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) limitations in older adult medicare beneficiaries, cancer survivors and people without cancer.
After adjusting for socio-demographic characteristics and comorbidities, cancer survivors were more likely to have physical functional limitations than older adults without cancer [adjusted odds ratio (OR): 1.62 (95% confidence interval (CI): (1.28–2.06)], whereas no statistical difference was found in ADL limitations (OR: 1.08 (0.72– 1.62)) and IADL limitations [OR: 1.30 (0.97–1.73)] (Table 3). Overall, cancer survivors were 24% more likely to have any functional limitations than people without cancer [OR: 1.24 (0.95–1.62)]. In addition, factors such as older age, being a male, lower income level, and presence of multiple comorbidities were significantly more likely to increase physical and functional limitations in participants (Table 3).
| Determinants | Adjusted OR(95% CI) | |||
|---|---|---|---|---|
| Two or more physical limitation | Two or more ADL limitation | Two or more IADL limitation | Any limitation | |
| Cancer survivors vs. Non-cancer | 1.62 (1.28–2.06)a | 1.08 (0.72–1.62) | 1.30 (0.97–1.73) | 1.61 (1.29–2.02)a |
| Age (per year) | 1.04 (1.03–0.05)a | 1.04 (1.03–1.05)a | 1.04 (1.03–1.05)a | 1.04 (1.03–1.05)a |
| Female vs. male | 0.69 (0.61–0.78)a | 0.71 (0.61–0.83)a | 0.76 (0.65–0.88)a | 0.74 (0.66–0.83)a |
| African American vs. Caucasian | 1.01 (0.82–1.23) | 1.45 (1.11–1.89) | 1.14 (0.94–1.39) | 1.03 (0.86–1.22) |
| Income (ref: <$15,000 per year) | -- | -- | -- | -- |
| $15,000 to $30,000 | 0.70 (0.62–0.80)a | 0.67 (0.53–0.85)a | 0.74 (0.61–0.89)a | 0.68 (0.59–0.78)a |
| ≥ $30,000 | 0.36 (0.31–0.42)a | 0.34 (0.25–0.45)a | 0.48 (0.40–0.58)a | 0.37 (0.32–0.43)a |
| Comorbidity (≥ 2 vs. <2) | 4.30 (3.31–4.99)a | 4.92 (3.94–6.16)a | 4.62 (3.88–5.51)a | 4.33 (3.80–4.95)a |
| Site of Cancer (compared with non-cancer) | ||||
| Lung | 0.77 (0.42–1.39) | 0.95 (0.44–2.08) | 0.93 (0.51–1.71) | 0.79 (0.45–1.38) |
| Breast | 0.71 (0.49–1.02) | 1.62 (0.84–3.13) | 1.03 (0.71–1.49) | 0.76 (0.55–1.06) |
| Prostate | 0.52 (0.36–0.75)a | 1.36 (0.71–1.58) | 0.86 (0.55–1.35) | 0.66 (0.46–0.94) |
| Colon | 0.71 (0.47–1.07) | 0.81 (0.41–1.60) | 0.94 (0.61–1.44) | 0.71 (0.49–1.04) |
| Kidney | 0.67 (0.28–1.58) | 0.54 (0.10–2.83) | 0.67 (0.13–1.58) | 0.84 (0.35–2.00) |
OR: Odds Ratio, CI: Confidence Interval; Models were adjusted for age, race, sex, income, medical comorbidities, site of cancer, and first entrance round to the survey ap<0.01.
Table 3: Adjusted odds ratios of determinants of physical and functional limitations at baseline.
We further conducted sensitivity analysis using the backward elimination method for each individual comorbidity in a multivariable model, and found that cancer survivors still had significantly higher physical limitations than people without cancer but the same was not true for ADL and IADL limitations. Furthermore, after restricting our sample to those without multiple comorbidities, results were similar but were non-significant due to the smaller sample size. The time trends for predicted probabilities of functional limitations were similar as shown in Figures 1 and 2.
Discussion
Our study demonstrated that elderly cancer survivors suffered more physical and functional limitations in their daily activities than those without cancer. Such disparities negatively impact the ability of independent living at home among older cancer survivors. In addition, there was about one year difference in the probability of having functional limitations between cancer survivors and non-cancer individuals, suggesting that public health interventions at an early stage may improve the quality of life in this population.
Several studies have examined the differences in health status of cancer survivors [10,23], and a few have assessed the age-related and cancer-related functional impairment, comorbidities, and other psychological problems. Hamama-Raz et al. reported a stronger reciprocal relationship between functional limitations and quality of life among cancer survivors above 75 years of age [9], and Wolinsky et al. also showed a decline in activities of daily living among older adult cancer survivors with greater odds of functional decline before one year of death [24]. Our results are in line with these previous studies.
Our findings enhanced the understanding of the burdens of physical and functional limitations among cancer survivors. Previous studies have shown that older cancer survivors face physical, emotional, and social challenges in their daily lives [24,25]. By examining the patterns of limitations and exploring items in each domain, we could identify key barriers faced by older cancer survivors in their daily lives. We found that physical limitation activities were instrumental in affecting cancer survivor’s mobility and independence. The higher prevalence of physical limitations among older cancer survivors may be due to the impact of cancer and its treatment on physical functions of the body, as cancer related surgery, chemotherapy, and radiation therapy may have an impact on the physical functions, and can often lead to some irreversible changes in the body. ADL and IADL limitations among non-cancer older adults, were also related to impaired physical functioning of the body.
Furthermore, cancer survivors were more likely to have multiple comorbidities [15,26]. On an average a long-term cancer survivor has five medical comorbidities [26] and most comorbidities and disabilities have been associated with poor mental and physical health [11]. In some of these individuals, identifying patterns and mechanisms of functional limitations, preventing or slowing the progression of symptom deteriorations, and improving quality of life may be more important than the treatment of the disease.
Our study suggested a one year loss of physical capacity due to cancer-related disabilities, as predicted in the figures showing the prevalence of physical and any functional limitations. Again, this may be due to the inevitable consequences of cancer and its treatment on physical functioning of the body. Such differences negatively affect the quality of life among cancer survivors. For instance, cancer survivors had difficulties in shopping, preparing meals and getting in and out of bed and chair. However, since there is a one year lag between cancer survivors and non-cancer individuals, physical and functional limitations among older cancer survivors could be improved through physical therapy and muscle strengthening activities to regain physical strength and function, as demonstrated by two previous studies [5,27].
In addition, health care needs for older cancer survivors tend to be more disintegrated and disorganized. Health care providers, including oncologists, primary care physicians, and geriatricians, should pay more attentions to the functional status of older cancer survivors during their clinic visits. Coordinating follow up care and adequately addressing their health needs during subsequent visits can be challenging [28], due to limited time slot for each clinic visit and competing demands in managing various chronic conditions [29]. However, some measures of functional limitations should be made as a part of the routine cancer survivorship care. Risk estimation for physical and functional limitations should be developed [30], which helps devise more coordinated and tailored care plan for older adult cancer survivors.
The most important strength of our study is our analysis which is based on the modern causal inference theory. We adopted the potential outcome framework and used propensity score methods to ensure that cancer survivors and those without cancer were comparable in key confounders. The unadjusted prevalence of physical and functional limitations presented in Table 2 were adjusted implicitly through propensity score weighting, and were un-confounded by variables we presented in Table 1. Another main strength of the study is that MCBS is a nationally representative survey and we obtained a complete profile of both physical and functional limitations experienced by the older population, therefore inferences from this study can be applied to the older adult cancer survivor population.
This study also has a few limitations. The MCBS questionnaires did not have detailed cancer staging, disease severity, stage of recovery, and treatment information. Differences in these factors can lead to different trajectories of physical and functional limitations. The age of cancer diagnosis was not available except an indicator of whether cancer was diagnosed during the past year of the survey conducted. Thus, we were not able to identify long-term cancer survivors (survived 5 or more years after diagnosis). In addition, the measures of outcomes and exposures were self-reported and might be subject to recall or interview bias. Propensity score analysis cannot take account of unmeasured confounders, if some of the important confounders are unmeasured, the estimates may be still biased. The data presented in this study is 7 years old so, these individuals must have received antineoplastic therapies over 10 years ago. Today, there may be greater efforts towards improved survivorship care planning that mitigate these limitations; nonetheless, there is a need to identify and manage these limitations in a more proactive manner.
Cancer survivors now live longer due to early detection of cancer, and improved cancer treatment. But they have more physical and functional limitations than those without cancer, resulting in an equivalence of one year loss of physical and functional capacities. Although this difference is disconcerting, it can be reduced through targeted interventions such as prehabilitation training programs and guided physical exercise training. Furthermore, the need for devising an optimal care plan for older cancer survivors is critical. Our study calls for health care providers to incorporate formal assessments of functional status and quality of life into their regular clinical practice.
Conflicts of Interest
The authors declare that there is no conflict of interest associated with this manuscript.
References
- Miller KD, Siegel RL, Lin CC, Mariotto AB, Kramer JL, et al. (2016) Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 66: 271-289.
- de Moor JS, Mariotto AB, Parry C, Alfano CM, Padgett L, et al. (2013) Cancer survivors in the united states: Prevalence across the survivorship trajectory and implications for care. Cancer Epidemiol Biomarkers Prev 22: 561-570.
- Stein KD, Syrjala KL, Andrykowski MA (2008) Physical and psychological longā?term and late effects of cancer. Cancer 112: 2577-2592.
- Sweeney C, Schmitz KH, Lazovich D, Virnig BA, Wallace RB, et al. (2006) Functional limitations in elderly female cancer survivors. J Natl Cancer Inst 98: 521-529.
- Mishra SI, Scherer RW, Snyder C, Geigle P, Gotay C (2014) Are exercise programs effective for improving health-related quality of life among cancer survivors? A systematic review and meta-analysis. Oncol Nurs Forum 41: E326-E342.
- Grov EK, Fosså SD, Dahl AA (2010) Activity of daily living problems in older cancer survivors: A populationā?based controlled study. Health & social care in the community 18: 396-406.
- Sklenarova H, Krümpelmann A, Haun MW, Friederich HC, Huber J, et al. (2015) When do we need to care about the caregiver? supportive care needs, anxiety, and depression among informal caregivers of patients with cancer and cancer survivors. Cancer 121: 1513-1519.
- Bogner HR, de Vries McClintock HF, Hennessy S, Kurichi JE, Sreim JE, et al. (2015) Patient satisfaction and perceived quality of care among older adults according to activity limitation stages. Arch Phys Med Rehabil. 96: 1810-1819.
- Hamamaā?Raz Y, Shrira A, Benā?Ezra M, Palgi Y (2015) The recursive effects of quality of life and functional limitation among older adult cancer patients: Evidence from the survey of health, ageing and retirement in europe. Eur J cancer care 24: 205-212.
- Yang P, Cheville AL, Wampfler JA, Garces YI, Jatoi A, et al. (2012) Quality of life and symptom burden among long-term lung cancer survivors. J Thorac Oncol 7: 64-70.
- Song L, Ji Y, Nielsen ME (2014) Quality of life and health status among prostate cancer survivors and noncancer population controls. Urology 83: 658-663.
- Brach JS, FitzGerald S, Newman AB, Kelsey S, Kuller L, et al. (2003) Physical activity and functional status in community-dwelling older women: A 14-year prospective study. Arch Intern Med 163: 2565-2571.
- Becker H, Kang SJ, Stuifbergen A (2012) Predictors of quality of life for long-term cancer survivors with preexisting disabling conditions. Oncol Nurs Forum 39: E122-E131.
- Roehrig B, Hoeffken K, Pientka L, Wedding U (2007) How many and which items of activities of daily living (ADL) and instrumental activities of daily living (IADL) are necessary for screening. Crit Rev Oncol. 62: 164-171.
- Stenholm S, Westerlund H, Head J, Hyde M, Kawachi I, et al. (2015) Comorbidity and functional trajectories from midlife to old age: The health and retirement study. J Gerontol A Biol Sci Med Sci 70: 332-338.
- Stewart A, Ware Jr JE, Brook RH (1977) The meaning of health: Understanding functional limitations. Med Care 15:939-952.
- http://www.mcbs.norc.org/node/6
- Schüsslerā?Fiorenza Rose SM, Stineman MG, Pan Q, Bogner H, Kurichi JE, et al. (2016) Potentially avoidable hospitalizations among people at different activity of daily living limitation stages. Health Serv Res 52: 132-155.
- https://www.cancer.gov/publications/dictionaries/cancer-terms?cdrid=450125
- Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 40: 373-383.
- Rubin DB (2004) On principles for modeling propensity scores in medical research. Pharmacoepidemiol Drug Saf 13: 855-857
- DuGoff EH, Schuler M, Stuart EA (2014) Generalizing observational study results: Applying propensity score methods to complex surveys. Health Serv Res 49: 284-303.
- Serraino D, Fratino L, Zagonel V, GIOGer Study Group (2001) Prevalence of functional disability among elderly patients with cancer. Crit Rev Oncol 39: 269-273.
- Wolinsky FD, Bentler SE, Hockenberry J, Jones MP, Obrizan M, et al. (2011) Long-term declines in ADLs, IADLs, and mobility among older medicare beneficiaries. BMC Geriatr 11: 43.
- Stineman MG, Streim JE, Pan Q, Kurichi JE, Rose SMS, et al. (2014) Activity limitation stages empirically derived for activities of daily living (ADL) and instrumental ADL in the US adult community-dwelling medicare population. PM&R 6: 976-987.
- Leach CR, Weaver KE, Aziz NM, Alfano CM, Bellizzi KM, et al. (2015) The complex health profile of long-term cancer survivors: Prevalence and predictors of comorbid conditions. J Cancer Surviv 9: 239-251.
- Burnham TR, Wilcox A (2002) Effects of exercise on physiological and psychological variables in cancer survivors. Med Sci Sports Exerc 34: 1863-1867.
- Jacobs LA, Shulman LN (2017) Follow-up care of cancer survivors: Challenges and solutions. Lancet Oncol 18: e19-e29.
- Williams JW (1998) Competing demands. J Gen Intern med 13: 137-139.
- McCabe MS, Partridge AH, Grunfeld E, Hudson MM (2013) Risk-based health care, the cancer survivor, the oncologist, and the primary care physician. Semin Oncol 40: 804-812.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 3582
- [From(publication date):
July-2017 - Jul 13, 2025] - Breakdown by view type
- HTML page views : 2712
- PDF downloads : 870