Pheochromocytoma in Primary Care
Received: 30-Oct-2023 / Manuscript No. jpcm-23-114986 / Editor assigned: 01-Nov-2023 / PreQC No. jpcm-23-114986(PQ) / Reviewed: 15-Nov-2023 / QC No. jpcm-23-114986 / Revised: 20-Nov-2023 / Manuscript No. jpcm-23-114986(R) / Accepted Date: 25-Nov-2023 / Published Date: 27-Nov-2023 DOI: 10.4172/2165-7386.1000590
Abstract
Pheochromocytomas/Paragangliomas are rare tumors arising from chromaffin cells of the adrenal medulla or sympathetic ganglia. The clinical suspicion is mainly based on the signs and symptoms in relation to excess circulating catecholamines including sweating, palpitation, high blood pressure, and headache. After clinical suspicion, biochemical confirmation and radio-logical localization are essential to diagnosis. Treatment is surgical after adequate pharmacological preparation. All patients should do genetic testing. The family physician has an important role in diagnosing these rare tumors. The chain of good health care from family physician to endocrinologist to surgeon is the cornerstone of successful diagnosis and management. Here, we report a case of right adrenal pheochromocytoma and review the related literature.
Keywords
Pheochromocytoma; Hypertension; Secondary hypertension; Rare tumor
Case Study
S.A is a 42-year-old female, engineer by profession who presented to our family medicine clinic with one year history of fluctuating blood pressure. The episodes of raised blood pressure were initially intermittent in nature, than became more repetitive 4 months prior to her presentation. Those episodes were managed at times as stress related and at other times treated with anti-hypertensive medications with variable relief. There was also a history of excessive hyperhidrosis which was noted one year back. In addition, there were episodes of easy sweats, fatigability, palpitations and pulsating headaches upon awakening or with climbing two flights of stairs. The episodes would occur with variable frequency ranging from once or twice weekly up to 4-6 times daily, each episode lasting on average 10-15 minutes. Blood pressure checked during some of those episodes was found to be over 140/100 mmHg.
The patient was otherwise healthy with no history of chronic diseases or surgical procedures. There was no history of tobacco, alcohol or illicit drug abuse; allergy to penicillin was reported; Family history was negative for nephrolithiasis and diabetes but positive for hypertension (father).On physical examination the patient was anxious but not diaphoretic. Blood pressure was 140/100 mmHg, Pulse 92 per minute Respiratory rate 18/minute, temperature 37.1°C, weight 74.2 kg Height 160 cm, Basal Metabolic Index 29 Kg/m2.
Head and Neck, chest and heart examinations were all reported as normal. There were no abdominal striae, palpable masses or bruits. Peripheral pulses were all present and equal. Neurological and musculoskeletal examination was unremarkable.
Laboratory values
CBC, electrolytes, creatinine liver and thyroid function tests were all normal. Fasting blood sugar was 155 mg/dl (8.6 mmol/l) (repeated 7.4 mmol/l)
Hb A1C=7.6%, Total cholesterol 282 mg/dl (7.3 mmol/l); LDL=161 mg/dl (4.17 mmol/ l); HDL=111.8 mg/dl (2.89 mmol/l); T.G=0.52 mmol/l; Ca=2.70 mmol/l (2.1-2.6 mmol/ l); Uric Acid=433 umol/l (145-360 umol/l).
Chest X Ray was also normal. EKG showed sinus rhythm with right atrial enlargement and non-specific T wave changes. There was no evidence of ventricular hypertrophy on|echocardiography.
24 h Urine Collection for fractionated metanephrines and catecholamines: Total Urine Volume=1112 ml
• Metanephrine=621 nmol/24h (Normal: 250-1200 nmol)
• Normetanephrine=52142 nmol ((Normal 750-2000 nmol)
• 3 ortho methyl dopamine=8075 nmol/24h (600-1300).
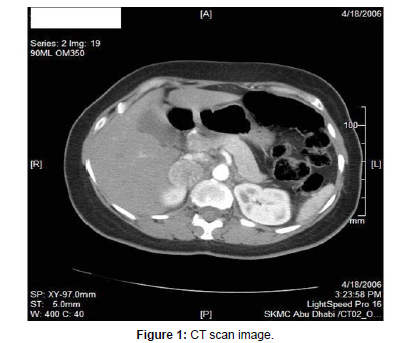
CT scan of Abdomen and Pelvis showed a rounded well demarcated mass in the right suprarenal region, in homogeneously enhancing and measuring approximately 33 x 44 x 28 mm; This mass was seen displacing and compressing the neighboring vena cava. Given the clinical presentation, this mass is a pheochromocytoma. I-131 MIBG metaiodobenzylguanidine Scan. Did not reveal uptake in any other extra adrenal site.
Based on the above findings, the diagnosis of pheochromocytoma was made and the patient referred to Mayo Clinic for consideration of surgery.
The patient was successfully prepared with an alpha 2 agonist and Nicardipine to which metyrosine was added few days later.(Phenoxybenzamine was not included into her regimen because previously documented hypersensitivity reaction to the drug) (Table 1).
| Pre-operative Preparation (drugs/ date) | Day 1 | Day 2 | Day 3 | Day 4 | Day 7 |
|---|---|---|---|---|---|
| Cardene (Nicardipine) | 30 mg bid | 30 mg bid | 30 mg bid | 30 mg bid | 30 mg bid |
| Cardura (Doxazocin) | 1 mg HS | 1 mg HS | 1 mg bid | ||
| Demser (Metyrosine) | 750 mg qid | ||||
| Physiotens (Moxonidine) | 0.2 mg | 0.2 mg | |||
| Weight | 68.4 | 68.9 | 69.8 | 71 | 71.5 |
Table 1:Pre-operative preparation.
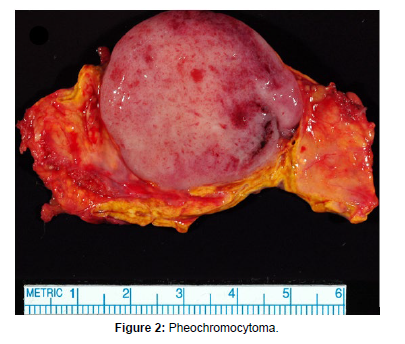
Laparoscopic right adrenalectomy was performed without any complications; a 7.1 x 3.9 x 2.5 cm well-circumscribed tan-colored pheochromocytoma was removed.
On the second day postoperatively, plasma free normetanephrine had normalized at 0.39 nmol/ (<0.90 nmol/l).
One year later, the patient was completely asymptomatic. B.P was 120/75 mmHg on no anti-hypertensive Medications. Fasting blood sugar and 24-h urine collection for catecholamines and metanephrines were also normal (Table 1, Figures 1 and 2).
Discussion
The patient presented to our family medicine clinic for evaluation of hypertension. We confirmed first the diagnosis of hypertension according to the multiple high blood pressure readings she was having since several months and documented in visits to other physicians. In her history and review of system, there were several clues to suspect a secondary cause of her hypertension. Given her age (in the 4th decade) and the type of spells she could describe including the flushing and diaphoresis, which were associated with palpitation, headache and high blood pressure readings, a clinical diagnosis of pheochromocytoma was highly suspected; accordingly, the biochemical confirmation of the diagnosis was successfully made through the high 24 h urine levels of normetanephrine and 3-ortho methyl dopamine. The repeated sample of the 24 h urine, which was advised by the laboratory for confirmation, was not necessary; although we were not convinced, we had repeated the test that showed even higher positive results. CT scan of the abdomen and pelvis then did localization of the tumor in the right adrenal. The high results of fasting sugar, lipids, LFT, uric acid and calcium, which were out before the result of the 24 h urine for metanephrines, were surprising to us and to the patient who was previously told that all her laboratory tests were normal; we thought that these results should have some association together and our differential diagnosis at that stage included metabolic syndrome, hepatitis and pheochromocytoma. Prescribing a central alpha-2 agonist as antihypertensive agent was a good choice in our opinion because its mechanism of action is through decreasing sympathetic over activity caused by high catecholamines secreted by the tumor. Pheochromocytomas are very rare tumors arising from chromaffin cells of the adrenal medulla or sympathetic ganglia (better called paragangliomas in this case). The prevalence is 0.01%- 0.1% of the hypertensive population and 4% of patients with adrenal incidentalomas. The incidence is 2-8 cases / million/year [1,2]. Recent autopsy series showed lower prevalence in comparison to previous early series indicating improvement in the diagnosis of these tumours in living individuals [3]. They may be sporadic or part of several genetic diseases. Their presence in certain familial syndromes will increase their whole-life incidence to 1-5% in neurofibromatosis type 1 (NF1), 15-20% in Von Hippel-Lindau VHL disease (Hemangioblastoma, renal or pancreatic tumors), 30-50% in multiple endocrine neoplasia type 2 (MEN-2, medullary thyroid cancer, hyperparathyroidism), and to above 50% in carriers of succinate dehydrogenase gene mutation subunits B and D (SDHB, SDHD) [2].
These tumors are present equally in men and women, usually between the third and fifth decades of age [4]. Adrenal tumors are usually benign and secrete both epinephrine and norepinephrine in 50% of the cases while extra adrenal tumors are usually aggressive or metastatic in nature and have nor-epinephrine and/or dopamine phenotype [5].
There are 4 steps in catecholamine metabolism: Tyrosine is converted to L-DOPA which is then converted to dopamine which in its turn is converted to norepinephrine and finally to epinephrine. The last step usually occurs in adrenal medulla, so extra adrenal pheochromocytomas do not usually pro-duce epinephrine. Metanephrine and normetanephrine are the metabolites of epinephrine and norepinephrine successively [6].
The diagnosis can be delayed because the symptoms and signs are nonspecific (may mimic several paroxysmal conditions like panic attacks for example), and the hypertension can remain absent for long time as active catecholamines can be converted within the tumor into inactive metanephrines; even when hypertension is present, it was found that the average time lag from the onset of hypertension to the diagnosis is three years [2]. Hypertension can be present in 80-90% of patients with pheochromocytoma, with almost half of them developing sustained hypertension and 45% paroxysmal one, while 5-15% can present with normotension. There is correlation be-tween biochemical phenotype and characteristics of hypertension in a way that sustained hypertension occurs in case of tumours secreting high nor-epinephrine concentrations while paroxysmal and orthostatic hypertension is seen in case of high epinephrine concentrations. Tumors who secrete mainly dopamine will cause mostly normotension [7]. Patients may also present with heart failure. Large tumors secreting norepinephrine may cause episodic bradycardia; this wide range of symptoms, from infarction of the tumor and hemorrhage occasionally to the other extreme with almost no symptoms despite dangerous hypertension, makes the screening of all patients presenting with hypertension or those presenting with unexplained heart failure or with evidence of MEN syndrome very important [6].
There are 3 steps in the diagnosis of Pheochromocytoma including clinical suspicion, biochemical confirmation and radiological localization. The clinical suspicion is mainly based on the signs and symptoms caused by these tumors in relation to the effect of excess circulating catecholamines and which include sweating, palpitation, high blood pressure, pain mainly headache and sometimes chest pain. Flushing is not common, but once presents it is associated with epinephrine and dopamine secretion. The associated hypertension can be either sustained in 50% of the patients or paroxysmal in the other 50%. It is due to increase in total peripheral resistance caused by the high secretion of norepinephrine which is a potent vasoconstrictor secreted by the majority of such tumor. The high suspicion is related to paroxysmal symptoms especially hypertension and to family history of pheochromocytoma [1,13]. Nonspecific symptoms including abdominal pain, constipation, chest pain that mimic myocardial infarction may be caused by sudden release of catecholamines. Because to the multiple clinical presentations, pheochromocytoma is considered as one of the great mimics in medicine, and the physician should think about this disease although it is rare [8].
In our case the hypertension was paroxysmal and the flushing was present and can be explained by its association with the high dopamine secretion noted in the urine. The spells related to pheochromocytoma are variable, usually with duration of 10-60 min and a frequency ranging from daily to several times per year. Our patient had also hyperglycemia in association with her tumor. Diabetes Mellitus in patients with pheochromocytoma has a prevalence of 24%. It was shown that there is a clear association between high catecholamine production and high fasting blood glucose levels. The mechanism includes many factors: alpha receptor mediated inhibition and/or delay in insulin secretion after glucose load, insulin resistance, and increase glucose production by enhancing hepatic glycogenolysis and gluconeogenesis; catecholamines have antagonistic effect on insulin’s stimulation of the transport of glucose over the cell membrane and they reduce the cellular number of insulin receptors [9]. The likelihood ratios of clinical signs and symptoms in diagnosing pheochromocytoma were widely studied and concluded the absence of any clinical finding that could have a significant value in the diagnosis or the exclusion of pheochromocytoma. However, combining some symptoms and signs with paraclinical exams is much important for physicians [10]. Hypercalcemia can also be present in patients with this tumor (as was the case in our patient). It is important to rule out MEN-2-related hypercalcemia. It was found that the secretion of calcitonin depends on catecholamines; hypercalcemia is most of the time isolated and will spontaneously resolve postoperatively [11]. Hyperlipidemia may be also seen in patients with pheochromocytoma due to reduced rate of lipolysis in fat cells in response to catecholamines [9]. The biochemical confirmation should show high levels of fractionated catecholamines (epinephrine, norepinephrine and dopamine) and metanephrines (metanephrine and normetanephrine) in urine or plasma. It was found that measurement of 24 h urine collection of fractionated catecholamines and metanephrines is the most accurate diagnostic method due to its high sensitivity and specificity (both at 98%) [12-14]. The most reliable screening test is metanephrine in 24 h urine collection. In high clinical suspicion, catecholamines, dopamine and VMA should be added and plasma fractionated metanephrines, which are metabolites produced from catecholamines inside the tumor, are very important to mea-sure [15,16]. If the test of plasma fractionated metanephrines is normal, it highly excludes pheochromocytoma except in early preclinical disease or in tumors secreting purely dopamine. Although this plasma test is favored sometimes by some groups because it is simple and more convenient than the 24 h urine collection, it has low specificity at 85- 89% which can drop even to 77% in patients above 60 years of age. Its sensitivity is 96-100%. Therefore, plasma fractionated metanephrines is not recommended as first line test but reserved to cases with high clinical suspicion. Some medications such as labetalol, paracetamol and tricyclic antidepressant may interfere with metanephrines and catecholamines assays. The current use of high-performance liquid chromatography by most laboratories had helped to avoid the problems noted with fluorometric analysis like false positive results caused by some drugs like alpha methyldopa, atenolol and sotalol and false negative results seen with imaging contrast agents. Major stressors such as major surgeries, stroke and malignant hypertension can also result in falsely elevated levels of catecholamines and its metabolites. While recommendations were controversial concerning the first choice screening test for pheochromocytoma between groups favoring 24 h urine collection for metanephrines and catecholamines, and others in favor of plasma fractionated metanephrines, a universal guideline of using urinary metanephrines or plasma free metanephrines as test of choice was proposed at the first pheochromocytoma symposium held in October 2005 [17].
A clinical study showed that, in the absence of renal insufficiency, the three metanephrine-based tests including total plasma metanephrines, free plasma metanephrines, and fractionated metanephrines in urine have the same diagnostic accuracy and it is convenient to associate any two of them for con-firming or excluding pheochromocytoma [18]. In case of kidney failure, the most appropriate and cost-effective screening test is plasma free metanephrines in combination with 24-h urinary metanephrines [19]. A practice guideline for pheochromocytoma and paraganglioma was published by the endocrine society in 2014 recommending using plasma free or urinary fractionated metanephrines as the initial biochemical test and requiring follow-up of all positive results [20]. Radiological localization of the tumor is an important step to guide surgical resection that can cure 90% of patients. It is also an essential tool to know if the tumor is single or multiple, adrenal or ectopic, benign or malignant, sporadic or as part of familial syndromes. It was shown that pheochromocytomas are bilateral in 10% of the cases, malignant in 7%, and familial in 18% (some series mentioned 24%); paragangliomas constitute 13% of all the cases [21].
Computed tomography (CT scan) or magnetic resonance imaging (MRI) of the abdomen is the test of choice. (98% of pheochromocytoma present in the abdomen with 90% of them in the adrenal glands). MRI is preferred for children and pregnant patients. In non-familial cases with an evident bio-chemical diagnosis and a unilateral adrenal mass on CT Scan or MRI, it was originally recommended that no additional functional imaging is needed while taking in consideration the biochemical phenotype of the tumor; for example, the hypersecretion of only epinephrine and its metabolite metanephrine should reflect the presence of adrenal mass whereas patient with noradrenergic biochemical phenotype may have either adrenal, extra-adrenal tumor or both (like in our case) [22,23]. Because research had shown that apparently sporadic tumors are in fact hereditary in at least 24% of the cases, it was finally recommended that the absence of family history should not be the criterion for not doing functional imaging. MEN 2-are at risk for bilateral adrenal pheochromocytoma while hereditary paragangliomas related to succinate dehydrogenase SDH mutations are more associated with metastatic disease and functional imaging should be done accordingly.
In case the abdominal imaging is negative, functional imaging using I-131 MIBG Metaiodobenzylguanidine Scan is helpful where this radioactive product accumulates preferentially in catecholamines producing tumors.
I-131 has lower sensitivity than I-123 which should be used when available. Labetolol, calcium channel blockers, and antipsychotic drugs reduce I-123 MIBG and I-131 MIBG uptake and should be discontinued several days be-fore the investigation (can cause false negative results). I-123 MIBG scintigraphy has lower sensitivity in metastatic pheochromocytoma while it has good performance in primary benign adrenal pheochromocytoma. It was also shown that MRI is less specific for pheochromocytoma/paraganglioma than previously thought. The recent endocrine society practice guideline suggested the initial imaging to be a CT scan, but MRI is preferred in case of metastatic disease suspicion or when the exposure to radiation is an issue. 123I MIBG is advised for metastatic disease. Pheochromocytomas can take up and decarboxylate an amino acid such as dehydroxyphenylalanine DOPA which can be labeled with 18-F to form 18-F-F DOPA. Pemission Tomographic (PET) scan with 18-F fluorodeoxyglucose, fluoro- DOPA, or fluoro dopamine may also be needed sometimes to identify metastatic localization of the tumor in case MIBG is negative (mainly in non-secreting paraganglioma or in discordant results). In VHL carriers, (PET) scan with 18-F-fluoro dopamine is the test of choice; in patients with SDHB mutations, (PET) scan with 18-F fluorodeoxyglucose or 18-F fluoro dopamine is recommended. If PET is not available, scintigraphy with 111-In pentetreotide (Octreoscan), which is a labeled somatostatin analogue, may also be used to locate metastatic disease (can detect 7 out of 8 metastatic cases but only 2 out of 8 of primary benign pheochromocytomas). Newer somatostatin analogues like DOTATOC and DOTANOC labeled with the PET radiotracer (68-Ga) have shown promising superior results compared to Octreoscan scintigraphy. Recent introduction of combined PET/CT Scan had further improved the precision in tumor localization. Adequate pharmacologic preparation before surgery is very important for successful result. It reverses the acute and chronic effects of excess catecholamines. Combined alpha and beta adrenergic blockade is needed to control blood pressure and prevent any hypertensive crisis during surgery. Alpha adrenergic blockade begins 1 week prior to surgery to allow for expansion of the contracted blood volume, Beta adrenergic blockade will be started once alpha blockage is achieved; usually 3 days preoperatively. Phenoxybenzamine is an irreversible, long-acting alpha adrenergic blocking agent, used in dose 20-100 mg/day, has multiple side effects including postural hypotension, tachycardia, nasal congestion, miosis, and fatigue. It is a preferred drug because it provides Alpha adrenergic blockage of long duration. Our patient could not tolerate the side effects of this drug. Doxazosin (Cardura) is a selective alpha 1 adrenergic blocking agent, has less side effects. Beta adrenergic blockade should be done after adequate alpha blockade or else severe hypertension will develop because of unopposed alpha adrenergic stimulation. It is used to control tachycardia associated with high catecholamines and alpha adrenergic blocking. It should be started at low dose with slow increase as needed to control the tachycardia and in a way to avoid any acute pulmonary edema due to the Beta adrenergic blockade use in the presence of any cardiomyopathy that could have been developed due to chronic excess secretion of catecholamines. Catecholamine synthesis inhibitor is usually added whenever tumor manipulation is suspected before the venous outflow from the tumor is controlled, or when alpha and beta adrenergic blockade not tolerated (as in our case) or are not enough to reach target blood pressure value. Alpha-methyl-p-l-tyrosine (Metyrosine) blocks tyrosine hydroxylase enzyme and thus inhibits the synthesis of catecholamines; its side effects include sedation, depression, anxiety, diarrhea, galactorrhea and urolithiasis. It is usually added to help alpha and beta adrenergic blockade in case of suspected difficult resection such as malignant paraganglioma, or in destructive therapy such as radiofrequency ablation of hepatic metastasis. It is usually added 5 days prior to surgery and may have hypersomnolence as side effect. Calcium channel blockers inhibit norepinephrine-mediated calcium transport into vascular smooth muscles. Their effectiveness is comparable to alpha and beta adrenergic blockade when used as the main antihypertensive agent. Nicardipine is the most commonly used. It is usually added when alpha and beta adrenergic blockade is not enough to control blood pressure.
Surgical resection of pheochromocytoma is considered a high risk surgery and it needs an experienced team including a qualified surgeon and anesthesiologist for good outcome. Surgical survival rate 98-100% [24]. Laparoscopic adrenalectomy is typical for solitary adrenal pheochromocytoma less than 8-10 cm. Average hospitalization 1.7-2.3 days. It was shown to be safe and effective as compared with open adrenalectomy. Post-operative pain and post-operative stay were significantly less than those of open adrenelactomy. Operative time, post-operative complications, intra-operative hypertension or hypotension were similar [25]. The patient should be monitored postoperatively for any hypotension which is less common if patient was well prepared preoperatively with effective combined alpha and beta adrenergic blockade and good volume expansion. Blood pressure will be usually normalized by the time of hospital discharge, but some patients may continue to have high blood pressure up to 4 or 6 weeks postoperative. Postoperative follow up should include 24 h urine fractionated metanephrines and catecholamines in 1-2 weeks after surgery. If they are normal (as in our case), this reflects the success of complete surgical resection of the tumor. If not, it means that residual tumor may still be present or there are metastatic lesions. 24 h urine fractionated metanephrines and catecholamines or plasma fractionated metanephrines should be checked yearly for life. Follow up CT scan or MRI is needed when fractionated metanephrines and/or catecholamines become elevated or the original tumor was hormonally nonfunctional. All patients with Pheochromocytoma and/or Paraganglioma should do genetic testing whatever the location of the tumor or the age of the patient. Targeted genetic testing should be considered in case of family history of pheochromocytoma or hereditary paraganglioma (head and neck paraganglioma with family history in the paternal branch) or for any signs suggesting genetic cause like café au lait spots or retinal angiomas, and in case of thyroid carcinoma or hyperparathyroidism (family history of MEN-2-, VHL). The disease has autosomal dominant inheritance for all pheochromocytoma susceptibility genes, but in families with SDHD mutations (succinate dehydrogenase) it is transmitted exclusively via the fathers due to maternal imprinting. In sporadic presentation, VHL and SDHB should be analysed. Malignancy is highly associated with SDHB mutations. All 1st degree relatives of a pheochromocytoma patient should do biochemical testing i.e. 24 h urine fractionated metanephrines and catecholamines. If a patient has positive mutation testing, 1st degree relatives should do stepwise (e.g. parents first) germline screening because early detection of small tumors reduce the morbidity of the disease. According to the recent endocrine society practice guideline, genetic testing should be considered in all patients including testing for SDHx mutations in paraganglioma and for SDHB mutations in metastatic disease.
Conclusion
Although pheochromocytoma is a rare tumor and an uncommon cause of hypertension, the classic presentation of a triad of headache, palpitation, and diaphoresis in a patient with new onset hypertension whether sustained or paroxysmal should prompt one to consider this diagnosis and search for it. The family medicine physician role as the primary health care provider is very important; the chain of good health care from family physician to endocrinologist to surgeon is the cornerstone of successful diagnosis and management. Family physician role is to diagnose uncommon diseases as well as common ones; keeping the physician-patient relationship, which is unique in family medicine, is essential for proper patient care and proper referral at the right time. In our case, proper history taking had given us the clinical clues to highly suspect this tumor and then to do proper biochemical tests for confirmation and later to request the proper radiological tool to localize the tumor. Adequate pharmacologic preparation with alpha adrenergic blockade, calcium channel blocker, and metyrosine along with volume expansion had assure successful surgical removal of the pheochromocytoma and had totally reversed the hypertension as well as the hyperglycemia, hyperlipidemia and hypercalcemia. This case presented to us as a case of hypertension, but it was really more than it seemed.
Declaration of Conflicting Interests
The authors declared no conflict of interest.
References
- Young WF (2003) Pheochromocytoma. Rachel and Bope: Conn’s Current Therapy 2003. Elsevier Science (USA) 724-729.
- Plouin PF, Gimenez-Roqueplo AP (2006) Pheochromocytomas and secreting paragangliomas. Orphanet J Rare Dis 1:1-7.
- Eisenhofer G, Pacak K, Maher ER, Young WF, de Krijger RR (2013) Pheochromocytoma. Clin Chem 59:466-72.
- Young WF, Maddox DE (1995) Spells: in search of a cause. Mayo Clin Proc 70:757-765.
- Havekes B, King K, Lai EW, Romijn JA, Corssmit EP, et al. (2010) New imaging approaches to phaeochromocytomas and paragangliomas. Clinical endocrinology 72:137-145.
- Karet FE, Brown M (1994) Phaeochromocytoma: diagnosis and management. Postgrad Med J 70:326-328.
- Zuber SM, Kantorovich V, Pacak K (2011) Hypertension in pheochromocytoma: characteristics and treatment. Endocrinol Metab Clin North Am 40:295-311
- Därr R, Lenders JW, Hofbauer LC, Naumann B, Bornstein SR, et al. (2012) Pheochromocytoma – update on disease management. Ther Adv Endocrinol Metab 3:11-26.
- Stenström G, Sjöström L, Smith U (1984) Diabetes Mellitus in Pheochromocytoma, Fasting blood glucose levels before and after surgery in 60 patients with pheochromocytoma. Acta Endocrinol 106:511-515.
- Soltani A, Pourian M, Davani BM (2016) Does this patient have Pheochromocytoma? a systematic review of clinical signs and symptoms. J Diabetes Metab Disord 15:6.
- Melmed S, Polonsky KS, Larsen PR, Kronenberg HM (2015) Williams Textbook of Endocrinology. Elsevier Health Sciences.
- Young WF (2007) Adrenal causes of hypertension: Pheochromocytoma and primary aldosteronism. Rev Endocr Metab Disord 8:309-320.
- Kudva YC, Sawka AM, Young Jr WF (2003) The Laboratory Diagnosis of Adrenal Pheochromocytoma: The Mayo Clinic Experience. J Clin Endocrinol Metab 88:4533-4539.
- Sawka AM, Jaeschke R, Singh RJ, Young Jr WF (2003) A Comparaison of Biochemical Tests for Pheochromocytoma: Measurement of Fractionated Plasma Metanephrines Compared with the Combination of 24-hour Urinary Metanephrines and Catecholamines. J Clin Endocrinol Metab 88:553-558.
- Lenders JW, Pacak K, Walther MM, Linehan WM, Mannelli M, et al. (2002) Biochemical Diagnosis of Pheochromocytoma, Which test is best? JAMA 278:1427-1434.
- Sawka AM, Prebtani AP, Thabane L, Gafni A, Levine M, et al (2004) A systematic review of the literature examining the diagnostic efficacy of measurement of fractionated plasma free metanephrines in the biochemical diagnosis of Pheochromocytoma. BMC Endocrine Disorders 2004, 4:2.
- Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP (2007) Pheochromocytoma: Recommendations for Clinical Practice from the First International Symposium October 2005. Nat Clin Pract Endocrinol Metab 3:92-102.
- Grouzmann E, Drouard-Troalen L, Baudin E, Plouin PF, Muller B, et al. (2010) Diagnostic accuracy of free and total metanephrines in plasma and fractionated metanephrines in urine of patients with pheochromocytoma. Eur J Endocrinol 162:951-960.
- Sawka AM, Gafni A, Thabane L, Young Jr WF (2004) The Economic Implications of Three Biochemical Screening Algorithms for Pheocromocytoma. J Clin Endocrinol Metab 89:2859-2866.
- Lenders JW, Duh QY, Eisenhofer G, Gimenez-Roqueplo AP, Grebe SK, et al (2014) Pheochromocytoma and Paraganglioma: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 99:1915-1942.
- Amar L, Servais A, Gimenez-Roqueplo AP, Zinzindohoue F, Chatellier G (2005)Year of Diagnosis, Features at presentation, and Risk of Recurrence in Patients with Pheochromocytoma or Secreting Paraganglioma. J Clin Endocrinol Metab 90:2110-2116.
- Miskulin J, Shulkin BL, Doherty GM, Sisson JC, Burney RE, et al. (2003) Is Preoperative Iodine 123 Meta-iodobenzylguanidine Scintigraphy Routinely Necessary before Initial Adrenalectomy for Pheochromocytoma? Surgery 134:918-922.
- Mihai R, Gleeson F, Roskell D, Parker A, Sadler G (2008) Routine Preoperative (123) I- MIBG Scintigraphy for patients with Pheocromocytoma is not necessary. Langenbecks Arch Surg 393:725-727.
- Plouin, PF, Duclos JM, Soppelsa F, Boublil G, Chatellier G (2001) Factors Associated with Perioperative Morbidity and Mortality in Patients with Pheochromocytoma: Analysis of 165 Operations at a single Center. J Clin Endocrinol Metab 2001 86:1480-1486.
- Humphrey R, Gray D, Pautler S, Davies W (2008) Laparoscopic Compared with Open Adrenalectomy for resection of Pheocromocytoma: A Re- view of 47 cases. Can J Surg 51:276-280.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Karameh W (2023) Pheochromocytoma in Primary Care. J Palliat CareMed 13: 590. DOI: 10.4172/2165-7386.1000590
Copyright: © 2023 Karameh W. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 558
- [From(publication date): 0-2023 - Apr 25, 2025]
- Breakdown by view type
- HTML page views: 353
- PDF downloads: 205