Research Article Open Access
Pharmacological Interventions for Neuropathic Pain Associated with Compressive Myelopathy
Toshiya Tachibana*, Keishi Maruo, Fumihiro Arizumi, Kazuki Kusuyama, Kazuya Kishima and Shinichi Yoshiya
Department of Orthopaedic Surgery, Hyogo College of Medicine, Japan
- Corresponding Author:
- Toshiya Tachibana
Department of Orthopaedic
Surgery Hyogo College of Medicine
Nishinomiya, Hyogo-663-8501, Japan
Tel: +81-798-45-6452
Fax: +81-798-45-6453
E-mail: tachi@hyo-med.ac.jp
Received date: August 02, 2016; Accepted date: August 17, 2016; Published date: August 22, 2016
Citation: Tachibana T, Maruo K, Arizumi F, Kusuyama K, Kishima K, et al. (2016) Pharmacological Interventions for Neuropathic Pain Associated with Compressive Myelopathy. J Pain Relief 5:258. doi:10.4172/2167-0846.1000258
Copyright: © 2016 Tachibana T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pain & Relief
Abstract
Neuropathic pain following spinal cord injury (SCI) is a common problem in patients with SCI, which influences the quality of life of such patients. However, in our experiments of treatments for patients with compressive myelopathy, neuropathic pain was identified in patients with not only SCI, but also those with compressive myelopathy. The objective of this study was the evaluation of pharmacological interventions for neuropathic pain associated with compressive myelopathy (NePCM). Forty-five consecutive patients with NePCM who underwent pharmacological interventions from 2005 to 2016 were included in the study. Patient records were analyzed retrospectively. Evaluated factors were visual analog scale (VAS) and grid score (GS), which were used for quantification of pain. Effective pharmacological interventions were identified when VAS or GS decreased more than 10 points after treatments. The patients’ diagnoses were as follows: cervical or thoracic ossification of posterior longitude ligaments in 17 patients, cervical spondylotic myelopathy in 12 patients, disc herniation in 3 patients, and other diagnoses in 13 patients. All patients received decompression surgery with or without spinal fusion except 7 patients. Cervical lesions were in 32 patients, thoracic lesions were in 11 patients, and both cervical and thoracic lesions were in 2 patients. Pain distribution was at-level in 10 patients, below-level in 23 patients, and both at-level and below-level in 12 patients. Effective interventions were anticonvulsants for 19 patients, antidepressants for 10 patients, and other interventions for 3 patients. The effective anticonvulsants were pregabalin for 9 patients, gabapentin for 6 patients, and chronazepam for 5 patients. The effective antidepressants were duloxetine for 7 patients. However, 15 patients did not respond to any medications. Anticonvulsants and antidepressants are likely to be effective for NePCM, however, some patients do not respond to these interventions. Therefore, advanced treatments have to be developed for NePCM.
Keywords
Compressive myelopathy; Neuropathic pain; Pharmacological intervention
Introduction
Neuropathic pain following spinal cord injury (NePSCI) is a common problem in patients with spinal cord injury (SCI). Seventyfive percent of patients with SCI will experience NePSCI, and around one-half of these patients will have severe pain, which influences their quality of life [1]. However, in our experiments of treatments for patients with compressive myelopathy, neuropathic pain was not only identified in patients with SCI, but also patients with compressive myelopathy. These patients with neuropathic pain associated with compressive myelopathy (NePCM) had prolonged neuropathic pain even after decompression surgery and recovery of motor symptoms.
Moreover some patients had complained of new pain after operation. NePCM has not been well studied, nor has the treatment for it been established yet, and it is still a challenging issue. We have been trying to treat NePCM by pharmacological interventions such as anticonvulsants, antidepressants and opioids, which were recently adapted to neuropathic pain (NeP). The objective of this study was to evaluate of pharmacological interventions for NePCM.
Materials and Methods
Ethics committee approval was given for this study at our institution and written informed consent for participation, use of personal data and follow-up and was signed by all of the patients.
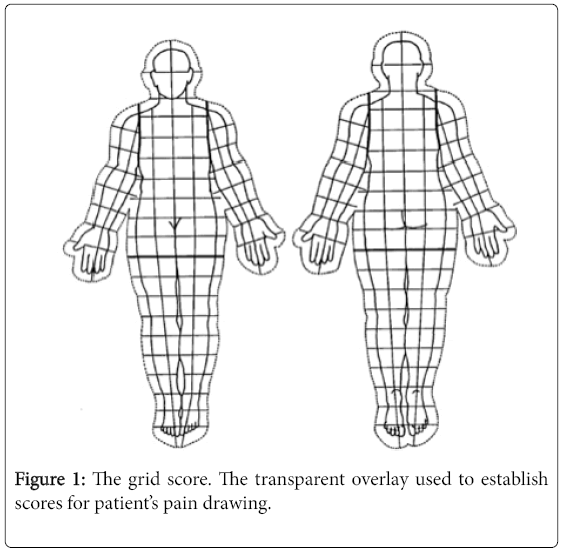
Forty-five consecutive patients with neuropathic pain and compressive myelopathy who underwent pharmacological interventions by the first author from 2005 to 2016 were included in the study. Patient records were analyzed retrospectively, and the evaluated factors were visual analog scale (VAS) and grid score (GS), which was used for quantification of pain drawing (PD) [2,3]. PD evaluations were performed before and during the course of the treatment for each patient. Nurses explained to patients how to draw a PD at our outpatient clinic each time. Patients were able to indicate where they feel pain by drawing on a whole-body figure. In order to quantitatively evaluate the severity of symptoms based on the PD results, GS was applied to the PD drawing (Figure 1) [2,3]. Boxes that are bilaterally symmetric and of approximately equal area cover the pain drawing, but also the quantitate pain extending outside the body allows for differentiation of localized mechanical and referred/ radicular pain patterns. There are a total numbers of boxes is 208. Pain distribution was classified using the neuropathic section of IASP classification of pain following SCI [4]. Effective pharmacological interventions were identified when VAS and/or GS decreased more than 10 points after treatments. In the statistical analysis, the student t-test was performed using Excel (Microsoft Corporation Redmond, WA, USA). A p-value of <0.05 was considered to indicate significance.
Results
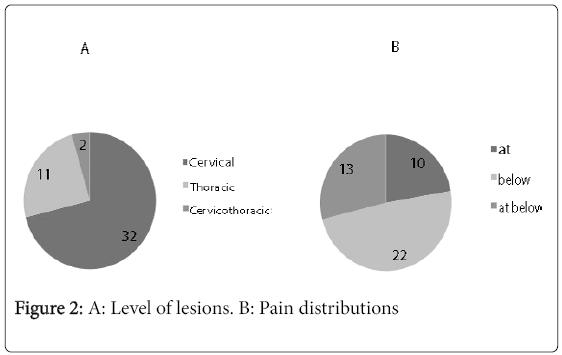
There were 27 male patients and 19 female patients. The mean age of patients was 67 years old (range, 42-89 years old). The mean followed-up period was 52.6 months (range, 6-144 months). The patients’ diagnoses were cervical or thoracic ossification of posterior longitude ligaments in 17 patients, cervical spondylotic myelopathy in 12 patients, disc herniation in 3 patients, and other diagnoses in 13 patients. All but 7 patients received decompression surgery with or without spinal fusion. Cervical lesions were in 32 patients, thoracic lesions were in 11 patients, and both cervical and thoracic lesions were in 2 patients (Figure 2A). Pain distribution was at-level in 10 patients, below-level in 22 patients, and both at-level and below level in 13 patients (Figure 2B).
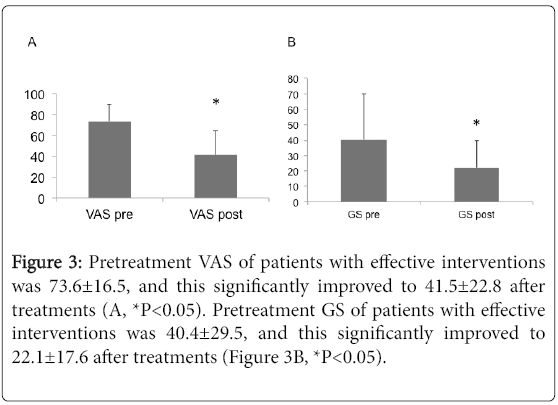
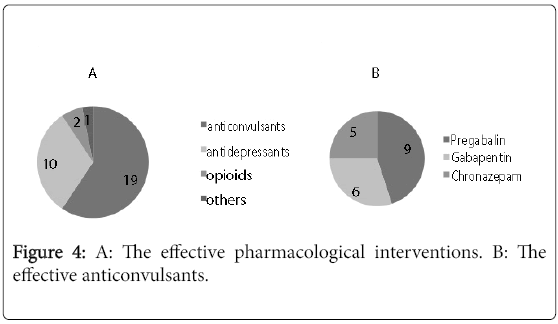
There were 30 patients who were responded to one or more interventions, however, 15 patients did not respond to any medications. In total, 31 effective responses of interventions were detected using VAS in 29 patients. Pretreatment VAS with effective interventions was 73.6±16.5, and this significantly improved to 41.5±22.8 after treatments (Figure 3A, P<0.05). In total, 10 effective responses of interventions were detected using GS in 9 patients. Pretreatment GS with effective interventions was 40.4±29.5, and this significantly improved to 22.1±17.6 after treatments (Figure 3B, P<0.05). Incidentally, 8 patients responded to both of VAS and GS. Effective interventions were anticonvulsants for 19 patients, antidepressants for 10 patients, opioids for 2 patients and others for 1 patient in total (Figure 4A). The effective anticonvulsants were pregabalin for 9 patients, gabapentin for 6 patients, and chronazepam for 5 patients in total (Figure 4B). The effective antidepressants were duloxetine for 7 patients and others for 3 patients in total. The effective opioid was tramadol-acetaminophen for 2 patients.
Figure 3: Pretreatment VAS of patients with effective interventions was 73.6±16.5, and this significantly improved to 41.5±22.8 after treatments (A, *P<0.05). Pretreatment GS of patients with effective interventions was 40.4±29.5, and this significantly improved to 22.1±17.6 after treatments (Figure 3B, *P<0.05).
Discussion
There have been many literatures for NePSCI in the last two decades [1,4-7], however, NePCM has not yet been studied. The current study may be the first paper to evaluate the pharmacological interventions for NePCM.
NePCM and NeSCI may have similar pathology as central NeP due to spinal cord lesions in spite of acute lesion or chronic lesion, respectively. It has been speculated that following SCI anatomical, neurochemical, inflammatory, excitotoxicity and physiological events in the injured spinal cord caused clinical and behavioral response involving allodynia, hyperalgesia and pain in NePSCI [5]. Pharmacological targets for NePSCI and NePCM may be suppressing hyper excitability of the neural circuit and recovery of the inhibitory system. Anticonvulsants are one type of drug targeting excitability of the neural circuit. On the other hand, antidepressants are drugs that target to the inhibitory system.
In the current study, anticonvulsants and antidepressants were mainly effective for NePCM. Gapapentin, one of the anticonvulsants has been proposed a first choice of drug for NePSCI [6]. Pregabalin, another type of anticonvulsant is more effective in reducing the duration-adjusted average change in pain as compared with the baseline in patients with SCI over a 16-week period when compared to the placebo in the RCT [7]. Both of gabapentin and pregabalin are ligands for alpha-2-delta-1 subunit of voltage-gated calcium channels. The importance of alpha-2-delta-1 subunit for peripheral NeP models has been stated previously [8-10]. Alpha-2-delta-1 subunit may also be involved in NePSCI because alpha-2-delta-1 subunit was up-regulated in the dorsal spinal cord after SCI [11]. The increase of alpha-2-delta-1 subunit in the dorsal spinal cord after SCI may be related to the effect of gabapentin and pregabalin on NePSCI and NePCM. Duloxetine, one type of antidepressant is a mixed serotonin and noradrenaline reuptake inhibitor. It has demonstrated efficacy in peripheral Nep and central NeP without significant postsynaptic effects [12-14]. The efficacy of duloxetine for NePCM may be involved in the inhibitory system.
The limitations of this preliminary study were the retrospective cross-sectional study design, and the small number size. Thus, the data were not robust enough to draw definite conclusions.
Conclusion
In conclusion, some pharmacological interventions involving anticonvulsants and antidepressants are likely to be effective for NePCM. However, some patients do not respond to these interventions. Therefore, advanced treatments have to be developed for NePCM.
References
- Siddall PJ, McClell JM, Rutkowski SB, Cousins MJ (2003) A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 103:249-257.
- Gatchel RJ, Mayer TG, Capra P, Diamond P, Barnett J (1986) Quantification of lumbar function part 6: the use of psychological measures in guiding physical function restoration. Spine 11:36-42.
- Tachibana T, Maruo K, Inoue S, Arizumi F, Kusuyama K, et al. (2016) Use of pain drawing as an assessment tool of sciatica for patients with single level lumbar disc herniation. Springerplus
- Siddall PJ (2009) Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord 47:352-359.
- Yezierski RP, Burchiel KJ (2002) Progress in pain research and management volume 23, Spinal cord injury pain: assessment, mechanisms, management, Seattle.
- Siddall PJ, Middleton JW (2006) A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord 44: 67-77.
- Cardenas DD, Nieshoff EC, Suda S, Sanin L, Goto S, et al. (2013) A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury. Neurology 80: 533-539
- Li CY, Song YH, Higuera ES, Luo D (2004) Spinal dorsal horn calcium channel alpha-2-delta-1 subunit upregulation contributes to peripheral nerve injury- induced tactile allodynia. J Neurosci 29: 8494-8499.
- Tanabe M, Takasu K, Takeuchi Y, Ono H (2008) Pain relief by gabapentin and pregabalin via supraspinal mechanisms after peripheral nerve injury. J Neurosci Res 86: 3258-3264.
- Patel R, Bauer CS, Nieto-Rostro M, Margas W, Ferron L, et al. (2013) Alpha-2-delta-1 gene deletion affects somatosensory neuron function and delays mechanical hypersensitivity in response to peripheral nerve damage. J Neueosci 33:16412-16426
- Borujerdi A, Zeng J, Sharp K, Kim D, Steward O, et al. (2011) Calcium channel alpha-2-delta-1 protein upregulation in dorsal spinal cord mediates spinal cord injury induced neuropathic pain states. Pain 152: 649-655.
- Finnerup NB, Sindrup SH, Jensen TS (2010) The evidence for pharmacological treatment of neuropathic pain. Pain 150: 573-581.
- Vranken JH, Hollmann MW, Vegt MH, Kruis MR, Heesen M, et al. (2011) Duloxetine in patients with central neuropathic pain caused by spinal cord injury or stroke: A randomized, double-blind, placebo-controlled trial. Pain 152: 267-273.
- Mehta S, Guy S, Lam T, Teasell R, Loh E (2015) Antidepressants Are Effective in Decreasing Neuropathic Pain After SCI: A Meta-Analysis. Top Spinal Cord InjRehabil 21:166-173.
Relevant Topics
- Acupuncture
- Acute Pain
- Analgesics
- Anesthesia
- Arthroscopy
- Chronic Back Pain
- Chronic Pain
- Hypnosis
- Low Back Pain
- Meditation
- Musculoskeletal pain
- Natural Pain Relievers
- Nociceptive Pain
- Opioid
- Orthopedics
- Pain and Mental Health
- Pain killer drugs
- Pain Mechanisms and Pathophysiology
- Pain Medication
- Pain Medicine
- Pain Relief and Traditional Medicine
- Pain Sensation
- Pain Tolerance
- Post-Operative Pain
- Reaction to Pain
Recommended Journals
Article Tools
Article Usage
- Total views: 10919
- [From(publication date):
September-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 10099
- PDF downloads : 820