Peri-operative Rectus Sheath Fentanyl-levobupivacaine Infusion vs. Thoracic Epidural Fentanyl Levobupvacaine Infusion in Patients Undergoing Major Abdominal Cancer Surgeries with Medline Incision
Received: 27-Apr-2018 / Accepted Date: 02-May-2018 / Published Date: 09-May-2018 DOI: 10.4172/2167-0846.1000318
Abstract
Background and Objectives: The gold standard for acute postoperative pain management in major abdominal surgeries is thoracic epidural analgesia (TEA) and this was proved by a lot of studies, systematic reviews and metaanalyses. However, TEA is sometimes contraindicated and may cause serious risks. Rectus Sheath Block (RSB) is effective for the abdominal surgeries with midline abdominal incisions as local anesthetics will be injected within the posterior rectus sheath bilaterally leading to intense pain relief for the middle anterior wall extending from the xiphoid process to the symphysis pubis. The aim of the study was to assess intra and post-operative RSB versus intra and post-operative TEA, in patients undergoing elective major abdominal cancer surgery with midline incisions.
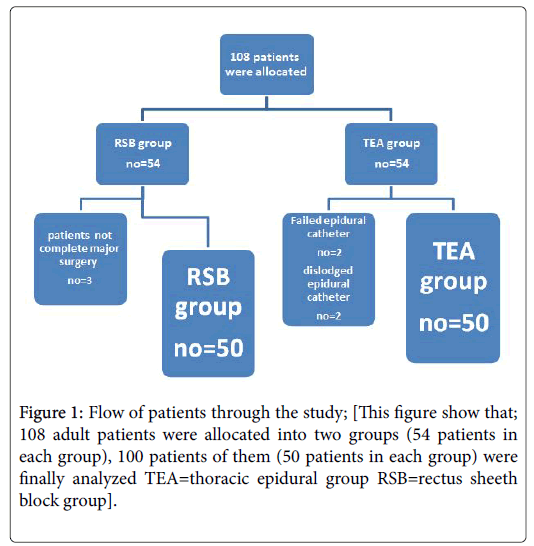
Methods: This randomized, blinded, was registered at www.clinicaltrials.gov at no.: “NCT03460561” and was approved by local ethics committee of South Egypt Cancer Institute, Assiut University, Egypt. One hundred adult patients, (ASA grade II and III), scheduled for major elective abdominal cancer surgery with Medline incision, were randomly divided into two groups, (50 patients each); TEA group: patients in this group received TEA with standard GA and intra-operative analgesia was started before skin incision by injecting epidural bolus dose of 0.1 ml/kg of (0.125% levo-bupivacaine+fentanyl 2 μg/ml). Postoperative analgesia was provided through PCEA by injecting a bolus dose of 3 ml then continuous infusion of 0.1 ml/kg of mixture of (0.0625% levo-bupivacaine+fentanyl 2 μg/ml) for 48 hours postoperative. RSB group: patients in this group received standard GA plus ultrasound (U/S) guided rectus sheath block by a volume of 20 mL of (0.25% levo-bupivacaine+fentanyl 30 μg) in saline on either side. Before end of surgery and before closure of abdominal wall, bilateral surgically placed catheters in rectus sheath plane aiming to provide post-operative analgesia using the following; 20 mL of (0.125% levo-bupivicaine+Fentanyl 30 μg) every 12 hours in to each catheter for 48 hours. Perioperative hemodynamics (MAP and HR) were recorded. Postoperative pain was assessed over 48 hour post operatively using (VAS). Total fentanyl consumption, Peak expiratory flow rate (PEFR), postoperative and side effects of the drugs and duration of ICU and hospital stay were recorded.
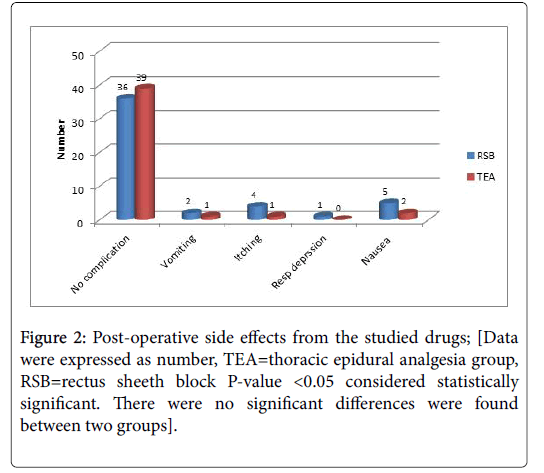
Results: We found a significant reduction in VAS pain scores (at rest and during cough) in both group at all postoperative period but fentanyl consumption was significantly lower in TEA group. Also we found a significant reduction in intra-operative hemodynamics (mean arterial pressure and heart rate) in TEA group in comparison to RSB group while there was minimal statistically significant reduction in postoperative MAP and heart rate. The incidence of other postoperative complications such as sedation, nausea and vomiting were comparable in both groups.
Conclusion: Rectus sheath block was not inferior to thoracic epidural analgesia in reduction of pain intensity after major abdominal cancer surgeries, and associated with hemodynamic stability along the 48 hours postoperative without procedure related adverse events or decreasing PEFR.
Keywords: Rectus sheath block; Thoracic epidural analgesia; VAS scale; Abdominal cancer surgeries
Introduction
Major upper abdominal cancer surgeries with midline incisions usually cause intense postoperative pain, and a significant component of this experienced severe pain is due to abdominal wall incision [1]. Treating of this pain lead to reduction of stress response, postoperative insulin resistance and allows early patients mobility, which itself is very important to decrease secondary complications such as chest infection and Deep Venous Thrombosis. This is an important goal of Enhanced Recovery Programmes (ERP) which aimed at reducing complications [2]. Thoracic epidural analgesia (TEA) is considered the gold standard method in major upper abdominal surgeries for postoperative analgesia, and this was proved by many studies, systematic reviews and meta-analyses which have concluded that TEA was associated with effective postoperative analgesia with better patients' outcomes and reduction of (ileus, systemic opiate requirements and pulmonary complications) [3-7].
However, TEA is sometimes contraindicated and leads to many serious risks as; motor block involving lower limbs preventing early mobilization of patient, high incidence of failure rate, premature catheter dislodgement and hypotension with risk of prolonged use of vasopressors [8]. Also TEA may cause rare but dangerous and critical neurologic complications such as; (hematoma, abscess and paraplegia) [9,10]. Several investigators explored other alternatives to reach the best choice for post-laparotomy analgesia avoid adverse effects related to TEA, decrease opioid requirements and allow patients to breathe and cough more comfortably [11,12]. The rectus sheath block (RSB) was performed first time in 1899 as an analgesic technique. Then, the block appears to decrease opioid requirements after laparotomy, by blocking ventral rami of the seventh to twelfth intercostal nerves, which supply the rectus abdominis muscle and overlying skin, are blocked [13,14].
RSB was used effectively for the abdominal surgeries with midline incisions as local anesthetics injected within the posterior rectus sheath bilaterally providing good analgesia for the middle anterior abdominal wall from the xiphoid process to the symphysis pubis [15,16]. But, RSB has no effects on visceral pain control, which may be experienced in the early postoperative 12-36 hours [15]. To improve the block duration or quality or both, many studies have shown that adjuvant like opioids (Fentanyl), has been used for regional nerve plexus blocks [17,18]. The value of u/s image guiding for rectus sheath block helps to reduce incidence of peritoneal or vital structures injury, and to facilitate correct needle position [19]. The aim of the study was to answer the question; does analgesic efficacy of intra and post-operative RSB-as safe alternative-comparable to intra and post-operative TEA in patients undergoing elective major abdominal cancer surgery with midline incisions?
Patients and Methods
This randomized, blinded, was registered at www.clinicaltrials.gov at no.: “NCT03460561” and was approved by local ethics committee of South Egypt Cancer Institute, Assiut University, Egypt. One hundred adult patients, (ASA grade II and III), scheduled for major elective abdominal cancer surgery with Medline incision, were consecutively enrolled. Patients who excluded from the study; who refused the study, Patients with active neurological disease, Patients with coagulopathy, cutaneous disorders at the epidural insertion site, and Patients allergic to the studied medications. All patients were evaluated by cardiologist and anesthesiologist for medical history, and physical fitness.
Oral ranitidine tablet, 50 mg and lorazepam tablet, 3 mg on the night of surgery were given to all patients as pre-operative medications. The day before surgery, patients of both group were taught how to evaluate their own pain intensity using the visual analog scale (VAS), scored from 0 to 10 (where 0=no pain and 10=worst pain imaginable) [20], and how to use the patient controlled analgesia (PCA) device (Abbott Laboratories, North Chicago, IL, USA). Patients were randomly assigned into two groups, (50 patients in each group), and method of randomization was as following; opaque sealed envelopes containing a computer generated randomization schedule; the opaque envelopes were sequentially numbered and were opened immediately before application of anesthetic plan.
TEA group (No.=50): Patients in this group received TEA with standard GA and intra-operative analgesia was started before skin incision by injecting epidural bolus dose of 0.1 ml/kg of (0.125% levobupivacaine+ fentanyl 2 μg/ml). Postoperative analgesia was provided by bolus dose of 3 ml then continuous infusion of 0.1 ml/kg of mixture of (0.0625% levo-bupivacaine+fentanyl 2 μg/ml) for 48 hours postoperative.
RSB group (No.=50): Patients in this group received standard GA plus ultrasound (U/S) guided rectus sheath block by a volume of 20 mL of (0.25% levo-bupivacaine+fentanyl 30 μg) on either side. Before end of surgery and before closure of abdominal wall, bilateral surgically placed catheters in rectus sheath plane aiming to provide postoperative analgesia using the following; 20 mL of (0.125% levobupivicaine +Fentanyl 30 μg) every 12 hours in to each catheter for 48 hours. Also we gave postoperative intravenous rescue analgesic Fentanyl (30 μg) that could be repeated every 10 minute) if visual analog pain scale (VAS) ≥ 4.
Standard general anesthesia
Preoxygenation for 3 min, then induction of anesthesia was done with IV propofol (2.5 mg/kg) plus 0.15 mg/kg Cisatracurium to facilitate Tracheal intubation and fentanyl 2 μg/kg. Anesthesia maintainance was done by; sevoflurane 1-1.5 minimum alveolar concentration (MAC) and cisatracurium 0.03 mg/kg when indicated. Patients were mechanically ventilated to maintain end tidal CO2 between 35 and 40 mmHg. The oxygen-air mixtures was used to keep inspired oxygen fraction (FIO2) 50% At the end of surgery, neuromuscular block was antagonized in all patients using neostigmine 0.05 mg/kg and atropine 0.02 mg/kg and the patients were extubated in the operating room. Hypotension was defined as systolic blood pressure <85 mmHg and was treated with IV fluid plus IV ephedrine 0.1 mg/kg. Bradycardia was defined as HR slower than 50 beats/min and was treated by atropine 0.01 mg/kg.
The technique of thoracic epidural
Thoracic epidural catheter was inserted, under complete aseptic precautions and before induction of GA, using a 17 gauge, Tuohy epidural needle by a midline approach. T9-T10 interspace was targeted for the injection after skin infiltration by 5 mL of lidocaine 1%. Using loss of resistance technique, the epidural space was identified then the catheter was introduced 2 cm into the epidural space, then epidural test dose of 3 mL of lidocaine 2% with 1:200,000 adrenaline was injected to exclude accidental vascular or subarachnoid position. Loading dose of 0.1 mL/kg of 0.125% bupivacaine+fentanyl 2 μg/mL to obtain T4 sensory level but if the injected dose was not enough to achieve T4 sensory level, another dose of 0.05 mL/kg was injected after 20 minutes.
Rectus sheath block technique
Just after induction of GA and before surgical incision, rectus sheath blocks (RSB) were performed (by one investigator to all patients) in the operative room. Emergency equipments to treat local anesthetic toxicity were available and under complete aseptic sterilization, the rectus muscle was imaged with the ultrasound probe, A broadband (5-12 MHz) linear array probe of Sonosite™ 3000 ultrasound (FUJIFILM, Sonosite EDGE II-UAS) in a transverse orientation immediately above the level of the umbilicus, with an imaging depth of 4-6 cm.
Then an 18G Tuohy needle was introduced few millimeters depth using an in plane technique in an angle of 45 degrees to the skin. The ultrasound images identify the rectus muscle and posterior rectus sheath with fascia transversalis as two hyperechoic railway-like lines. Then under direct vision, the needle was advanced to the desired position where 20 mL of (levo-bupivacaine 0.25% Fentanyl 30 μg) were injected causing hydro dissection of the rectus muscle away from the posterior rectus sheath. And the same technique was repeated on the opposite side.
Before closure of abdominal wall, an epidural catheter (Smithsmedical 16G epidural mini-pack) with multiple opening at the end of the tubing were inserted by surgeon as following; two catheters were placed at the superior end of the laparotomy wound. And the surgeon placed one hand inside the abdomen and the other hand used for insertion of the introducer needle. The surgeon felt when needle was in the interface between the peritoneum and muscle layer, and palpated the inferior epigastric artery to prevent its injury then he removed the stylet and the epidural catheter was advanced until a 5 cm length is in the peritoneum-muscle interface. The surgeon fixed the catheter and secured it at this point, to prevent accidentally pulled out.
Then a bacterial filter was connected and the catheter was flushed as to avoid its occlusion. The procedure was repeated on the contra lateral side. In PACU, we injected above mentioned local anesthetic mixture every 12 hours in to each catheter, and the catheters were examined every day for signs of infection or occlusion. All patients were followed up for 48 hours in PACU by the following parameters:
• Vital signs (MAP, HR) were recorded intra and post-operative 48 hours.
• VAS score (at rest and with cough) was recorded at 0,2,6,12,24,36 and 48 hours.
• Total intra and post-operative Fentanyl consumption.
• The Peak expiratory flow rate (PEFR) preoperatively, 12 and 24 hours postoperative.
• Any side effects as; nausea, vomiting, itching, respiratory depression (diagnosed as SPO2 less than 90%) or sedation by (sedation score).
• Interventional complications (dural puncture, hematoma, abscess or vital structure injury) were recorded.
• Duration of ICU and hospital stay.
Results
The study involved two groups of patients who underwent major abdominal cancer surgeries using midline incisions; the RSB Group (n=50) and the TEA Group (n=50) (Figure 1) illustrates the flow of the patients through the study. The demographic data and the patient's characteristics were similar between groups (Tables 1-4). We found a significant reduction in VAS pain scores (at rest and with cough) in both group at all measured time points (Tables 5-7) however, intra and post-operative fentanyl consumption were significantly decreased in TEA group (P-value 0.000**) (Table 8). Also there was a significant reduction in early intra and post-operative mean arterial pressure (MAP); and heart rate in TEA group in comparison to RSB group patients (Table 2 and 3) who had clinically important but not statistically significant reduction in postoperative PEFR (192.0 ± 28.0 versus 181.6 ± 31.7 L/min) (Table 4). The incidence of postoperative complications (nausea, itching and vomiting) was comparable in both groups (Figure 2) except sedation which was significantly increased in early post-operative RSB group (P-value 0.046*) (Table 7).
| RSB Group (n=50) | TEA Group (n=50) | p value | |
|---|---|---|---|
| Age (kg) | 56.6 ± 8.6 | 53.7 ± 11.6 | 0.322 |
| Sex (male/female) | 44/6 | 46/4 | 1 |
| Body Mass Index (kg/m2) | 27.8 ± 4.4 | 26.7 ± 5.0 | 0.439 |
| Duration of operation (min) | 162.4 ± 24.9 | 156.0 ± 27.1 | 0.389 |
| Type of Operation | |||
| Cystectomy | 24 (48.0%) | 32 (64.0%) | 0.634 |
| Colectomy | 18 (36.0%) | 14 (28.0%) | |
| Hysterectomy | 6 (12.0%) | 4 (8.0%) | |
| Anterior pelvic resection | 2 (4.0%) | 0 (0.0%) | |
Table 1: Demographic and baseline clinical characteristics of the two studied groups; [Data are expressed as (mean ± standard deviation, ratio and frequency (percentage) TEA=thoracic epidural group RSB=rectus sheeth block. P-value <0.05 considered statistically significant].
| MAP (mmhg) | RSB group (n=50) | TEA group (n=50) | P-value |
|---|---|---|---|
| Baseline reading | 77.9+10.6 (58-94) | 78.5+9.3 (68-95) | 0.117 |
| 1 hour | 82.47+10.04 (62-100) | 64.53+10.02 (56-90) | 0.002* |
| 2 hour | 79.67+12.12 (62-98) | 65.07+7 (52-77) | 0.001* |
| 3 hour | 73.73+11.79 (60-100) | 69.67+7.32 (60-82) | 0.12 |
| 4 hour | 77.2+13.43 (62-108) | 73.2+8.35 (59-86) | 0.218 |
| 5 hour | 73.13+8.86 (62-98) | 72.93+4.95 (65-82) | 0.914 |
| HR (bpm) | |||
| 0 hour | 74.8+11.0 (56-94) | 77.9+14.0 (57-97) | 0.326 |
| 1 hour | 84.13+10.37 (65-98) | 62.4+7.16 (65-89) | 0.001* |
| 2 hour | 81.93+18.02 (56-120) | 66.47+14.43 (57-110) | 0.016* |
| 3 hour | 83.27+13.96 (58-110) | 70.67+11.81 (56-108) | 0.012* |
| 4 hour | 79.07+14.14 (59-108) | 75.33+11.57 (50-98) | 0.161 |
| 5 hour | 73.93+12.34 (55-100) | 72.73+13.05 (55-100) | 0.952 |
Table 2: Intra-operative MAP and HR.
| RSB group (n=50) | TEA group (n=50) | P-value | |||
| Range | Mean+SD | Range | Mean+SD | ||
| Postoperative HR (bpm) | |||||
| Day 1 | 64.8-121.4 | 92.91+19.07 | 55-116.6 | 84.59+21.78 | 0.003* |
| Day 2 | 67.4-125.4 | 88.53+15.1 | 61.6-112 | 80.6+15.14 | 0.147 |
| Postoperative MAP (mmhg) | |||||
| Day 1 | 68.8-84.6 | 77.21+4.63 | 61.4-80.8 | 73.69+7.14 | 0.031* |
| Day 2 | 64.8-83.2 | 76.15+7.94 | 62.6-79.2 | 73.75+7.96 | 0.154 |
Table 3: Post-operative haemodynamic variables (mean of readings/ day).
| RSB Group (n=50) | TEA Group (n=50) | P value | |
|---|---|---|---|
| Preoperative | 210.0 ± 29.6 | 196.4 ± 33.4 | 0.031 |
| 12 hour Postoperative | 192.0 ± 28.0 | 181.6 ± 31.7 | |
| 24 hour Postoperative | 196.0 ± 28.0 | 184.6 ± 31.7 |
Table 4: The Peak expiratory flow rate preoperatively and 12 hours postoperative period in the two studied groups.
| VAS scores at rest | RSB Group (n=50) | TEA Group (n=50) | p value |
|---|---|---|---|
| 1 hour | 3 (1-4) | 2 (2-4) | 0.822 |
| 2 hour | 2 (1-3) | 2 (1-4) | 0.512 |
| 6 hour | 2 (1-3) | 1.5 (1-3) | 0.946 |
| 12 hour | 1 (1-2) | 1.5 (1-2) | 0.354 |
| 24 hour | 1 (1-2) | 1 (1-2) | 0.734 |
| 36 hour | 2.5 (2-3) | 2.2 (2:3) | 0.126 |
| 48 hour | 2 (2-3) | 2 (1:3) | 0.302 |
Table 5: Pain VAS scores at rest during the postoperative 2 days.
| VAS score with coughing | RSB Group (n=50) | TEA Group (n=50) | p value |
|---|---|---|---|
| 1 hour | 3 (2-5) | 3 (2-4) | 0.854 |
| 2 hours | 3 (2-4) | 2.5 (1-4) | 0.251 |
| 6 hours | 3 (2-4) | 2.5 (1-4) | 0.465 |
| 12 hours | 2.5 (1-4) | 2 (1-4) | 0. 735 |
| 24 hours | 2.4 (1-4) | 2 (1-4) | 0.693 |
| 36 hours | 2 (1:3) | 1 (1:1) | 0.194 |
| 48 hours | 2 (2:2) | 2(1:3) | 0.157 |
Table 6: Pain VAS score with coughing during the postoperative 2 days.
| Post-op. sedation score | RSB group(n=50) | TEA group (n=50) | P-value | ||
| Range | Mean+SD | Range | Mean+SD | ||
| 0 hour | 01-02 | 2 | 01-01 | 1 | 0.01* |
| 4 hour | 01-03 | 2 | 01-01 | 1 | 0.01* |
| 8 hour | 01-03 | 2 | 01-01 | 1 | 0.046* |
| 12 hour | 01-02 | 1 | 01-01 | 1 | 0.943 |
| 16 hour | 01-01 | 1 | 01-01 | 1 | 0.948 |
| 20 hour | 01-01 | 1 | 01-01 | 1 | 0.943 |
| 24 hour | 01-01 | 1 | 01-01 | 1 | 0.956 |
Table 7: Post-operative sedation score.
| RSB group (n=50) | TEA group (n=50) | P-value | |||
| Range | Mean+SD | Range | Mean+SD | ||
| ICU stay (day) | 2-7 | 4.47 ± 2.16 | 02-06 | 3.8 ± 1.57 | 0.115 |
| Hospital stay (day) | 3-12 | 8.13 ± 7.62 | 04-11 | 7.13 ± 4.12 | 0.209 |
| Fentanyl (mic/24 hour) consumption | 600-900 | 725.6 ± 234.5 | 200-320 | 225.3 ± 122.43 | 0.000** |
Table 8: ICU, Hospital stay and total (intra and post-operative) fentanyl consumption.
Data are expressed as mean ± SD. At base line reading and 1, 2, 3, 4 and 5 hours MAP= mean arterial pressure (mmhg), HR=heart rate (beat per minutes), h=hour interval 0h=Baseline reading TEA=thoracic epidural group RSB=rectus sheeth block P-value <0.05 considered statistically significant. There was significant difference in early post-operative periods being decreased in TEA group in comparison to control group.
Data are expressed as mean ± SD, HR=heart rate (beat per minutes), TEA=thoracic epidural group. MAP=mean arterial pressure (mmhg), TEA=thoracic epidural group RSB=rectus sheeth block between two groups there was only significant difference in early post-operative day regarding patient's H.R and MAP. P-value <0.05 considered statistically significant.
Data are expressed as mean ± standard deviation TEA=thoracic epidural group RSB=rectus sheeth block Peak expiratory flow rate (PEFR) was assessed preoperatively and then 12 and 24 hours postoperatively. Using ANOVA for repeated measures, (p <0.001). The two groups had the almost same effect on PEFR, however, it was clinically but not significantly higher in RSB Group (p=0.031).
Data are expressed as median (range) TEA =thoracic epidural group RSB=rectus sheeth block VAS=visual analogue scale, h=hour. P-value <0.05 considered statistically significant.
Data are expressed as median (range) TEA=thoracic epidural group RSB=rectus sheeth block, VAS=visual analogue scale, h=hour, P-value <0.05 considered statistically significant. Data are expressed as mean ± SD TEA =thoracic epidural analgesia group. RSB=rectus sheeth block, h=hour 0h=immediately after recovery. In RSB group sedation was significant in early post-operative hours P-value <0.05 considered statistically significant.
Data are expressed as mean ± SD, TEA=thoracic epidural analgesia group, RSB=rectus sheeth block, P-value <0.05 considered statistically significant. There was a difference between two groups. Patients of TEA group stay less period in ICU and hospital and consumed less fentanyl.
Discussion
This study showed that both TEA and RSA provided effective of postoperative pain control during the 48 hours with insignificant effects on PEFR and hemodynamics. However, TEA had a better opioid sparing effect than RSA, as proved by much lesser postoperative fentanyl consumption, less ICU stay and hospital stay. With exception of sedation scores which were high in the (RSA) group at the first 12 hours postoperatively in comparison to the TEA group, reflecting the increased fentanyl consumption, there were no interventional complications recorded during the study period. Anesthesia has evolved as an essential three element (pre, intra and postoperative) patient care, and pain management, has become a major quality of life issue [21]. Since the pain inhibitory system was discovered and modulated by neurotransmitters like endorphins, serotonin and others, there were possibilities of using substances that imitate the action of these inhibitory neurotransmitters in the epidural or subarachnoid spaces as means for decreasing acute postoperative pain [22].
The main analgesic regimens used for major abdominal surgery are patient-controlled epidural analgesia (PCEA) or intravenous patient controlled analgesia (IVPCA) with a combination of opiods and local anesthetic drugs with or without intravenous non-steroidal antiinflammatory drugs (NSAID) or paracetamol [23]. TEA is in routine use in the Egyptian Cancer Institutes in anesthetic management of cancer patients [24] and their risks and benefits are well described and proved and as mentioned above; and many studies concluded that TEA is the gold standard method of post-operative pain control [25,26], therefore this study does not confer any additional risk to trial patients but to investigate if RSB is as effective and safe as TEA or inferior to it. But important limitation of analgesic choice in these cases is contraindications to neuroaxial block as risk of sepsis, immune suppression or coagulopathy that may necessitate avoiding an epidural block for analgesia. These problems are especially common in developing countries [27].
And IV opioids may not be particularly effective in controlling postoperative pain as they provide an initial analgesic effect but subsequently because rapid development of tolerance [21] and it prolongs duration of hospital stay due to dose-related side effects such as postoperative nausea and vomiting (PONV), respiratory depression, over sedation, urinary retention, and ileus [28]. For these reasons, we are concerned with the search for the best analgesic modality to be used in vulnerable cancer patients requiring major surgery associated with hemodynamic instability, excessive blood loss with the least possible side effects that encourage early postoperative mobility. Enhanced recovery after cancer surgery should be the main goal in such vulnerable group.
The regional blocks (as RSB) have been proved to provide effective postoperative analgesia. Furthermore, they were safe and avoid the risk for potentially devastating complications of EA and to decrease systemic analgesic side effects [29,30]. An effective epidural provide effective analgesia after abdominal surgery, while rectus sheath block may spare some visceral pain which is usually minimal by 24 hours post-operative [31]. This fact was proved by the study of Smith and their colleagues who concluded that the RSB was more effective in diagnostic laparoscopy than laparoscopic sterilization because women who performed sterilization experienced a pelvic visceral pain [32].
Visceral pain in this study was almost controlled, we can explain this control because of fentanyl which used with levo-bupivacaine in our study aiming to prolong the duration of sensory and motor blockade as proved by many studies [33,34]. the mechanism of this decrease probably by directly binding with opioid binding sites on the dorsal nerve roots aided with these axonal transport or by diffusing into surrounding tissues and subsequently into the epidural and subarachnoid spaces, it may also have been central opioid receptor mediated after systemic absorption of fentanyl [35,36]. Adding of Fentanyl as adjuvant opioid to levo-bupivacaine encouraged us to use the more diluted 0.125% concentrations.
RSB has been studied many surgeries, as umbilical and incisional hernia repair in children, cesarean section (when midline incision is used), and laparoscopy and proved to be effective [30,37]. The rectus sheath block aims to block the terminal branches of T6-L1 nerves by injecting local anaesthetics within the posterior rectus sheath bilaterally providing intense analgesia over the middle anterior wall from the xiphoid process to the symphysis pubis [38]. Confirming us Hamill et al. who investigated the effect of rectus sheath block on pain after laparoscopic appendectomy for acute appendicitis in children aged 8-14 years. In this group RSB reduced early post-operative pain. Authors recommended its use as a part of multimodal recovery program [39].
In the current study we used a single intraoperatve shot then continuous post-operative RSB via catheters infusion. As a single bolus of local anesthetic has a maximum duration of 12 hours. So, the comparison period between the two groups extended to the 48 postoperative hours [40]. Confirming us, more recent retrospective case review was done to report on the safety and efficacy of rectus sheath blocks, using bilateral rectus sheath catheters (RSCs), in 200 patients undergoing major open urological surgery. Operations included radical retropubic prostatectomy and radical cystectomy. All RSCs were successfully placed without complications. Low overall pain scores were reported [41].
In accordance with us, another study, which concluded that; RSB provide equivalent analgesia to EPB and avoid the recognized potential complications of EPB after colorectal surgery. RSB is associated with a shorter time to mobilization. This study involved 95 patients undergoing elective open or laparoscopic-converted-to-open colorectal resection for both benign and malignant disease [42]. But against us, an early study which studied the efficacy of intermittent injection of local anesthetics into rectus sheath space on postoperative opioid requirement, pain score and peak expiratory flow rate. In this study, patients who undergoing midline laparotomy received either bupivacaine 0.25% or normal saline using surgically placed catheters in the rectus sheath for 48 hours postoperative. And the results were, no statistically significant differences in postoperative opioid requirement, pain score or PEFR were noticed between two groups [30].
Of course, abdominal incisions is important reason that cause marked reduction in lung volume this is explained by spasm of the anterior abdominal wall muscles, splinting of the diaphragm and absence of deep breaths and sighs. The current study showed a reduction in PEFR in the first 12 h after surgery but the reduction was less pronounced using RSB compared to TEA. This is explained by less peritoneal irritation of the under-surface of the diaphragm and limitation of excursion in patients who receive RSB [43]. In addition, cancer patients constitute a vulnerable group. Elderly patients will increasingly make up the population of patients with cancer. Currently 60% of all malignancies, and 70% of all cancer deaths, occur in people over the age of 65. These patients may have problems in activities of daily living, COPD and medications for medical co-morbidities [44].
When compared with other regional block, a recent prospective, observer-blinded, randomized clinical study was done to evaluate the efficacy of US-guided RSB and transversus abdominis plane (TAP) blocks. The study involved 40 patients undergoing elective liver resection or Whipple procedure. RSB in combination with TAP block was associated with significantly decreased intraoperative fentanyl consumption, significantly lesser morphine boluses in PACU and significantly lower cumulative 24 hour postoperative morphine dosage [45]. Another subsequent study confirmed more effectiveness of administration of bupivacaine following midline laparotomy when placed in the rectus sheath compared with suprafascial delivery. Pain was less intense and morphine consumption decreases with intrafasical bupivacaine infusion [46].
A positive development is the advent of ultrasound use in anesthesia, which has made a variety of regional anesthesia blocks possible that may offer technically simple, safe and better alternative analgesic regimen or adjuncts [47]. It was noticed that the learning skills for the performing of RSCs are increasing in steep manner, particularly in those who previously experienced in ultrasonographyguided regional blocks and the rate of successful RSB is high with ultrasound guidance. The large size of the rectus muscle made RSB an easy technique to master [14]. This is confirmed by a RCT which compared the percentage of success and performance of inexperience trainees using ultrasound versus loss-of-resistance (LOR) technique, it was observed that the needle was placed in the correct targeted plane twice as often using ultrasound but in 21% of the LOR technique, the needle was placed intraperitoneal [48].
And surgical placement of RSCs, either blindly or with dissection, is a good alternative technique; but, some authors disagree with us and concluded that; the surgically placed RSCs were associated with more problems such as blockage or early removal. Also was also noted that patients required a greater amount of rescue analgesia [49]. We can conclude that rectus sheath block is almost effective as TEA in reduction of pain intensity at rest and with coughing following major abdominal operations in cancer patients without decrease of PEFR and addition of fentanyl to levo-bupivacaine as adjuvant may prolong the duration of sensory block. Also Rectus sheath block is associated with hemodynamic stability along the 48 hours postoperative with no drugor procedure-related adverse events. So RSB could be used as an effective alternative to TEA in patients undergoing laparotomies with a midline incision especially when TEA is contraindicated.
Study Limitations
Our study has many limitations. First, a continuous infusion was not considered in the RSB group. Otherwise, intermittent 12 hours’ interval injection was used, meanwhile an uninterrupted epidural infusion used for the TEA group. Second, the study was not double blind. Third, we did not appraise the level of the sensory block in RSA group patients after catheters insertion. Finally, we should include patients with ASA physical status classes >III.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- Rozen WM, Tran TM, Ashton MW, Barrington MJ, Ivanusic JJ, et al. (2008) Refining the course of the thoracolumbar nerves: A new understanding of the innervation of the anterior abdominal wall. Clin Anat 21: 325-333.
- Gustafsson UO, Scott MJ, Schwenk W, Demartines N, Roulin D, et al. (2013) Guidelines for perioperative care in elective colonic surgery: Enhanced recovery after surgery (ERAS) Society Recommendations. World J Surg 37: 259-284.
- Cook TM, Eaton JM, Goodwin AP (1997) Epidural analgesia following upper abdominal surgery: United Kingdom practice. Acta Anaesthesiol Scand 41: 18-24.
- Wheatley RG, Schug SA, Watson D (2001) Safety and efficacy of postoperative epidural analgesia. Br J Anaesth 87: 47-61.
- Peyton PJ, Myles PS, Silbert BS, Rigg JA, Jamrozik K, et al. (2003) Perioperative epidural analgesia and outcome after major abdominal surgery in high-risk patients. Anesth Analg 96: 548-554.
- Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA Jr, et al. (2003) Efficacy of postoperative epidural analgesia: A meta-analysis. JAMA 290: 2455-2463.
- Werawatganon T, Charuluxananan S (2005) Patient controlled intravenous opioid analgesia versus continuous epidural analgesia for pain after intra-abdominal surgery. Cochrane Database Syst Rev.
- Bonnet F, Marret E (2005) Influence of anaesthetic and analgesic techniques on outcome after surgery. Br J Anaesth 95: 52-58.
- Sugimoto M, Nesbit L, Barton JG, Traverso LW (2015) Epidural anesthesia dysfunction is associated with postoperative complications after pancreatectomy. J Hepatobiliary Pancreat Sci 23: 102-109.
- Freise H, Van Aken HK (2011) Risks and benefits of thoracic epidural anaesthesia. Br J Anaesth 107: 859-868.
- Pöpping DM, Zahn PK, Van Aken HK (2008) Effectiveness and safety of postoperative pain management: A survey of 18925 consecutive patients between 1998 and 2006 (2nd revision): A database analysis of prospectively raised data. Br J Anaesth 101: 832-840.
- Charlton S, Cyna AM, Middleton P, Griffiths JD (2010) Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database Syst Rev 12.
- Webster K (2010) Ultrasound guided rectus sheath block analgesia for abdominal surgery. Update Anaesth 26: 12-17.
- Sandeman DJ, Dilley AV (2008) Ultrasound-guided rectus sheath block and catheter placement. ANZ J Surg 78: 621-623.
- Cuneyitoglu S, Turktan M, Biricik E, Ozcengiz D (2015) Ultrasound-guided rectus sheath block in gynaecological surgery with pfannenstiel incision. Turk J Anaesthesiol Reanim 43: 318-322.
- Kim JS, Choi JB, Lee SY, Kim WH, Baek NH, et al. (2016) Pain related to robotic cholecystectomy with lower abdominal ports: effect of the bilateral ultrasound-guided split injection technique of rectus sheath block in female patients: A prospective randomised trial. Medicine (Baltimore) 95: 4445.
- Fletcher D, Kuhlman G, Samii K (1994) Addition of fentanyl to 1.5% lidocaine does not increase the success of axillary plexusblock. Reg Anesth 19: 183-188.
- Gissen AJ, Gugino LD, Datta S, Miller J, Covino BG (1987) Effects of fentanyl and sufentanil on peripheral mammalian nerves. Anesth Analg 66: 1272-1276.
- Abrahams MS, Horn JL, Noles LM, Aziz MF (2010) Evidence-based medicine: Ultrasound guidance for truncal blocks. Reg Anesth Pain Med 35: S36-42.
- McCormack HM, Horne DJ, Sheather S (1988) Clinical applications of visual analogue scales: A critical review. Psychol Med 18: 1007-1019.
- Hudcova J, Mc Nicol E, Quah C (2006) Patient controlled opioids analgesia versus conventional opioid analgesia for postoperative pain. Cochrane Database Syst Rev.
- Finnerty O, Carney J, McDonnell JG (2010) Trunk blocks for abdominal surgery. Anaesthesia 1: 76-83.
- Liu SS, Carpenter RL, Mackey DC, Thirlby RC, Rupp SM, et al. (1995) Effects of perioperative analgesic technique on rate of recovery after colon surgery. Anesthesiology 83: 757-765.
- Farouk MM, Mohammad MA (2017) Thoracic epidural analgesia reduces myocardial injury in ischemic patients undergoing major abdominal cancer surgery. J Pain Res 10: 887-895.
- Rigg JR, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, et al. (2002) Epidural anaesthesia and analgesia and outcome of major surgery: A randomised trial. Lancet 359: 1276-1282.
- Wu CL, Murphy JD (2014) Epidural anesthesia analgesia and patient outcomes: A perspective. Adv Anesthesiol.
- Cook TM, Counsel D, Wildsmith JAW (2009) Major complications of central neuraxial block: Report on the 3rd National Audit Project of the Royal College of Anaesthetists. Br J Anaesth 102: 179-190.
- Imani F (2011) Postoperative pain management. Anesthesiol pain Med 1: 6-7.
- Crosbie EJ, Massiah NS, Achiampong JY, Dolling S, Slade RJ (2012) The surgical rectus sheath block for post-operative analgesia: A modern approach to an established technique. Eur J Obstet Gynecol Reprod Biol 160: 196-200.
- Wilkinson KM (2014) Thoracic epidural analgesia versus rectus sheath catheters for open midline incisions in major abdominal surgery within an enhanced recovery programme (TERSC): Study protocol for a randomised controlled trial. Trials 15: 400.
- Padmanabhan J, Rohatgi A, Niaz A, Chojnowska E, Baig K, et al. (2007) Does rectus sheath infusion of bupivacaine reduce postoperative opioid requirement? Ann R Coll Surg Engl 89: 229-232.
- Smith BE, Suchak M, Siggins D, Challands J (1988) Rectus sheath block for diagnostic laparoscopy. Anaesthesia 43: 947-948.
- Nishikawa K, Kanaya N, Nakayama M, Igarashi M, Tsunoda K, et al. (2000) Fentanyl improves analgesia but prolongs the onset of axillary brachial plexus block by peripheral mechanism. Anesth Analg 91: 384-387.
- Nehra P, Oza V, Parmar V, Fumakiya P (2017) Effect of addition of fentanyl and clonidine to local anesthetic solution in peribulbar block. J Pharmacol Pharmacother 8: 3-7.
- Stein C, Lang LJ (2009) Peripheral mechanisms of opioid analgesia. Curr Opin Pharmacol 9: 3-8.
- Sehgal N, Smith HS, Manchikanti L (2011) Peripherally acting opioids and clinical implications for pain control. Pain Physician 14: 249-258.
- Gurnaney HG, Maxwell LG, Kraemer FW, Goebel T, Nance ML, et al. (2011) Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br J Anaesth 107: 790-795.
- Cowlishaw PJ, Scott DM, Barrington MJ (2012) The role of regional anaesthesia techniques in the management of acute pain. Anaesth Intensive Care 40: 33-45.
- Hamill JK, Liley A, Hill AG (2015) Rectus sheath block for laparoscopic appendicectomy: A randomized clinical trial. ANZ J Surg 85: 951-956.
- Cornish P, Deacon A (2007) Rectus sheath catheters for continuous analgesia after upper abdominal surgery. ANZ J Surg 77: 84.
- Wuethrich PY, HsuSchmitz SF, Kessler TM (2010) Potential influence of the anesthetic technique used during open radical prostatectomy on prostate cancer-related outcome: A retrospective study. Anesthesiology 113: 570-576.
- Tudor EC, Yang W, Brown R, Mackey PM (2015) Rectus sheath catheters provide equivalent analgesia to epidurals following laparotomy for colorectal surgery. Ann R Coll Surg Engl 97: 530-533.
- Extermann M (2003) Studies of comprehensive geriatric assessment in patients with cancer. Cancer Control 10: 463-468.
- American cancer society (2003) Cancer facts and figures 2003. GA: American Cancer Society, Atlanta.
- Abdelsalam K, Mohamdin OW (2016) Ultrasound-guided rectus sheath and transversus abdominis plane blocks for perioperative analgesia in upper abdominal surgery: A randomized controlled study. Saudi J Anaesth 10: 25-28.
- Khorgami Z, Shoar S, HosseiniAraghi N, Mollahosseini F, Nasiri S, et al. (2013) Randomized clinical trial of subcutaneous versus interfascial bupivacaine for pain control after midline laparotomy. Br J Surg 100: 743-748.
- Neal JM, Brull R, Chan VW, Grant SA, Horn JL, et al. (2010) The ASRA evidence-based medicine assessment of ultrasound-guided regional anesthesia and pain medicine: Executive summary. Reg Anesth Pain Med 35: S1-9.
- Dolan J, Lucie P, Geary T, Smith M, Kenny GN (2009) The rectus sheath block: accuracy of local anesthetic placement by trainee anesthesiologists using loss of resistance or ultrasound guidance. Reg Anesth Pain Med 34: 247-250.
- Parsons BA, Aning J, Daugherty MO, McGrath JS (2011) The use of rectus sheath catheters as an analgesic technique for patients undergoing radical cystectomy. Br J Med Surg Urol 4: 24-30.
Citation: Turky DAEM, Ibrahim IAR, Elzohry AAM (2018) Peri-operative Rectus Sheath Fentanyl-levo Bupivacaine Infusion vs. Thoracic Epidural Fentanyl-levo Bupivacaine Infusion in Patients Undergoing Major Abdominal Cancer Surgeries with Medline Incision. J Pain Relief 7:318. DOI: 10.4172/2167-0846.1000318
Copyright: © 2018 Turky DAEM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5330
- [From(publication date): 0-2018 - Dec 22, 2024]
- Breakdown by view type
- HTML page views: 4591
- PDF downloads: 739