Research Article Open Access
Periodontal Disease and Preterm Birth, is There any Relationship?
Nadia I Kawar1*, Elham Partovi2, Charles Hildebolt3, Dwight McLeod4 and Douglas D Miley51Department of Periodontics, University of Illinois, USA.
2Private Practice, Los Angelos, USA.
3Department of Radiology, Washington University, USA.
4Department of Periodontics, Southern Illinois University, USA.
5Department of Periodontics, Saint Louis University, USA.
- *Corresponding Author:
- Nadia Kawar
801 S Paulina St
Chicago IL 60612, USA
Tel: 312-355-1722
Fax: 312-996-0943
E-mail: kawarnad@uic.edu
Received Date: June 02, 2016; Accepted Date: July 05, 2016; Published Date: July 13, 2016
Citation: Kawar NI, Partovi E, Hildebolt C, McLeod D, Miley DD (2016) Periodontal Disease and Preterm Birth, is There any Relationship? J Interdiscipl Med Dent Sci 4:202. doi:10.4172/2376-032X.1000202
Copyright: © 2016 Kawar NI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Aim: Prematurity and low birth weight are major causes of neonatal morbidity, mortality and long-term disability. The purpose of this study was to determine if an association exists between periodontal disease and preterm birth (PT).
Material and methods: 59 females from the delivery ward at St. Mary’s Health Center, St. Louis, MO. Group I had 29 women who had Preterm birth (PT). Group II had 30 women whose babies were born full term (T). Full-mouth periodontal examination performed. Data collected about risk factors: race, maternal age, pregnancy complications; infections/inflammation; number of previous pregnancies and chemical abuse. Mothers were considered to have moderate to severe periodontal disease if ≥ 10% of sites measured ≥ 5 mm probing depth. Nominal logistic regression analysis used to calculate the odds of having a preterm birth infant having moderate to severe periodontal disease while adjusting for other risk factors.
Results: After adjustment for smoking, preeclampsia, and infections/inflammation other than periodontitis, a statistically significant association was found between PT and moderate to severe periodontitis (odds ratio = 5.8, 95% CI = 1.2-37.5, p = 0.04).
Conclusion: Moderate to severe periodontal disease may be an independent risk factor for preterm birth.
Abstract
Aim: Prematurity and low birth weight are major causes of neonatal morbidity, mortality and long-term disability. The purpose of this study was to determine if an association exists between periodontal disease and preterm birth (PT).
Material and methods: 59 females from the delivery ward at St. Mary’s Health Center, St. Louis, MO. Group I had 29 women who had Preterm birth (PT). Group II had 30 women whose babies were born full term (T). Full-mouth periodontal examination performed. Data collected about risk factors: race, maternal age, pregnancy complications; infections/inflammation; number of previous pregnancies and chemical abuse. Mothers were considered to have moderate to severe periodontal disease if ≥ 10% of sites measured ≥ 5 mm probing depth. Nominal logistic regression analysis used to calculate the odds of having a preterm birth infant having moderate to severe periodontal disease while adjusting for other risk factors.
Results: After adjustment for smoking, preeclampsia, and infections/inflammation other than periodontitis, a statistically significant association was found between PT and moderate to severe periodontitis (odds ratio = 5.8, 95% CI = 1.2-37.5, p = 0.04).
Conclusion: Moderate to severe periodontal disease may be an independent risk factor for preterm birth.
Keywords
Oral health; Systemic disease; Periodontitis; Preterm birth
Introduction
Preterm birth is the greatest contributor to infant death and longterm neurological morbidity [1]. Despite all the medical efforts to reduce the preterm birth, the rate is still high relatively high; according to the Centers for Disease Control and Prevention, preterm birth affected about 1 of every 10 infants born in the United States in 2014. Prevention and treating the underlying causes of preterm labor would be more successful than treating existing preterm labor [2]. Maternal infections are responsible for between 30%-50% of preterm births [3]. Remote subclinical infections have also been considered as causes of preterm labor [1]. Periodontal disease being an inflammatory disease triggered by microbial biofilm has been identified as a risk factor for preterm birth [4-6]. The purpose of this study is to determine if a relationship exists between periodontal disease and preterm birth.
Material and Methods
Patient selection
This is a Case-Control study was conducted at St Mary’s Health Center in St Louis Missouri in 2005. A convenience sample of 70 postpartum women were asked to participate in the study. Selection criteria were: 1) Hospital stay within three days postpartum 2) 18 years of age or older 3) No postpartum complications. Exclusion criteria were: 1) Requiring prophylactic antibiotics before periodontal examination 2) Bleeding tendency 3) Immune-compromised patients 4) Acute infections or chronic inflammatory diseases that directly caused preterm labor 5) Inability to comprehend and sign the informed consent written in English 6) Multiple gestation. Institutional Board Review approvals were obtained from Saint Louis University and Southern Illinois University, Informed consents were signed by participating patients.
Interview and questionnaire
The purpose of the study, risks, benefits and alternatives were discussed with each participant prior to the examination. A medical history was obtained from each subject and verified from the subject’s hospital record, if necessary. Data collected were: 1) Baby’s gestational age at delivery 2) Baby’s weight 3) Race 4) Maternal age 5) smoking 6) Pregnancy complications 7) Current infections and/or inflammation 8) Number of previous pregnancies 9) Chemical substance.
Examination procedure
The examination was performed while the patient in a semireclined position in a hospital bed or a rocking chair. A built-in examination light in each room was used in addition to room light. All present teeth were included except for inaccessible third molars. Teeth with potential source of infection besides periodontal disease were also identified such as large cavities, remaining roots, or purulent exudates. Measured parameters were: 1) Probing depths (PD) 2) Bleeding on probing (BOP) marked as present or absent. PD and BOP measured at six sites of each tooth which were distobuccal, buccal, mesiobuccal, distolingual, lingual and mesiolingual 3) Mobility of each tooth 4) Clinical attachment level (CAL) was estimated by measuring the distance between the cementoenamel junction (CEJ) and the gingival margin at two sites, buccal and lingual 5) Plaque marked as present or absent on two surfaces per tooth, buccal and lingual 6) Calculus marked as present or absent on two surfaces one on the buccal and one on the lingual surface of each tooth 7) Teeth with large cavities, remaining roots, purulent exudates were also marked. The examination instruments used were sterile disposable plastic mirrors, UNC-15 periodontal probes, and sterile gauze. Universal precautions and infection control measures were applied by the examiner and assistant recording the findings. Examinations were performed by one examiner who was not blinded to the pregnancy outcome. The timeline for the total encounter with the subject ranged between 20-30 minutes.
Subject education
All subjects were informed about their dental needs, based on the limited finding of this clinical examinations. Oral hygiene instructions were given and each subject was given an oral hygiene kit as a compensation for their participation supplied by Saint Louis University Graduate Periodontal program.
Study design
This a retrospective case-control study. Test cases were defined as subjects who delivered their babies before completion of 37 weeks of gestation, referred to as Preterm Birth (PT Group). Control were subjects delivered their babies after 37 weeks of gestation, referred to as Term Birth (T Group).
Statistical analysis
Age distributions in the two groups were tested for normality with Shapiro-Wilk W tests and equality of variances were tested for equality with O’Brien, Brown-Forsythe, Levene, and Bartlett tests. Age was also dichotomized for risk of PT, with women older than 34 years being considered at risk. This association was tested for significance with a Fisher’s exact test. Race distributions between the two groups were tested for significant differences with a Fisher’s exact test. Smoking, preeclampsia, infection/inflammation, and number of previous pregnancies were dichotomized. Subjects were also dichotomized based on the extent of their periodontal disease. If ≥10% of their measured sites had ≥ 5 mm probing depths, they were considered to have moderate-to-severe periodontal disease. If less than 10% they were considered to have healthy or mild periodontal disease. For each variable, nominal logistic regression analysis was used to calculate the odds of a woman’s having a preterm a PT. No subject indicated substance abuse during the current pregnancy. Statistical analyses were performed with JMP Statistical Software (SAS Institute Inc., Cary, NC).
Results
59 subjects were eligible to participate, 29 were in the PT and 30 in the T groups. For the two groups variances were equal (p≥0.05); however, age distributions were not normally distributed (p<0.05), so the non-parametric Wilcoxon test was used to compare group, for which there was no significant difference between ages (Wilcoxin-test, p=0,23). Of the 29 subjects with PT, 14 (48%) were African American and 15 (52%) were white, Table S1.
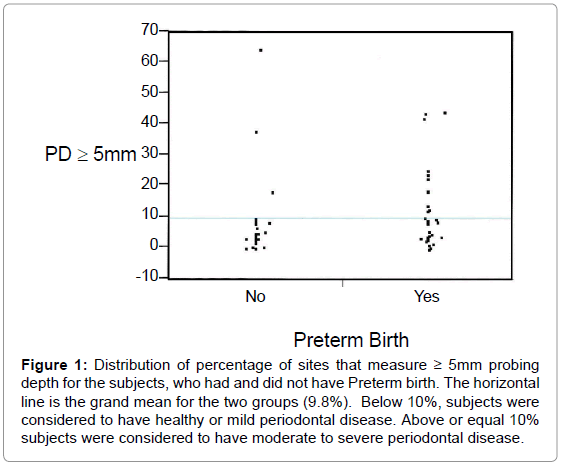
The distribution of percentage of sites measuring ≥ 5mm probing depth are illustrated in Figure 1 and Table 1, which contains a cross tabulation of the numbers of patients’ PT and their periodontal disease status; Table 1 also contains other cross tabulations. Eleven of 14 (79%) of subjects with moderate-severe periodontal disease had PT whereas 3 of 14 (21%) had mild periodontal disease. Nineteen of 44 (43%) of subjects, who were not smokers did not have PT whereas 10 of 15 (67%) of subjects who were smokers had PT. Twenty-four of 53 (45%) of subjects, who did not have preeclampsia did not have PT whereas 5 of 6 (83%) of subjects who had preeclampsia had PT. Fourteen of 37 (18%) of subjects, who did not have infection/inflammation did not have PT whereas 15 of 22 (68%) subjects who had infection/inflammation had PT. Six of 21 (29%) of subjects, who did not have previous pregnancies did not have PT birth whereas 23 of 38 (61%) of subjects who had previous pregnancies had PT birth. The results of a nominal logistic regression analysis (Table 2) indicated that after adjustment for smoking, preeclampsia, and infections/inflammation, a statistically significant association was found between PT and moderate to severe periodontal disease (odds ratio =5.8, 95% CI=1.2-37.5, p=0.04). The association between smoking and PT birth was not significant (odds ratio =1.6, 95% CI=0.3-8.8, p=0.61). There was a significant association between PT and preeclampsia (odds ratio =18.02, 95% CI=2.1- 420.6, p=0.02), but no significant association between inflammation/infection (including potential dental infection) and PT (odds ratio =3.3, 95% CI =0.8-14.5, p=0.09) nor between previous pregnancy and PT (odds ratio=3.6, 95% CI=0.9-16.8, p=0.08).
Figure 1: Distribution of percentage of sites that measure ≥ 5mm probing depth for the subjects, who had and did not have Preterm birth. The horizontal line is the grand mean for the two groups (9.8%). Below 10%, subjects were considered to have healthy or mild periodontal disease. Above or equal 10% subjects were considered to have moderate to severe periodontal disease.
| PT (n = 29) |
Term (n = 30) |
Total (n = 59) |
P value* | |
|---|---|---|---|---|
| Periodontal status | ||||
| Healthy or Mild | 18 | 27 | 38 | 0.02 |
| Moderate-Severe | 11 | 3 | 21 | |
| Smoker | ||||
| No | 19 | 25 | 44 | 0.14 |
| Yes | 10 | 5 | 15 | |
| Preeclampsia | ||||
| No | 24 | 29 | 53 | 0.1 |
| Yes | 5 | 1 | 6 | |
| Infection/inflammation | ||||
| No | 14 | 23 | 37 | 0.03 |
| Yes | 15 | 7 | 22 | |
| Prior pregnancy | ||||
| No | 6 | 15 | 21 | 0.03 |
| Yes | 23 | 15 | 38 | |
*Fisher’s exact test
Table 1: Cross-tabulations of PT with (1) periodontal status, (2) smoking, (3) preeclampsia, (4) infection/inflammation, and (5) prior pregnancies.
| Term | Parameter Estimate | Standard error | Chi-square value | Odds ratio | 95% CI* | P value |
|---|---|---|---|---|---|---|
| Periodontal disease (mod-severe) | 0.88 | 0.43 | 4.18 | 5.8 | 1.2-37.5 | 0.04 |
| Smoking | 0.22 | 0.43 | 0.27 | 1.6 | 0.3-8.8 | 0.61 |
| Preeclampsia | 1.45 | 0.63 | 5.31 | 18 | 2.1-420.6 | 0.02 |
| Infection/inflammation | 60 | 0.36 | 2.79 | 3.3 | 0.8-14.5 | 0.09 |
| Previous pregnancy | 0.64 | 0.36 | 3.06 | 3.6 | 0.9-16.8 | 0.08 |
*95% confidence interval.
Table 2: Results of logistic regression analysis of the influence of periodontitis, smoking, preeclampsia and infection/inflammation on PT.
Discussion
This study demonstrated that moderate to severe periodontal disease is associated with preterm birth. This association is highly significant with odds ratio of 5.8 (p=0.04). These findings are in agreement with many other studies that found a positive correlation [4,6-10].
The first study to suggest an association between periodontal disease and preterm labor and low birth weight was in 1996 [4], despite the differences in the selection criteria, adjusted variables and definition of periodontal disease, the investigators found that results consistent with this study with odds ratio for periodontal disease and premature birth 7.9. In a 5-year prospective study titled “Oral Conditions and Pregnancy (OCAP)” Offenbacher et al. [11], demonstrated that both antepartum maternal periodontal disease and incidence/progression of periodontal disease based on full mouth periodontal examination are associated with preterm birth and growth restriction. Regarding the potential mechanism behind this relationship is that premature birth and periodontal disease share a common pathological pathway, inflammation [12-16]. Pathogenesis of periodontitis involves release of inflammatory cytokines, specially IL-1B, PGE2, TNF alpha. Labor can be induced if a threshold level of inflammatory cytokines in fetoplacental units is reached before 37 weeks of gestation [12,17]. Remote infections such as periodontitis can trigger this rise in cytokine level and promote premature labor.
One of the shortcomings of this study is the parameters used to define periodontal disease. We used deep probing depth percentage to assess the extent and severity of periodontal disease. The current best practices for diagnosing periodontal disease is based on a set of clinical and radiographic evaluations. Some studies investigating this relationship have used PD, BOP, and CAL as an indicators of periodontal disease [11,18-21]. Radiographic evaluation was not possible within the hospital setting and in consideration of the patient’s comfort. It may have been better to include bleeding on probing, which may be a better reflection of the inflammatory status of the periodontal pockets and systemic markers of inflammation that represent tissue invasion and systemic dissemination of organisms [22]. Attachment level, a widely acceptable measure of chronic periodontitis, may not be the most appropriate clinical measure when the goal is to assess periodontitis as an exposure for a systemic disease. Attachment loss may only be a blunt indicator of the current status of the underlying causes of periodontitis, infection, and inflammatory response, which may be better represented by PD and BOP [22]. Other intraoral infections can pose similar effect on systemic health as periodontal disease. As a matter of fact, pericoronitis can pose a more acute form of infection and hence systemic inflammatory burden. A study was conducted to detect the effect of asymptomatic third molars on periodontal disease and inflammatory mediators. Results indicated that the levels of GCF IL-1B and PGE2 were higher if a patient had a PD equal to or greater than 5 mm in the third molar region [23]. By exclusion of inaccessible third molars in this study and other studies a major source of inflammation and infection can be missed.
In our study subjects with deep cavities, remaining roots, dental purulent exudate were considered as having an infection and were adjusted for in our statistical analyses. Other factors that could have affected the periodontal inflammatory status is that postpartum women can be taking non- steroidal anti-inflammatory medications to control pain. All preterm labor group were given steroid injection to halt down labor and help in baby’s lungs maturation. Smoking is another factor that might mask the degree of bleeding on probing masking the inflammatory status of the patient. Antibiotics were also given in many patients which might have affected the periodontal bacterial load and hence the inflammation. That is why prospective studies are preferred to view results from a different perspective. One prospective study conducted before delivery on a large sample size of 1,313 subjects [7], examined periodontal status at 21 -24 weeks of gestation. Their results were in accordance with our results, they concluded that preexisting periodontal disease in the second trimester of pregnancy increases the risk of preterm labor with odds ratio of 4.45 to 7.07 for subjects with generalized periodontitis. Some interventional studies are also in support of our [24-26], provided periodontal treatment before 28 weeks of gestation for 200 women compared to 200 women who were not treated, periodontal therapy during pregnancy was found to significantly reduces the rates of preterm labor and low birth weight in women with periodontal disease. They also concluded that periodontal disease was the strongest factor among other risk factors related to Preterm Labor and Low birth Weight odds ratio of 4.7. Unlike other studies, we adjusted for preeclampsia as a known risk factor for preterm labor and low birth weight; we found that preeclampsia was highly correlated and independent risk factor for preterm labor and low birth weight. Other studies suggested an association between preeclampsia and periodontal disease [19,27]. Preeclampsia also involves increase in inflammatory cytokines in the blood stream, which makes adjusting for preeclampsia in our study important before any conclusion can be made. On the other hand, many studies did not find a positive correlation between periodontal disease and preterm labor [28-32]. Based on these results they do not support a specific drive to improve periodontal health of pregnant women as a means of improving pregnancy outcomes [28]. Another study that did not find any significant relationship used partial mouth recordings which may underestimates the prevalence of periodontal disease [29]. An interventional study did not find a difference in the clinical periodontal status between preterm low birth weight cases and normal birth weight outcome. However, PLBW mothers had significantly higher levels of Bacteroides forsythus and Campylobacter rectus, and consistently elevated counts for the other species examined. It is worth mentioning that the sample size in that study was too small [31]. Studies were both performed in the United States [4,7], involved higher proportions of subjects from African American ethnic groups (approximately 60% of Offenbacher’s and 82% of Jeffcoat’s cohorts), which is a known risk factor. Racial disparity should be taken into consideration when appraising these studies. A more recent systematic review and metaanalysis of randomized controlled trials evaluated the efficacy of scaling and root planning in reducing preterm birth and low birth weight risks. In those studies, they analyzed important subgroups and to further explore heterogeneity and bias risks in the pooled studies. The analysis indicated statistically significant effect in reducing risk of preterm birth for scaling and root planning in pregnant women with periodontitis for groups with high risks of preterm birth only. According to that study there was insufficient evidence to support the need for periodontal disease treatment to reduce preterm birth but periodontal treatment may be beneficial for populations in which the incidence of preterm birth is high [33].
Conclusions
Generalized moderate to severe periodontal disease clinically manifested by probing depths measuring ≥5mm in ≥10% of sites is an independent risk factor for preterm birth with odds ratio of 5.8 (95% CI =1.2-37.5, p=0.04). After adjustment for other significant risk factors of smoking, preeclampsia, infections/inflammation, number of previous pregnancies. There is a need for further interventional prospective multicenter studies with larger sample size and different ethnic backgrounds to support such an association relationship.
Clinical relevance
Scientific rationale for the study: The evidence that a relationship between periodontal disease and some systemic diseases such as cardiovascular diseases, arthritis, stress, preeclampsia and preterm birth is controversial.
Principal findings: This retrospective case-control study was performed to explore whether periodontitis can adversely affect pregnancy outcome. A positive correlation was found as a result of this study.
Practical implications: Studies supporting this relationship can be used to motivate health care providers and pregnant women to maintain good oral health during pregnancy and may contribute to prevention of a serious condition that is preterm birth.
References
- Goldenberg RL, Andrews WW, Hauth JC ( 2002) Choriodecidual infection and preterm birth. Nutr Rev 60: 19-25.
- Gibbs RS (2001) The relationship between infections and adverse pregnancy outcomes: an overview. Ann Periodontol 6: 153-163.
- McGaw T (2002) Periodontal disease and preterm delivery of low-birth-weight infants. J Can Dent Assoc 68: 165-169.
- Offenbacher S, Katz V, Fertik G, Collins J, Boyd D, et al. (1996) Periodontal infection as a possible risk factor for preterm low birth weight. J Periodontol 67: 1103-1113.
- Haake S (1996) Periodontal microbiology, microorganisms associated with specific periodontal diseases. In: Carranza√ʬ?¬?s Clinical Periodontology. pp: 93-94.
- Varadan M, Ramamurthy J ( 2015) Association of Periodontal Disease and Pre-term Low Birth Weight Infants. J Obstet Gynaecol India 65: 167-171.
- Jeffcoat MK, Geurs NC, Reddy MS, Cliver SP, Goldenberg RL, et al. (2001) Periodontal infection and preterm birth: results of a prospective study. J Am Dent Assoc 132: 875-880.
- Offenbacher S, Jared HL, O'Reilly PG, Wells SR, Salvi GE, et al. (1998) Potential pathogenic mechanisms of periodontitis associated pregnancy complications. Ann Periodontol 3: 233-250.
- Scannapieco FA, Bush RB, Paju S (2003) Periodontal disease as a risk factor for adverse pregnancy outcomes. A systematic review. Ann Periodontol 8: 70-78.
- Khader YS, Ta'ani Q (2005) Periodontal diseases and the risk of preterm birth and low birth weight: a meta-analysis. J Periodontol 76: 161-165.
- Offenbacher S, Lieff S, Boggess KA, Murtha AP, Madianos PN, et al. (2001) Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growthrestriction. Ann Periodontol 6: 164-174.
- Creasy RK, Iams JD (1999) Preterm Labor and Delivery. In: Maternal-Fetal Medicine. Saunders, Philadelphia, pp: 498-531.
- Page RC (1998) The pathobiology of periodontal diseases may affect systemic diseases: inversion of a paradigm. Ann Periodontol 3: 108-0120.
- Offenbacher S (1996) Periodontal diseases: pathogenesis. Ann Periodontol 1: 821-878.
- Madianos PN, Bobetsis YA, Offenbacher S (2013) Adverse Pregnancy Outcomes (APOs) and Periodontal Disease: Pathogenic Mechanisms. J Periodontol 84: 170-180.
- Sanz M, Kornman K; working group 3 of the joint EFP/AAP workshop (2013) Periodontitis and adverse pregnancy outcomes: consensus report of the Joint EFP/AAP Workshop on Periodontitis and Systemic Diseases. J Periodontol 84: 164-169.
- Perunovic NDJ, Rakic MM, Nikolic LI, Jankovic SM, Aleksic ZM, et al. (2016) The Association Between Periodontal Inflammation and Labor Triggers (Elevated Cytokine Levels) in Preterm Birth: A Cross-Sectional Study. J Periodontol 87: 248-256.
- Jeffcoat MK, Hauth JC, Geurs NC, Reddy MS, Cliver SP, et al. (2003) Periodontal disease and preterm birth: results of a pilot intervention study. J Periodontol 74: 1214-1218.
- Rich√?¬© EL, Boggess KA, Lieff S, Murtha AP, Auten RL, et al. (2002) Periodontal disease increases the risk of preterm delivery among preeclamptic women. Ann Periodontol 7: 95-101.
- Radnai M, Gorz√?¬≥ I, Nagy E, Urb√?¬°n E, Nov√?¬°k T, et al. (2004) A possible association between preterm birth and early periodontitis. A pilot study. J Clin Periodontol 31: 736-741.
- Davenport ES, Williams CE, Sterne JA, Sivapathasundram V, Fearne JM, et al. (1998) The East London Study of Maternal Chronic Periodontal Disease and Preterm Low Birth Weight Infants: study design and prevalence data. Ann Periodontol 3: 213-221.
- Beck JD, Offenbacher S (2002) Relationships among clinical measures of periodontal disease and their associations with systemic markers. Ann Periodontol 7: 79-89.
- White RP Jr, Offenbacher S, Phillips C, Haug RH, Blakey GH, et al. (2002) Inflammatory mediators and periodontitis in patients with asymptomatic third molars. J Oral Maxillofac Surg 60: 1241-1245.
- L√?¬≥pez NJ, Smith PC, Gutierrez J (2002) Periodontal therapy may reduce the risk of preterm low birth weight in women with periodontal disease: a randomized controlled trial. J Periodontol 73: 911-924.
- Polyzos NP, Polyzos IP, Mauri D, Tzioras S, Tsappi M, et al. (2009) Effect of periodontal disease treatment during pregnancy on preterm birth incidence: a metaanalysis of randomized trials. Am J Obstet Gynecol 200: 225-32.
- Reddy BV, Tanneeru S, Chava VK (2014) The effect of phase-I periodontal therapy on pregnancy outcome in chronic periodontitis patients. J Obstet Gynaecol 34: 29-32.
- Oettinger-Barak O, Barak S, Ohel G, Oettinger M, Kreutzer H, et al. (2005) Severe pregnancy complication (preeclampsia) is associated with greater periodontal destruction. J Periodontol 76: 134-137.
- Davenport ES, Williams CE, Sterne JA, Murad S, Sivapathasundram V, et al. (2002) Maternal periodontal disease and preterm low birthweight: case-control study. J Dent Res 81: 313-318.
- Moore S, Randhawa M, Ide M (2005) A case-control study to investigate an association between adverse pregnancy outcome and periodontal disease. J Clin Periodontol 32: 1-5.
- Buduneli N, Baylas H, Buduneli E, T√?¬ľrkoglu O, K√?¬∂se T, et al. (2005) Periodontal infections and pre-term low birth weight: a case-control study. J Clin Periodontol 32: 174-181.
- Mitchell-Lewis D, Engebretson SP, Chen J, Lamster IB, Papapanou PN (2001) Periodontal infections and pre-term birth: early findings from a cohort of young minority women in New York. Eur J Oral Sci 109: 34-39.
- Bulut G, Olukman O, Calkavur S ( 2014). Is there a relationship between maternal periodontitis and pre-term birth? A prospective hospital-based case-control study. Acta Odontol Scand 72: 866-873.
- Kim AJ, Lo AJ, Pullin DA, Thornton-Johnson DS, Karimbux NY ( 2012) Scaling and root planing treatment for periodontitis to reduce preterm birth and low birth weight: a systematic review and meta-analysis of randomized controlled trials. J Periodontol 83: 1508-1519.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 12332
- [From(publication date):
August-2016 - Apr 03, 2025] - Breakdown by view type
- HTML page views : 11262
- PDF downloads : 1070