Percutaneous Transesophageal Gastrostomy (Pteg): An Institutional Review and Largest Reported Case Series in the United States (U.S.)
Received: 02-Jan-2023 / Manuscript No. jpcm-23-86402 / Editor assigned: 05-Jan-2023 / PreQC No. jpcm-23-86402(PQ) / Reviewed: 18-Feb-2023 / QC No. jpcm-23-86402 / Revised: 23-Feb-2023 / Manuscript No. jpcm-23-86402(R) / Published Date: 30-Jan-2023 DOI: 10.4172/2165-7386.1000496
Abstract
This study aims to determine the safety and efficacy of percutaneous transesophageal Gastrostomy (PTEG) in patients with malignant bowel obstructions (MBO). To date, only small case series of PTEG have been published in the U.S. We aim to provide data via a review of PTEG indications, placements, and outcomes in what is the largest case series published in the U.S. A retrospective review of PTEG candidates in Arizona from 2014-2022. A total of 38 cases of PTEG procedures were included in the final data evaluation. The series included 19/38 (50%) male patients and 19/38 (50%). Three (8%) PTEG placements were performed without the use of anesthesia while the remainder (92%) were performed on patients under anesthesia. Clinical indication, method of placement, clinical outcome, mortality following placement and efficacy were evaluated. All PTEG placements were on the left side. All patients with successful PTEG placement experienced improved clinical symptoms. Technical success was achieved in 35/38 (92%) of patients. Overall, this large case series has proven that PTEG is a viable and durable option for patients with relative or absolute contraindications to traditional percutaneous gastrostomy tube placement for venting for MBO, proving itself to be an essential tool for oncology patients.
Keywords
Percutaneous transesophageal gastrostomy; Malignant bowel obstruction; Interventional radiology
Introduction
Malignant small bowel obstruction (MBO) is a frequent complication in many advanced cancer patients with a global prevalence thought to range from 3% - 15% of cancer patients [1]. During the course of MBO, patients face significant symptoms like pain, nausea, vomiting and inability to eat [2]. Some common treatment methods for MBO include palliative surgery, pharmacological management, nasogastric (NG) tube placement or percutaneous endoscopic gastrostomy (PEG) tube placement, among others [2,3].
Regardless of the technique used, long-term outcomes and prognosis for these patients are usually poor [3]. Surgical interventions are rarely recommended in these patients who are often terminally ill and have little physical reserve [4]. However, even in cases where patients meet the criteria for surgery, there is a high risk of morbidity andpost-surgical complications [5- 6].
Additionally, while NG tubes and PEG tubes are commonly used to resolve MBO
Their use has been contraindicated in many patients and been associated with severe complications. Prolonged NG tube use causes severe discomfort and can lead to mucosal ulceration [7]. On the other hand, PEG tube placement has been used to decompress inoperable MBO, and its use is often contraindicated; complications have been reported following the use of PEG including abdominal pain and even death [8].
Therefore, for patients with inoperable MBO and contraindications to percutaneous gastrostomy tube placement, there are very limited options for management of symptoms [9]. One study reported the mean survival time of patients with inoperable MBO to be less than four to five weeks [1]. Recently, percutaneous transesophageal gastric tube (PTEG) has become a promising alternative tool available for symptomatic control for these patients. PTEG is a less frequently used minimally invasive technique that utilizes aesophagostomy to access the gut rather than direct access [10].
The selection criteria and placement technique for in which PTEG could be offered when percutaneous gastrostomy was contraindicated was first described by Oishi et al. in 1994; primarily in total gastrectomy and abdominal ascites cases [11]. The first case series of PTEG in the U.S. was published in 2003 by Mackey et al. using the PTEG kit developed by Sumimoto Bakelite Co Ltd [12]. Since then, several small case series of PTEG have been published building on the safety and efficacy demonstrated in the original study [13-14].
However, there are few case studies determining the efficacy of PTEG. To date, only small case series of PTEG have been published in the U.S. Thus, to adequately compare the safety and outcomes of PTEG to treat MBO, a comprehensive retrospective review of PTEG procedures used to treat MBO was performed at the author’s institution over an review the author’s institutional experience with PTEG placements and provide a review eight-year span to understand the outcomes in a large cohort of patients. Here, we will of the current literature.
Materials and Method
After institutional review board approval, the data collection was performed utilizing the electronic medical record system, Epic (Epic Systems Corporation, Verona, Wisconsin) for “percutaneous transesophageal gastrostomy” and “PTEG” revealed 38 patients over a 8-year period from 2014 to 2022. These 38 patients were included in the final cohort. The medical chart was reviewed for clinical indication, method of placement, clinical outcome, mortality following placement, and efficacy outcomes. Efficacy of the PTEG placement was determined by symptom improvement, the ability to discharge the patient, prevention of additional intervention (ie. surgical procedures or other interventions for bowel obstruction) and reduction in dose and/or frequency of antiemetic use.
Complications from the PTEG procedure were assessed using the SIR (Society of Interventional Radiology) standards of practice guidelines for adverse event classification [15]. The categories assessed include bleeding (major and minor), infection, nausea, aspiration within 24 hours of the procedure, readmissions related to catheter complications, and death. The study was approved by the Mayo Clinic IRB. Informed consent was waived due to the retrospective nature of the study.
Placement technique and tube management
Standard PTEG placement is performed under general anesthesia with the patient in a supine position. SIR Anticoagulation Guidelines are followed with INR < 1.5 and platelet count > 50k/uL [16].
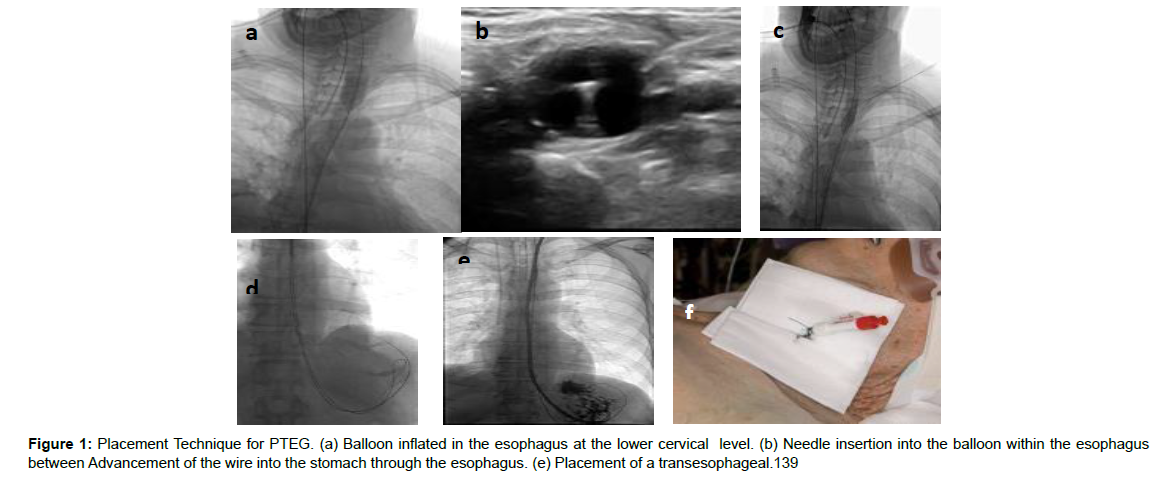
Nasogastric access prior to the start of the procedure is obtained in order to assure removal of gastric contents and prevent aspiration. A 10 mm or greater endovascular/endoscopic balloon is placed into the esophagus and inflated with a combination of saline and contrast. The balloon is then retracted to the level of the cricopharyngeus muscle. A 21g needle is advanced under ultrasonographic and fluoroscopic guidance into the balloon through the space between the carotid artery and thyroid a couple centimeters cranial to the clavicle. A wire is advanced through the needle into the balloon, and both the wire and the balloon are pushed as a unit into the stomach.
The balloon is then removed, and after exchanging for an extra stiff wire, the tract is dilated to accept a predetermined 10F or 12F catheter. The catheter is then placed over the wire and into the stomach, followed by the removal of the wire. The tube is secured to the skin at the neck site with a retention suture. The step-by-step procedure for placing the PTEG is shown in Figure 1.
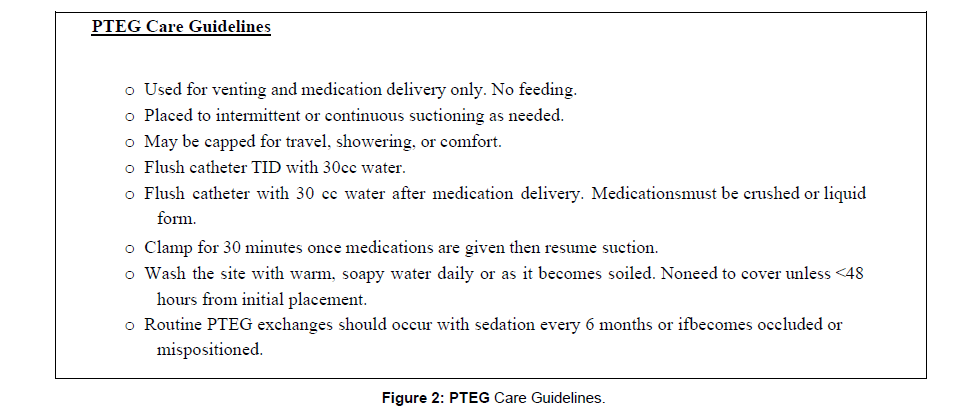
After placement, the tube should be attached to continuous or intermittent suction if used for venting. If the tube is also to be used for medication administration, suction should be held for 30 minutes after administration and the patient should remain upright for the 30 minutes to prevent gastroesophageal reflux. The tube should be briskly flushed 1-2 times daily with 30 mL of saline to keep the tube patent. Routine catheter exchanges are performed every 6 months as needed. A comprehensive set of guidelines for PTEG care can be found in Figure 2.
Results
Patient characteristics
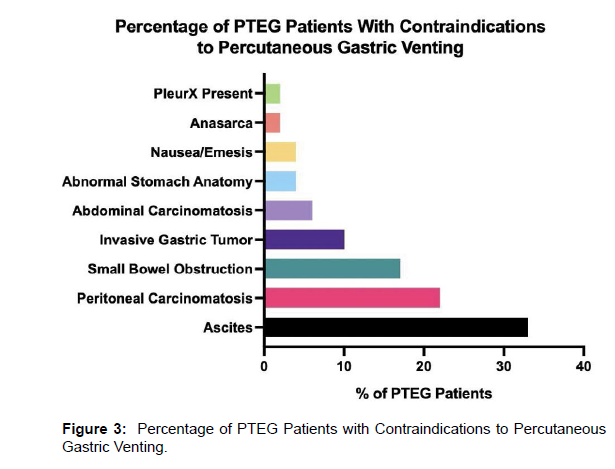
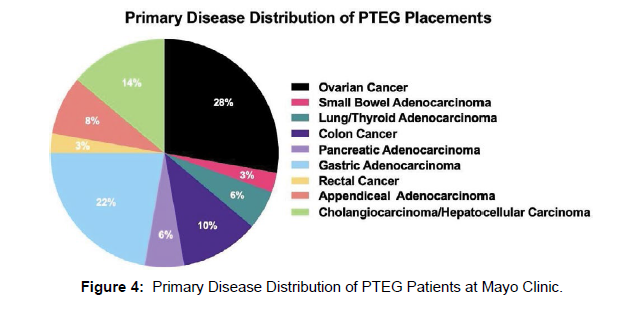
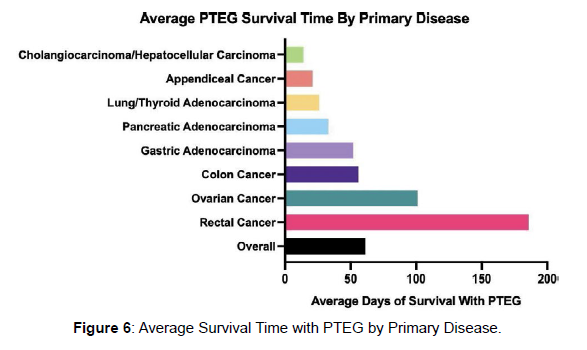
This series included 19 female and 19 male patients with ages ranging from 21-75 years and an average of 56 years. Median BMI was 24.3 kg/ m^2 (range 15.3-38.9). Observed contraindications for conventional percutaneous gastrostomy tube included ascites (33%), peritoneal carcinomatosis (22%), invasive gastric cancer (10%), abdominal carcinomatosis (6%), and abnormal stomach anatomy to include intrathoracic stomach (4%) (Figure 3). The most common malignancies included ovarian (28%), gastric (22%), cholangiocarcinoma (14%), colon (10%), among others (26%) (Figure 4). Three PTEG placements were performed as an outpatient procedure, while the remainder was performed on hospitalized patients. . The patient characteristic data is summarized in Table 1.
| Patient Characteristics | Value |
|---|---|
| Age | 56 [Range 21 - 75] years |
| BMI | 24.3 [Range: 15.3-38.9] kg/m2 |
| Sex | Male: 19 (50%) Female: 19 (50%) |
| ECOG | 2 [1-4] |
| History of Head and Neck Radiation | 2 |
| Enlarged Thyroid | 1 |
Table 1: Patient Characteristics and Outcomes.
Technical success
Technical success was achieved in 35/38 (92%) of patients. The three failed placements were complicated by a history of radiation to the neck, an inability to image and puncture the balloon, and an enlarged and nodular thyroid, respectively. No association between technical failure and BMI, age, or cancer type was identified. All PTEG placements were on the left side. There was low variability in placement technique with all using a 21g needle, esophageal balloon (14F), and placement tube size and length (14F and 45cm). Of note, active or prior chemotherapy use, and anticoagulation were not associated with poor outcomes or increased rates of bleeding.
Clinical success
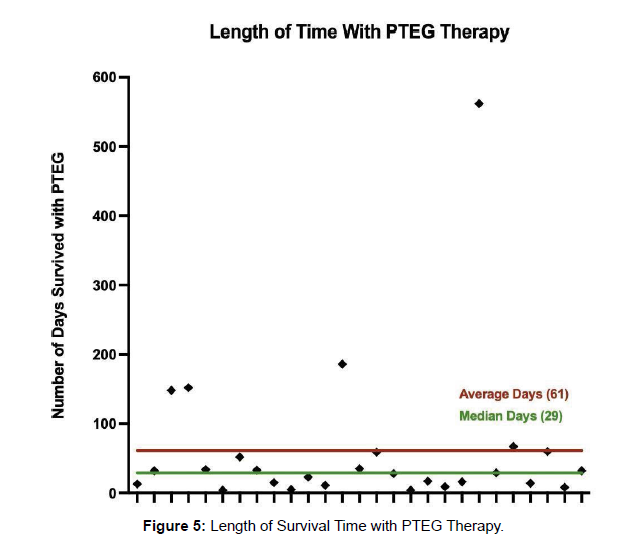
All patients with successful PTEG placement experienced improved clinical symptoms. 6 catheter exchanges were performed after PTEG placement with the most common indication being tube displacement. Other indications for catheter exchange included concerns for clog (5) and catheter fracture (1). Median catheter duration was 29 days (IQR 46 days), and all cases resulted in patient death in the setting of the patient’s underlying disease except for one case. The maximum duration of catheter use was 562 days. The median time to discharge after PTEG placement was 1.6 days (IQR 4.5 days). 2 patients were readmitted after discharge related to the PTEG. Both patients were not properly using the tube for venting and required further education. One patient was admitted for infection of the skin site. The other patient was admitted due to displacement of the PTEG which had advanced into the proximal duodenum. This was repositioned without further issue.
Safety
There was one death within 24 hours after PTEG placement resulting from a major aspiration event. The intraprocedural PTEG placement for this patient was uncomplicated. 5 mild adverse events occurred consisting of mild pain/discomfort at the site (4) and site infection (1). Pain and discomfort resolved within 1 week for all 4patients after conservative symptomatic treatment. One patient underwent placement of PTEG with moderate sedation only and experienced esophageal discomfort and nausea during the procedure.
However, the procedure was completed without complication. Theremainder of the cases were performed with general anesthesia.
Discussion
Success
These findings suggest placement and subsequent management of PTEG are safe and effective. Patient outcomes and efficacy of PTEG therapy are summarized in Table 2. All PTEGs were placed on the left side, however, it was noted during placement that the balloon sometimes migrated to the right neck on inflation and was easily visualized by ultrasound. Finger pressure on the right neck or a second esophageal balloon was used to move the esophagus and balloon to the left side for placement in these instances. While no right-sided placements have been reported in the literature, there have been no contraindications identified for PTEG placement on the right. Indwelling catheter position may be a reason for predominantly left-sided placements as they can result in a higher possibility of infection. Technical success was 92% and is in keeping with other published results. General anesthesia is highly recommended due to patient discomfort during balloon inflation within the esophagus. Lidocaine jelly coating the esophageal balloon was found to decrease throat discomfort after placement. Additionally, the presence of a tracheostomy tube does not appear to affect procedure success [17].
Complications
The most frequent minor complication after PTEG was the displacement of the tube, such that it was pulled back into the esophagus. This was often noted by the clinical service when symptoms of bowel obstruction returned and there was minimal return during suction. Chest x-ray readily identified malposition of the tube which could then easily be replaced and repositioned into the stomach. The percutaneous tract was accessed within 48 hours, and the PTEG was able to be replaced with local anesthesia through the existing tract.
Additionally, infection at the access site was uncommon. Only one site infection was reported, which occurred in a single patient. After PTEG placement, the patient developed redness and pain at the site eventually developing mild cellulitis.
The most common subjective complaints by patients with malignant bowel obstruction are nausea and vomiting. PTEG has proven superior in reducing these symptoms when compared to nasogastric tube decompression. Out of the 31 patients with reported antiemetic use, 21 (67%) patients were documented to have a decreased amount and/or frequency of antiemetic use following the PTEG placement.
Additionally, the placement of PTEGs in this case series was often late in the disease course. The majority of the patients died within 30 days of placement. The catheters demonstrated durable access into the stomach for venting in 4 of the patients maintaining the catheter for more than 90 days. One of the patients maintained the catheter for over 1 year (562 days) (Figure 5). This may be due to a lack of provider knowledge about the availability of the procedure and its indications. The majority of PTEG placements were suggested by the interventional radiologist upon review for a venting gastrostomy tube. Regardless, PTEG placement can be performed on terminally ill patients while maintaining functional status. No significant association was identified between ECOG score and major/minor complication rates (p>0.05). The pre-procedural and post- procedural complications are summarized in Table 2.
| Safety and Outcomes | Value | |
|---|---|---|
| Minor Bleeding | 0 | |
| Major Bleeding | 0 | |
| Complications (Procedural) |
Infection | 1 |
| Injury to Adjacent Structures | 0 | |
| Death | 1 | |
| Aspiration | 1 | |
| Leak | 0 | |
| Complications (Post-Procedure) |
Mild Pain | 5 |
| Tube Dysfunction | 1 | |
| Tube Dislodgement / Exchange | 5 | |
| Readmission within 30 days | 2 (home suction machine failure and infection) | |
| Patient Satisfaction | ||
| Tube removal (patient dissatisfaction) |
0 | |
| Venting | 40 | |
| Efficacy | Feeding | 0 |
| PTEG Longevity | 56.5 days [Range 2 - 562 days] | |
Table 2: Outcomes and Complications during and following PTEG treatment.
Comparison to other studies
Aramaki et al. demonstrated that PTEG was preferable to NGT in 40 patients (21 PTEG, 19 NGT) with a randomized controlled trial in the setting of malignant bowel obstruction using patient reported symptoms on a Likert scale for 2 weeks post placement as well as EQ- 5D and SF-8 [18]. There were no differences in survival, and there were no serious adverse events. Some studies report using the PTEG for feeding [17, 19]. In these patients, it is important to confirm that no bowel obstruction is present as this can lead to subsequent worsening of symptoms and aspiration. The majority of our patients presented with bowel obstruction in the malignant setting, therefore venting was the appropriate approach.
Swallowing functionality does not appear to be affected by the presence of a PTEG. Additionally, in some patients, dysphagia was found to improve with rehabilitation [17]. In our study, clamping the PTEG for 30 minutes following medication delivery was a 261 viable method. PTEG placement did not prevent limited liquid intake for palliative measures.
One of the advantages of PTEG is that it can be used immediately following its
Placement as the insertion site is far from the feeding site [17]. Gastric peristalsis is not found to be affected as no gastropexy is created [17]. Furthermore, the PTEG can be removed and has not been shown to cause esophageal stenosis or persistent 267 esophagocutaneous fistula [13]. The majority of studies utilize IV sedation over general anesthesia. However, we have found that our patient population is of high acuity and at a larger risk for complications (i.e. reflux and aspiration) with balloon inflation. Therefore, general anesthesia was instituted routinely across the author’s institution and was found to be safe and effective. Consideration for sedation could be given, but this would utilize caution, and patient selection would be be key. Therefore, routine exchanges are easily and safely performed with intravenous sedation. Selby et al. showed that in patients with malignant bowel obstruction for which the PTEG was placed for venting; using continuous suction at 120mmHg resolved the symptoms [20]. The symptoms returned if the tube was left to drain by gravity. In some patients using suction at 40-80mmhg was preferable due to discomfort at 120mmHg. Therefore, patient preference was the driving decision for this patient population. Trailing 80-120mmHg at both continuous and intermittent suction was determined solely on patient comfort and satisfaction [20]. Table 3 provides a summary of published PTEG cases that include studies with three or more patients. Limitations There are several limitations to this study. As a retrospective review, the characterization of the patient selection, technique, and follow-up were not standardized and limited to medical chart review. The markers for efficacy and patient satisfaction were surrogate markers. Some patients were lost to follow- up, but most had expired prior to the follow-up. This may have been due to patients often being identified late in their disease course or PTEG being suggested by the interventional radiologist after declining placement for percutaneous gastrostomy placement. Additionally, general anesthesia can limit placement options or be affected by late placement in terminal or difficult patients.
| Author | Year | Indications | GTube contraindications | Placements | Average Placement Time | Technical success | Efficacy | Satisfied (neutral or better) | Major complications | Minor Complications | PTEG/J Duration |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aramaki [18] | 2019 | Venting | Malignant bowel obstruction | 21 | Not reported | 21 | 21 | Superior to NGT | 2 | 15 | 50 d (survival) |
| Selby [20] | 2019 | Venting | Malignant bowel obstruction | 10 | Not reported | 10 | 10 | Majority | 0 | 2 | 15 d (2-35 d) |
| Sanogo [19] | 2019 | Feeding | Multiple: Gastric surgery, contractures/body habitus, gastric window, ascites |
14 | Not reported | 14 | 14 | 9 | 0 | 6 | 3 mo (follow up, 2 patients died prior to 3 mo follow up) |
| Iwase [13] | 2018 | Venting and Feeding | Malignant gastric outlet obstruction | 11 | 39.4 min | 11 | 11 | Not reported | 1 | 3 | Not reported |
| Toh Yoon [17] | 2017 | Feeding | Gastrectomy, diaphragm paralysis, colon interposition | 15 | Not reported | 15 | 15 | Not reported | 2 | 3 | 22 d (8-48 d) (time to discharge) |
| Aramaki [21] | 2013 | Venting | Malignant bowel obstruction or peritoneal carcinomatosis | 33 | 28.5 min | 33 | 30 | Superior to NGT | 1 | Not reported | 73 d (range 6 - 340 d) (survival) |
| Udomsawaengsup [22] | 2008 | Venting or Feeding | Bowel obstruction, carcinomatosis, ascites, esophagectomy/gastrectomy |
17 | Not reported | 16 | 17 | Not reported | 0 | 3 | Not reported |
| Mackey [12] | 2005 | Venting | Ascites | 7 | 15 - 30 min | 7 | 7 | Not reported | 0 | 1 | Not reported |
| Oishi [11] | 2003 | Venting and Feeding | Multiple: Gastrectomy, ascites, dysphagia, severe disease | 115 | 15 min | 115 | 115 | Not reported | 0 | 27 | 76.6 +/- 88.8 days (venting) and 171.2 +/- 151.8 d (feeding) |
Table 3: Summary of published studies on PTEG with cases > 3 patients.
By identifying possible PTEG candidates earlier in their disease course through provider education, the availability for placement may be increased. Furthermore, the small number of patients included in this study limits the power for the study [21]. However, despite this limitation, this is the largest single study of PTEG patients in the United States. Finally, patient follow-up data was difficult to collect due to poor survey responses post- 297 PTEG placement as many patients were too frail or incapacitated to participate [22].
The disadvantage of PTEG placement over a gastrostomy tube is that the placement requires good ultrasound skills and knowledge of cervical anatomy. The knowledge of vasculature and its relation to thyroid structures is critical. Hydro dissection was utilized in several cases to avoid these anatomical areas and prevent unintentional injury to the carotid and thyroid arteries. A trans cervical route posterior to the carotid sheath was used in one study, which was thought to minimize the risk of thyroid or thyroid artery injury [19]. This was not attempted at either facility in this study nor was thyroid artery injury reported. Additionally, proper usage and care of the tube is essential. Given its longer length and utilization as a palliative device only, education to the patient and their caregivers requires additional education efforts on behalf the proceduralist.
Conclusions
In conclusion, PTEG is supported to be a viable and durable option for patients with relative or absolute contraindications to traditional percutaneous gastrostomy tube placement for venting for MBO. In our series, frail patients, even those on anticoagulation or actively receiving, can tolerate and appreciate symptomatic improvement from malignant small bowel obstruction. Although sedation can be used, general anesthesia has proven to be comfortable and safe in the prevention of intra procedural aspiration. The researchers would like to further investigate PTEG as a viable option for gastric feeding and venting in patients with intact gastrointestinal systems with relative contraindications to percutaneous gastrostomy such as ascites. Regardless, this procedure serves as a useful option to provide symptomatic relief for terminally ill, palliative patients who oppose venting via nasogastric tubes. Staff, caregiver, and patient education are critical in 320 preventing inappropriate use of PTEG. Overall, this large case series has proven that 321 PTEG is a safe and effective essential tool for the Interventional Radiologist with oncology 322 patients.
Author Contributions: Conceptualization, LRC, A.W.; methodology, LRC, AW, and GS.; validation, LRC, G.S.; formal analysis, G.S, R.O; writing—original draft preparation, LRC and A.W.writing-review and editing, LRC, A.W, and G.S.; All authors have read and agreed to the published version of the manuscript funding.
Institutional Review Board Statement: The study was approved by the Mayo Clinic IRB. IRB Application #: 21-001685. IRB Approval Date: 3/25/2021.
Informed Consent Statement: According to national legislation, the study was not subject to obtain informed consent due to its retrospective nature.
Data Availability Statement: The data is contained within the article. Further details are available on request from the corresponding author.
Conflict of Interest: The authors declare no conflict of interest.
References
Percutaneous transesophageal gastrostomy; Malignant bowel obstruction; Interventional radiology
Introduction
Malignant small bowel obstruction (MBO) is a frequent complication in many advanced cancer patients with a global prevalence thought to range from 3% - 15% of cancer patients [1]. During the course of MBO, patients face significant symptoms like pain, nausea, vomiting and inability to eat [2]. Some common treatment methods for MBO include palliative surgery, pharmacological management, nasogastric (NG) tube placement or percutaneous endoscopic gastrostomy (PEG) tube placement, among others [2,3].
Regardless of the technique used, long-term outcomes and prognosis for these patients are usually poor [3]. Surgical interventions are rarely recommended in these patients who are often terminally ill and have little physical reserve [4]. However, even in cases where patients meet the criteria for surgery, there is a high risk of morbidity andpost-surgical complications [5- 6].
Additionally, while NG tubes and PEG tubes are commonly used to resolve MBO
Their use has been contraindicated in many patients and been associated with severe complications. Prolonged NG tube use causes severe discomfort and can lead to mucosal ulceration [7]. On the other hand, PEG tube placement has been used to decompress inoperable MBO, and its use is often contraindicated; complications have been reported following the use of PEG including abdominal pain and even death [8].
Therefore, for patients with inoperable MBO and contraindications to percutaneous gastrostomy tube placement, there are very limited options for management of symptoms [9]. One study reported the mean survival time of patients with inoperable MBO to be less than four to five weeks [1]. Recently, percutaneous transesophageal gastric tube (PTEG) has become a promising alternative tool available for symptomatic control for these patients. PTEG is a less frequently used minimally invasive technique that utilizes aesophagostomy to access the gut rather than direct access [10].
The selection criteria and placement technique for in which PTEG could be offered when percutaneous gastrostomy was contraindicated was first described by Oishi et al. in 1994; primarily in total gastrectomy and abdominal ascites cases [11]. The first case series of PTEG in the U.S. was published in 2003 by Mackey et al. using the PTEG kit developed by Sumimoto Bakelite Co Ltd [12]. Since then, several small case series of PTEG have been published building on the safety and efficacy demonstrated in the original study [13-14].
However, there are few case studies determining the efficacy of PTEG. To date, only small case series of PTEG have been published in the U.S. Thus, to adequately compare the safety and outcomes of PTEG to treat MBO, a comprehensive retrospective review of PTEG procedures used to treat MBO was performed at the author’s institution over an review the author’s institutional experience with PTEG placements and provide a review eight-year span to understand the outcomes in a large cohort of patients. Here, we will of the current literature.
Materials and Method
After institutional review board approval, the data collection was performed utilizing the electronic medical record system, Epic (Epic Systems Corporation, Verona, Wisconsin) for “percutaneous transesophageal gastrostomy” and “PTEG” revealed 38 patients over a 8-year period from 2014 to 2022. These 38 patients were included in the final cohort. The medical chart was reviewed for clinical indication, method of placement, clinical outcome, mortality following placement, and efficacy outcomes. Efficacy of the PTEG placement was determined by symptom improvement, the ability to discharge the patient, prevention of additional intervention (ie. surgical procedures or other interventions for bowel obstruction) and reduction in dose and/or frequency of antiemetic use.
Complications from the PTEG procedure were assessed using the SIR (Society of Interventional Radiology) standards of practice guidelines for adverse event classification [15]. The categories assessed include bleeding (major and minor), infection, nausea, aspiration within 24 hours of the procedure, readmissions related to catheter complications, and death. The study was approved by the Mayo Clinic IRB. Informed consent was waived due to the retrospective nature of the study.
Placement technique and tube management
Standard PTEG placement is performed under general anesthesia with the patient in a supine position. SIR Anticoagulation Guidelines are followed with INR < 1.5 and platelet count > 50k/uL [16].
Nasogastric access prior to the start of the procedure is obtained in order to assure removal of gastric contents and prevent aspiration. A 10 mm or greater endovascular/endoscopic balloon is placed into the esophagus and inflated with a combination of saline and contrast. The balloon is then retracted to the level of the cricopharyngeus muscle. A 21g needle is advanced under ultrasonographic and fluoroscopic guidance into the balloon through the space between the carotid artery and thyroid a couple centimeters cranial to the clavicle. A wire is advanced through the needle into the balloon, and both the wire and the balloon are pushed as a unit into the stomach.
The balloon is then removed, and after exchanging for an extra stiff wire, the tract is dilated to accept a predetermined 10F or 12F catheter. The catheter is then placed over the wire and into the stomach, followed by the removal of the wire. The tube is secured to the skin at the neck site with a retention suture. The step-by-step procedure for placing the PTEG is shown in Figure 1.
After placement, the tube should be attached to continuous or intermittent suction if used for venting. If the tube is also to be used for medication administration, suction should be held for 30 minutes after administration and the patient should remain upright for the 30 minutes to prevent gastroesophageal reflux. The tube should be briskly flushed 1-2 times daily with 30 mL of saline to keep the tube patent. Routine catheter exchanges are performed every 6 months as needed. A comprehensive set of guidelines for PTEG care can be found in Figure 2.
Results
Patient characteristics
This series included 19 female and 19 male patients with ages ranging from 21-75 years and an average of 56 years. Median BMI was 24.3 kg/ m^2 (range 15.3-38.9). Observed contraindications for conventional percutaneous gastrostomy tube included ascites (33%), peritoneal carcinomatosis (22%), invasive gastric cancer (10%), abdominal carcinomatosis (6%), and abnormal stomach anatomy to include intrathoracic stomach (4%) (Figure 3). The most common malignancies included ovarian (28%), gastric (22%), cholangiocarcinoma (14%), colon (10%), among others (26%) (Figure 4). Three PTEG placements were performed as an outpatient procedure, while the remainder was performed on hospitalized patients. . The patient characteristic data is summarized in Table 1.
| Patient Characteristics | Value |
|---|---|
| Age | 56 [Range 21 - 75] years |
| BMI | 24.3 [Range: 15.3-38.9] kg/m2 |
| Sex | Male: 19 (50%) Female: 19 (50%) |
| ECOG | 2 [1-4] |
| History of Head and Neck Radiation | 2 |
| Enlarged Thyroid | 1 |
Table 1: Patient Characteristics and Outcomes.
Technical success
Technical success was achieved in 35/38 (92%) of patients. The three failed placements were complicated by a history of radiation to the neck, an inability to image and puncture the balloon, and an enlarged and nodular thyroid, respectively. No association between technical failure and BMI, age, or cancer type was identified. All PTEG placements were on the left side. There was low variability in placement technique with all using a 21g needle, esophageal balloon (14F), and placement tube size and length (14F and 45cm). Of note, active or prior chemotherapy use, and anticoagulation were not associated with poor outcomes or increased rates of bleeding.
Clinical success
All patients with successful PTEG placement experienced improved clinical symptoms. 6 catheter exchanges were performed after PTEG placement with the most common indication being tube displacement. Other indications for catheter exchange included concerns for clog (5) and catheter fracture (1). Median catheter duration was 29 days (IQR 46 days), and all cases resulted in patient death in the setting of the patient’s underlying disease except for one case. The maximum duration of catheter use was 562 days. The median time to discharge after PTEG placement was 1.6 days (IQR 4.5 days). 2 patients were readmitted after discharge related to the PTEG. Both patients were not properly using the tube for venting and required further education. One patient was admitted for infection of the skin site. The other patient was admitted due to displacement of the PTEG which had advanced into the proximal duodenum. This was repositioned without further issue.
Safety
There was one death within 24 hours after PTEG placement resulting from a major aspiration event. The intraprocedural PTEG placement for this patient was uncomplicated. 5 mild adverse events occurred consisting of mild pain/discomfort at the site (4) and site infection (1). Pain and discomfort resolved within 1 week for all 4patients after conservative symptomatic treatment. One patient underwent placement of PTEG with moderate sedation only and experienced esophageal discomfort and nausea during the procedure.
However, the procedure was completed without complication. Theremainder of the cases were performed with general anesthesia.
Discussion
Success
These findings suggest placement and subsequent management of PTEG are safe and effective. Patient outcomes and efficacy of PTEG therapy are summarized in Table 2. All PTEGs were placed on the left side, however, it was noted during placement that the balloon sometimes migrated to the right neck on inflation and was easily visualized by ultrasound. Finger pressure on the right neck or a second esophageal balloon was used to move the esophagus and balloon to the left side for placement in these instances. While no right-sided placements have been reported in the literature, there have been no contraindications identified for PTEG placement on the right. Indwelling catheter position may be a reason for predominantly left-sided placements as they can result in a higher possibility of infection. Technical success was 92% and is in keeping with other published results. General anesthesia is highly recommended due to patient discomfort during balloon inflation within the esophagus. Lidocaine jelly coating the esophageal balloon was found to decrease throat discomfort after placement. Additionally, the presence of a tracheostomy tube does not appear to affect procedure success [17].
Complications
The most frequent minor complication after PTEG was the displacement of the tube, such that it was pulled back into the esophagus. This was often noted by the clinical service when symptoms of bowel obstruction returned and there was minimal return during suction. Chest x-ray readily identified malposition of the tube which could then easily be replaced and repositioned into the stomach. The percutaneous tract was accessed within 48 hours, and the PTEG was able to be replaced with local anesthesia through the existing tract.
Additionally, infection at the access site was uncommon. Only one site infection was reported, which occurred in a single patient. After PTEG placement, the patient developed redness and pain at the site eventually developing mild cellulitis.
The most common subjective complaints by patients with malignant bowel obstruction are nausea and vomiting. PTEG has proven superior in reducing these symptoms when compared to nasogastric tube decompression. Out of the 31 patients with reported antiemetic use, 21 (67%) patients were documented to have a decreased amount and/or frequency of antiemetic use following the PTEG placement.
Additionally, the placement of PTEGs in this case series was often late in the disease course. The majority of the patients died within 30 days of placement. The catheters demonstrated durable access into the stomach for venting in 4 of the patients maintaining the catheter for more than 90 days. One of the patients maintained the catheter for over 1 year (562 days) (Figure 5). This may be due to a lack of provider knowledge about the availability of the procedure and its indications. The majority of PTEG placements were suggested by the interventional radiologist upon review for a venting gastrostomy tube. Regardless, PTEG placement can be performed on terminally ill patients while maintaining functional status. No significant association was identified between ECOG score and major/minor complication rates (p>0.05). The pre-procedural and post- procedural complications are summarized in Table 2.
| Safety and Outcomes | Value | |
|---|---|---|
| Minor Bleeding | 0 | |
| Major Bleeding | 0 | |
| Complications (Procedural) |
Infection | 1 |
| Injury to Adjacent Structures | 0 | |
| Death | 1 | |
| Aspiration | 1 | |
| Leak | 0 | |
| Complications (Post-Procedure) |
Mild Pain | 5 |
| Tube Dysfunction | 1 | |
| Tube Dislodgement / Exchange | 5 | |
| Readmission within 30 days | 2 (home suction machine failure and infection) | |
| Patient Satisfaction | ||
| Tube removal (patient dissatisfaction) |
0 | |
| Venting | 40 | |
| Efficacy | Feeding | 0 |
| PTEG Longevity | 56.5 days [Range 2 - 562 days] | |
Table 2: Outcomes and Complications during and following PTEG treatment.
Comparison to other studies
Aramaki et al. demonstrated that PTEG was preferable to NGT in 40 patients (21 PTEG, 19 NGT) with a randomized controlled trial in the setting of malignant bowel obstruction using patient reported symptoms on a Likert scale for 2 weeks post placement as well as EQ- 5D and SF-8 [18]. There were no differences in survival, and there were no serious adverse events. Some studies report using the PTEG for feeding [17, 19]. In these patients, it is important to confirm that no bowel obstruction is present as this can lead to subsequent worsening of symptoms and aspiration. The majority of our patients presented with bowel obstruction in the malignant setting, therefore venting was the appropriate approach.
Swallowing functionality does not appear to be affected by the presence of a PTEG. Additionally, in some patients, dysphagia was found to improve with rehabilitation [17]. In our study, clamping the PTEG for 30 minutes following medication delivery was a 261 viable method. PTEG placement did not prevent limited liquid intake for palliative measures.
One of the advantages of PTEG is that it can be used immediately following its
Placement as the insertion site is far from the feeding site [17]. Gastric peristalsis is not found to be affected as no gastropexy is created [17]. Furthermore, the PTEG can be removed and has not been shown to cause esophageal stenosis or persistent 267 esophagocutaneous fistula [13]. The majority of studies utilize IV sedation over general anesthesia. However, we have found that our patient population is of high acuity and at a larger risk for complications (i.e. reflux and aspiration) with balloon inflation. Therefore, general anesthesia was instituted routinely across the author’s institution and was found to be safe and effective. Consideration for sedation could be given, but this would utilize caution, and patient selection would be be key. Therefore, routine exchanges are easily and safely performed with intravenous sedation. Selby et al. showed that in patients with malignant bowel obstruction for which the PTEG was placed for venting; using continuous suction at 120mmHg resolved the symptoms [20]. The symptoms returned if the tube was left to drain by gravity. In some patients using suction at 40-80mmhg was preferable due to discomfort at 120mmHg. Therefore, patient preference was the driving decision for this patient population. Trailing 80-120mmHg at both continuous and intermittent suction was determined solely on patient comfort and satisfaction [20]. Table 3 provides a summary of published PTEG cases that include studies with three or more patients. Limitations There are several limitations to this study. As a retrospective review, the characterization of the patient selection, technique, and follow-up were not standardized and limited to medical chart review. The markers for efficacy and patient satisfaction were surrogate markers. Some patients were lost to follow- up, but most had expired prior to the follow-up. This may have been due to patients often being identified late in their disease course or PTEG being suggested by the interventional radiologist after declining placement for percutaneous gastrostomy placement. Additionally, general anesthesia can limit placement options or be affected by late placement in terminal or difficult patients.
| Author | Year | Indications | GTube contraindications | Placements | Average Placement Time | Technical success | Efficacy | Satisfied (neutral or better) | Major complications | Minor Complications | PTEG/J Duration |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Aramaki [18] | 2019 | Venting | Malignant bowel obstruction | 21 | Not reported | 21 | 21 | Superior to NGT | 2 | 15 | 50 d (survival) |
| Selby [20] | 2019 | Venting | Malignant bowel obstruction | 10 | Not reported | 10 | 10 | Majority | 0 | 2 | 15 d (2-35 d) |
| Sanogo [19] | 2019 | Feeding | Multiple: Gastric surgery, contractures/body habitus, gastric window, ascites |
14 | Not reported | 14 | 14 | 9 | 0 | 6 | 3 mo (follow up, 2 patients died prior to 3 mo follow up) |
| Iwase [13] | 2018 | Venting and Feeding | Malignant gastric outlet obstruction | 11 | 39.4 min | 11 | 11 | Not reported | 1 | 3 | Not reported |
| Toh Yoon [17] | 2017 | Feeding | Gastrectomy, diaphragm paralysis, colon interposition | 15 | Not reported | 15 | 15 | Not reported | 2 | 3 | 22 d (8-48 d) (time to discharge) |
| Aramaki [21] | 2013 | Venting | Malignant bowel obstruction or peritoneal carcinomatosis | 33 | 28.5 min | 33 | 30 | Superior to NGT | 1 | Not reported | 73 d (range 6 - 340 d) (survival) |
| Udomsawaengsup [22] | 2008 | Venting or Feeding | Bowel obstruction, carcinomatosis, ascites, esophagectomy/gastrectomy |
17 | Not reported | 16 | 17 | Not reported | 0 | 3 | Not reported |
| Mackey [12] | 2005 | Venting | Ascites | 7 | 15 - 30 min | 7 | 7 | Not reported | 0 | 1 | Not reported |
| Oishi [11] | 2003 | Venting and Feeding | Multiple: Gastrectomy, ascites, dysphagia, severe disease | 115 | 15 min | 115 | 115 | Not reported | 0 | 27 | 76.6 +/- 88.8 days (venting) and 171.2 +/- 151.8 d (feeding) |
Table 3: Summary of published studies on PTEG with cases > 3 patients.
By identifying possible PTEG candidates earlier in their disease course through provider education, the availability for placement may be increased. Furthermore, the small number of patients included in this study limits the power for the study [21]. However, despite this limitation, this is the largest single study of PTEG patients in the United States. Finally, patient follow-up data was difficult to collect due to poor survey responses post- 297 PTEG placement as many patients were too frail or incapacitated to participate [22].
The disadvantage of PTEG placement over a gastrostomy tube is that the placement requires good ultrasound skills and knowledge of cervical anatomy. The knowledge of vasculature and its relation to thyroid structures is critical. Hydro dissection was utilized in several cases to avoid these anatomical areas and prevent unintentional injury to the carotid and thyroid arteries. A trans cervical route posterior to the carotid sheath was used in one study, which was thought to minimize the risk of thyroid or thyroid artery injury [19]. This was not attempted at either facility in this study nor was thyroid artery injury reported. Additionally, proper usage and care of the tube is essential. Given its longer length and utilization as a palliative device only, education to the patient and their caregivers requires additional education efforts on behalf the proceduralist.
Conclusions
In conclusion, PTEG is supported to be a viable and durable option for patients with relative or absolute contraindications to traditional percutaneous gastrostomy tube placement for venting for MBO. In our series, frail patients, even those on anticoagulation or actively receiving, can tolerate and appreciate symptomatic improvement from malignant small bowel obstruction. Although sedation can be used, general anesthesia has proven to be comfortable and safe in the prevention of intra procedural aspiration. The researchers would like to further investigate PTEG as a viable option for gastric feeding and venting in patients with intact gastrointestinal systems with relative contraindications to percutaneous gastrostomy such as ascites. Regardless, this procedure serves as a useful option to provide symptomatic relief for terminally ill, palliative patients who oppose venting via nasogastric tubes. Staff, caregiver, and patient education are critical in 320 preventing inappropriate use of PTEG. Overall, this large case series has proven that 321 PTEG is a safe and effective essential tool for the Interventional Radiologist with oncology 322 patients.
Author Contributions: Conceptualization, LRC, A.W.; methodology, LRC, AW, and GS.; validation, LRC, G.S.; formal analysis, G.S, R.O; writing—original draft preparation, LRC and A.W.writing-review and editing, LRC, A.W, and G.S.; All authors have read and agreed to the published version of the manuscript funding.
Institutional Review Board Statement: The study was approved by the Mayo Clinic IRB. IRB Application #: 21-001685. IRB Approval Date: 3/25/2021.
Informed Consent Statement: According to national legislation, the study was not subject to obtain informed consent due to its retrospective nature.
Data Availability Statement: The data is contained within the article. Further details are available on request from the corresponding author.
Conflict of Interest: The authors declare no conflict of interest.
References
- Tuca A, Guell E, Martinez-Losada E, Codorniu N (2012) Malignant Bowel Obstruction in Advanced Cancer Patients: Epidemiology, Management, and Factors Influencing Spontaneous Resolution. Cancer Manag Res 4:159-169.
- Paul Olson TJ, Pinkerton C, Brasel KJ, Schwarze ML (2014) Palliative Surgery for Malignant Bowel Obstruction from Carcinomatosis. JAMA Surgery 149: 383.
- Yu K, Liu L, Zhang X, Zhang Z, Rao B, et al. (2020) Surgical and Conservative Management of Malignant Bowel Obstruction: Outcome and Prognostic Factors. Cancer Manag Res 12:7797-7803.
- Liang DH, Kim MP, Chan EY, Gaur P (2017) Cervical Esophago-Gastric Tubes for Patients with Malignant Ascites. Journal of Gastrointestinal Surgery 21: 199-201.
- Wancata LM, AbdelsattarZM, Suwanabol PA, Campbell DA, Hendren S (2017) Outcomes After Surgery for Benign and Malignant Small Bowel Obstruction. J Gastrointest Surg 21: 363-371.
- MetzgerY, Song A N, Bruce R, Roses R, Krouse D L, Fraker R R, et al. (2020) Surgery for Malignant Bowel Obstruction Is Associated with Substantial Morbidity and Mortality. 2020 ACS Abstract.
- Prabhakaran S, Doraiswamy VA, Nagaraja V, Cipolla J, Ofurum U, et al. (2012) Nasoenteric Tube Complications. Scandinavian Journal of Surgery 101: 147-155,
- Mori M, Bruera E, Dev R (2009) Complications of a Gastrostomy Tube Used for Decompression of an Inoperable Bowel Obstruction in a Patient with Advanced Cancer. J Pain Symptom Manage38:466-472.
- Franke AJ, Iqbal A, StarrJS, Nair RM, George TJ (2017) Management of Malignant Bowel Obstruction Associated With GI Cancers. J Oncol Pract13: 426- 434.
- Toh Yoon EW, Nishihara K (2017) Percutaneous Transesophageal Gastro-Tubing (PTEG) as an Alternative Long-Term Tube Feeding Procedure When Gastrostomy Is Not Feasible. Therap Adv Gastroenterol 10: 911- 917.
- Oishi H, Shindo H, Shirotani N, Kameoka S A (2003) Nonsurgical Technique to Create an Esophagostomy for Difficult Cases of Percutaneous Endoscopic Gastrostomy. Surgical Endoscopy 17: 1224-1227.
- Mackey R, Chand B, Oishi H, Kameoka S, Ponsky JL(2005)Percutaneous Transesophageal Gastrostomy Tube for Decompression of Malignant Obstruction: Report of the First Case and Our Series in the US. J Am Coll Surg 201: 695-700.
- Iwase R, Suzuki Y, Yamanouchi E, SuzukiN, Imakita T, et al. (2018) Double Percutaneous Transesophageal Gastrotubing for Gastric Cancer: A Pilot Study. J Surg Res 232: 470-474.
- Singal AK, DekovichAA, Tam AL, Wallace MJ (2010) Percutaneous Transesophageal Gastrostomy Tube Placement: An Alternative to Percutaneous Endoscopic Gastrostomy in Patients with Intra-Abdominal Metastasis. Gastrointest Endosc 71: 402-406.
- Khalilzadeh O, Baerlocher MO, Shyn PB, Connolly BL, Devane AM, et al. (2017) Proposal of a New Adverse Event Classification by the Society of Interventional Radiology Standards of Practice Committee. J Vasc Interv Radiol 28: 1432-1437.e3
- Patel IJ, Rahim S, Davidson JC, Hanks SE, Tam AL, et al. (2019) Society of Interventional Radiology Consensus Guidelines for the Periprocedural Management of Thrombotic and Bleeding Risk in Patients Undergoing Percutaneous Image-Guided Interventions-Part II: Recommendations. Journal of Vascular and Interventional Radiology 30: 1168-1184.e1.
- Toh Yoon EW, Nishihara K (2017)Percutaneous Trans esophageal Gastro-Tubing (PTEG) as an AlternativeLong Term TubeFeeding Procedure When Gastrostomy Is Not Feasible. Therap Adv Gastroenterol 10: 911-917.
- Aramaki T, Arai Y, Takeuchi Y, Sone M, Sato R, et al. (2020) A Randomized, Controlled Trial of the Efficacy of Percutaneous Transesophageal Gastro-Tubing (PTEG) as Palliative Care for Patients with Malignant Bowel Obstruction: The JIVROSG0805 Trial. Supportive Care in Cancer 28: 2563-2569.
- Sanogo ML, Sherk W, Esparaz A, Marko X, Gemmete JJ (2020) Shields J Percutaneous Transesophageal Access for Enteral Feeding Tube Placement. Cardiovasc Intervent Radiol 43: 155-161.
- 02315-5 Selby D, Nolen A, Sittambalam C, Johansen K, Pugash R (2019) Percutaneous Transesophageal Gastrostomy (PTEG): ASafe and Well-Tolerated Procedure for Palliation of End-Stage Malignant Bowel Obstruction. Journal of Pain and SymptomManagement J Pain Symptom Manage 58: 306-310.
- Aramaki T, Arai Y, Inaba Y, SatoY, Saito H, et al. (2013) Phase II Study of Percutaneous Transesophageal Gastrotubing for Patients with Malignant Gastrointestinal Obstruction; JIVROSG-0205. Journal o2fVascular and Interventional Radiology 24: 1011–1017.
- Udomsawaengsup S, Brethauer S, Kroh M, Chand B(2008) Percutaneous Transesophageal Gastrostomy (PTEG): A Safeand Effective Technique for Gastrointestinal Decompression in Malignant Obstruction and Massive Ascites. Surg Endosc 22: 2314-2318.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref 365
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Rotellini-Coltvet L, Wallace A, Saini G, Naidu S, Kriegshauser JS, etal. (2023) Percutaneous Transesophageal Gastrostomy (Pteg): An InstitutionalReview and Largest Reported Case Series in the United States (U.S.). J PalliatCare Med 13: 496. DOI: 10.4172/2165-7386.1000496
Copyright: © 2023 Rotellini-Coltvet L, et al. This is an open-access articledistributed under the terms of the Creative Commons Attribution License, whichpermits unrestricted use, distribution, and reproduction in any medium, providedthe original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2180
- [From(publication date): 0-2023 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 1828
- PDF downloads: 352