Research Article Open Access
Percutaneous Tibial Nerve Stimulation for Treatment of Idiopathic Faecal Incontinence: Mid-term Results from a Single Center
Angela Inviati*, Silvia Di Giovanni, Roberto Gullo, Domenico Schifano, Giulia Bonventre, Valentina Di Paola, Gaspare Gulotta and Sebastiano Bonventre
Department of Surgical and Oncological Sciences, University of Palermo, Via L. Giuffrè 5, 90127 Palermo, Italy
- Corresponding Author:
- Angela Inviati
Department of Surgical and Oncological Sciences
University of Palermo, Via L. Giuffrè 5, 90127 Palermo, Italy
Tel: 0039 3396085629
E-mail: surgeryangela@hotmail.it
Received Date: February 23, 2016; Accepted Date: March 08, 2016; Published Date: March 15, 2016
Citation: Inviati A, Giovanni SD, Gullo R, Schifano D, Bonventre G, et al. (2016) Percutaneous Tibial Nerve Stimulation for Treatment of Idiopathic Faecal Incontinence: Mid-term Results from a Single Center. J Gastrointest Dig Syst 6:401. doi:10.4172/2161-069X.1000401
Copyright: © 2016 Inviati A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Objective: Percutaneous tibial nerve stimulation is a recent and minimally invasive treatment for faecal incontinence (FI). The aim of this study is to evaluate the mid-term results in patients with idiopathic faecal incontinence (IFI).
Methods: Fifty one patients (42 female and 9 male) were prospectively recruited. Patients were treated twice a week for 6 weeks as per study protocol. We have assessed the degree of fecal incontinence using the Cleveland Clinic faecal incontinence (CCF-FI) score at baseline, at 6 weeks, at 6 months and at 1 year. Also the anorectal manometric data (mean resting pressure (MRP), squeeze pressure (SP) and, rectal sensation) at baseline, at 6 weeks and at 6 months have been evaluated.
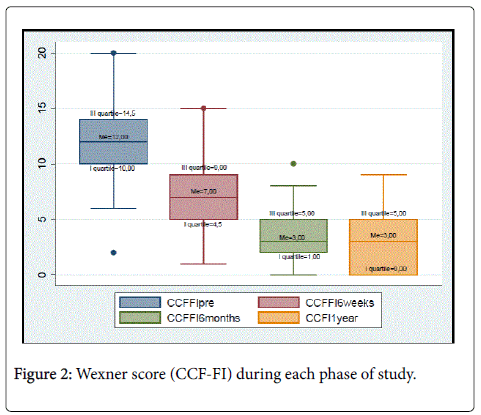
Results: The median CCF-FI score was significantly decreased from an initial baseline value from 12 to 7 at 6 weeks, 3 at 6 months and, 3 at 1 year (respectively: 1st interquartile 4.5, 1, 0 vs 10; 3rd interquartile 9, 5, 5 vs 14.5, p = 0.0001). Anorectal manometry showed an improvement of the internal (resting pressure, MRP) and the external sphincters (squeeze pressure, SP) at 6 months compared to the baseline and 6 weeks by PTNS, while, RP and SP at 6 months was greater than at baseline and 6 weeks (p = 0.004 and p = 0.002 respectively).
Conclusions: This study demonstrates that stimulation of the posterior tibial nerve could be an excellent procedure for the treatment of IFI. The stimulation of the posterior tibial nerve can improve the fecal continence (CCF-FI score) in the short term and this improvement is maintained after 1 year of follow-up without treatment.
Keywords
Idiopathic faecal incontinence; Posterior tibial nerve stimulation; Treatment
Introduction
Fecal incontinence (FI) is defined as the involuntary loss of feces or flatus. It has been underestimated because its existence is often kept secret by patients [1]. It is a common condition affecting approximately 2-20% of the adult population in the western world, with a female: male ratio of 6:1 [2], and mostly affecting women over the age of 65. FI is caused by the disturbance or disruption of the various mechanism of the sphincter musculature and its associated nerve supply, usually following obstetric or anal surgery, trauma, altered rectal sensation and/or colonic dysmotility. The prevalence of idiopathic faecal incontinence (IFI) is unknow; a Canadian study has reported a prevalence of 2%, with no gender preference, and with a mean age of affected individuals of 47 years [3]. Internal anal sphincter (IAS) functionally weakness and rectal sensory disturbances contribute to IFI. Intrapartum anal sphincter injury is the causative factor most commonly implicated in FI in women [4,5]. However, most women who sustain anal sphincter injury during vaginal delivery do not go on to develop FI. Moreover, it is unclear why women who generally sustain obstetric trauma in the second to third decade develop FI several decades thereafter [6]. These observations and other objective assessments of anorectal functions suggest that other risk factors and/or disturbances of anorectal functions contribute to the pathophysiology of this disorder. Thus patients with IFI may also have exaggerated or reduced rectal sensation, and exaggerated anal sphincter relaxation [7,8]. Its management consists in conservative treatment such as medical treatment (antidiarrheal medication) and/or invasive surgery (injection of bulking agents, radiofrequency ablation, implantation of a neosphincter). Although this kind of treatment may be helpful, a considerable number of patients require interventional treatment. Owing to the frequent failure of sphincteroplasty or artificial sphincter implantation, the technique of neuromodulation has been developed during the last decade. Sacral neuromodulation (SNM) has achieved success rates of 60–70% [9,10] but is not free of complications and also requires the implantation of a non-rechargeable pulse generator. More recently, posterior tibial nerve stimulation (PTNS) has been developed as a simple, noninvasive and less expensive alternative to SNM [11]. It has been shown that PTNS has achieved adequate success rates, the treatment is not yet generally available and studies have mostly reported mid-term results [12]. The aim of this study is to evaluate the mid-term results of posterior tibial nerve stimulation in patients with idiopathic faecal incontinence (IFI).
Materials and Methods
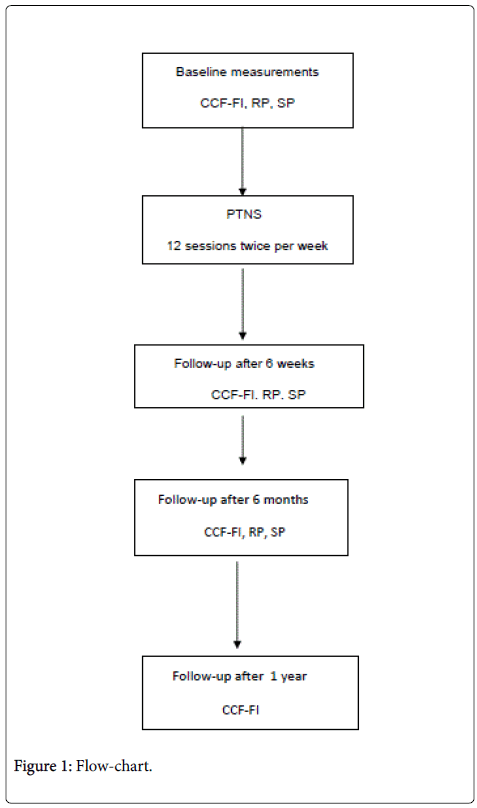
Before starting ethical approval has been obtained (Pr. 8/11, CE Palermo). From January, 2012 to September, 2014, 51 patients with idiopathic FI (42 female and 9 male, mean age 64.54 ± 11.18 years, range 33-80) were prospectively recruited at the University of Palermo’s Digestive Motility Department. The criteria for inclusion were age between 18 and 80 years, severe FI with a Wexner score of 8 or higher, more than 4 episodes of faecal leakage during a period of 28 days as recorded by the patient in a diary, duration of FI longer than 6 months, failure of conservative treatment (drug, biofeedback or bulking agents) and integrity anatomical of the external anal sphincter (EAS) and internal anal sphincter (IAS) by endoanal ultrasound. The criteria for exclusion were: severe cardiopulmonary disease, lesion of the tibial posterior nerve, underlying neurological disorders (e.g., multiple sclerosis, spinal cord injury, spina bifida, stroke, etc), severe venous insufficiency of the lower limbs, inflammatory bowel disease, diabetes, cardiac pacemaker or implantable defibrillator, immunosuppression, anal fissure, anal fistula or abscess, previous anal or pelvic surgery and pregnancy. Endoanal ultrasound and pudendal nerve latency were performed in all patient pre-PTNS to exclude anal sphincter and nerve injury. Then, all patients have a passive faecal incontinence without an anal sphincter defect. Before treatment (pre- PTNS) all patients were given a CCF-FI score (graded 0-20; with 0 = perfect continence and, 20 = complete incontinence). Their scores were revised respectively after 6 weeks, 6 months and 1 year from end of the PTNS cycle (Figure 1). Anorectal manometry was performed to determine anal resting and squeeze pressure pre-PTNS and also 6 weeks and 6 months post-PTNS. Rectal sensibility was estimated by the patient’s perception of distension of a latex balloon introduced through the anus pre-PTNS and 6 weeks and 6 months post-PTNS. Anal manometry was performed, using, a step-by-step pull-through technique, with Narco Bio System MMS 200 manometer (International Biomedical Inc, Austin, Texas) equipped with 8 electrodes connected to an International Biomedical Model 745-0100 (International Biomedical Inc, Austin, Texas), pneumo-hydraulic capillary infusion system with 8 perfusional channels. BEL UDMA20MZ manometric probes (Bioengineering Laboratories Spa, Italy) were used in various combinations with an open-end tip provided with 4 helical side-holes spaced at 1 cm from one another. This was used to determine resting pressure (MRP, mmHg), pressure maximum voluntary or squeeze pressure (SP, mmHg) and rectal sensation (threshold volume for first sensation and desire to defaecate, in ml). The procedure was standardised. The PTNS was performed using the Urgent PC Neuromodulation System (Uroplasty, Geleen, Netherlands). Stimulation was delivered unilaterally using a percutaneous electrode with the patient in the supine position. A 34-gauge stainless steel needle was inserted through the skin approximately 3-4 cm above the medial malleolus between the posterior margin of the tibia and the soleus muscle tendon. An adhesive earth electrode was placed on the same leg near the arch of the foot (Stoller’s Technique). Both needle and electrode were connected to a stimulator with an adjustable pulse intensity (0–10 mA). Fixed parameters included a pulse width of 200 Is and a frequency of 20 Hz. The stimulator contained a 9 V battery. The amplitude was slowly increased until plantar flexion of the large toe or fanning of the other toes occurred. In most patients, the motor response was accompanied by a sensory response felt as a radiating sensation spreading through the sole of the foot. The intensity of stimulation was set at a level that was well-tolerated.
Elevation of the level of intensity of stimulation was allowed whenever the sensation faded owing to adaptation. The treatment protocol consisted of 12 sessions twice per week, with each session lasting 30 minutes.
Statistical Analysis
Continuous variables and CCF-FI scores are summarized as media and standard deviation, median and 1st and 3rd interquartiles. The non-parametric Friedman test was used for continuous variables in multiple comparisons. A p value of less than 0.05 was considered statistically significant. All statistical analyses were done with XLSTAT version 7.5.
Results
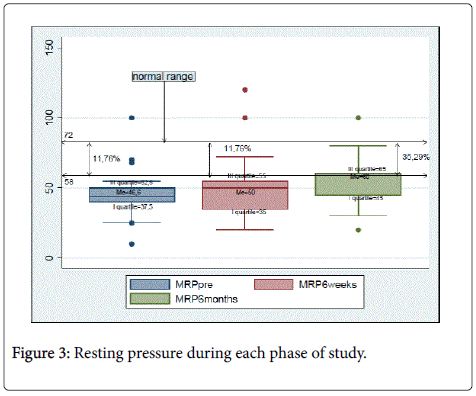
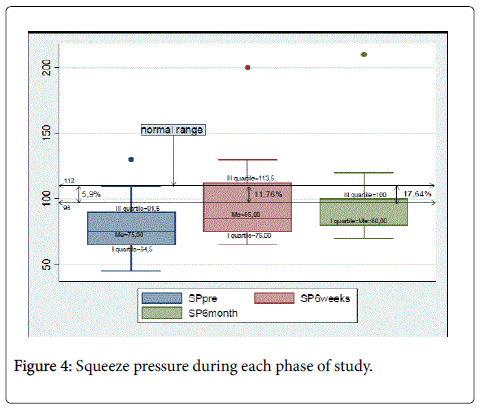
Table 1 shows the manometric data and Wexner score (median and standard deviation) obtained during each phase of the study. There was a significant reduction of symptoms of incontinence (CCF-FI) from baseline at 6 weeks, 6 months and at 1 year. The median CCF-FI score was significantly decreased from a baseline of 12 (mean score 12 ± 4.05) to 7 (mean score 6.94 ± 3.35) at 6 weeks, 3 (mean score 3.7 ± 2.84) at 6 months and, 3 (mean score 3 ± 2.69) at 1 year (respectively: 1st interquartile 4.5, 1, 0 vs 10; 3rd interquartile 9, 5, 5 vs 14.5, p = 0.0001) (Figure 2). The anorectal manometry showed an improvement functional of the internal sphincter (resting pressure, MRP) and the external sphincter (squeeze pressure, SP) at 6 months compared to 6 weeks and the baseline by PTNS; MRP at 6 months was greater than at 6 weeks and baseline (median respectively 60 and 50 mmHg vs 46.6; 1st interquartile 45 and 35 mmHg mmHg vs 37.5; 3rd interquartile 65 and 55 mmHg vs 52.5, p = 0.004). In fact, at the beginning of the PTNS only 11.76% of patients had a MRP within the normal range and after 6 months of treatment the 35.29% had a MRP within the range (Figure 3). SP at 6 months was greater than 6 weeks and at baseline (median, respectively: 80 and 85 mmHg vs 75; 1st interquartile 80 and 75 mmHg mmHg vs 64.5; 3rd interquartile 100 and 113.5 mmHg vs 91.5, p= 0.002) (Figure 4).
| Median | Standard Deviation (SD) | P value | |
|---|---|---|---|
| Age | 65.5 | ± 11.18 | |
| CCF-FI | 12 | ±4.05 | |
| Pre | |||
| CCF-FI | 7 | ±3.35 | |
| 6 weeks | |||
| CCF-FI | 3 | ±2.84 | |
| 6 months | |||
| CCF-FI 1 year | 3 | ±2.69 | 0.0001 |
| RP | 46.6 | ±20.82 | |
| Pre | |||
| RP | 50 | ±24.33 | |
| 6 weeks | |||
| RP | 60 | ±18.93 | 0.004 |
| 6 months | |||
| SP | 64.5 | ±21.82 | |
| Pre | |||
| SP | 85 | ±32.8 | |
| 6 weeks | |||
| SP | 80 | ±32.35 | 0.002 |
| 6 months |
Table 1: Median and DS of manometric data and Wexner score.
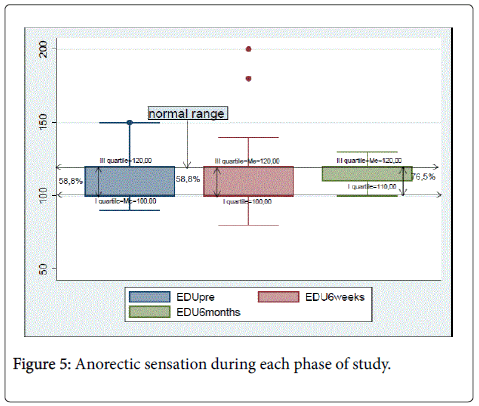
There were no statistically significant differences of anorectal sensation at baseline, 6 weeks and 6 months. However the anorectal sensation improved at 6 months in 70.5% of patients compared to 58.8% at baseline and 6 weeks (Figure 5).
Discussion
This study demonstrates that stimulation of the posterior tibial nerve could be an excellent procedure for the treatment of IFI. Our study showed an improvement in the fecal continence (CCF-FI score) in the short term, after 6 weeks and 6 months from PTNS, and that this improvement is maintained after 1 year of follow-up without treatment. Furthermore the manometric data showed that the PTNS increases the resting pressure and maximum squeeze pressure, to according the previous study [13]. However, we do not have the oneyear manometric data due to refusal of patients to rerun manometry. The resting anal pressure was considered as a measure of internal anal sphincter (IAS) function while the squeeze pressure was considered as a measure of external anal sphincter function. It has been shown in various studies that resting anal pressures and squeeze pressures correlate well with internal anal sphincter and external anal sphincter function respectively. The normal value IAS pressure is 58-72 mmHg; the normal value EAS pressure is 100-180 mmHg. The internal anal sphincter (IAS) provides the greater contribution to resting anal pressure but the vascular tissue of the anal mucosa and submucosa (the anal cushions) may also be important by facilitating hermetic closure of the anal canal . A weak or disrupted IAS or damage to the anal mucosa or submucosa may lead to passive faecal incontinence where incontinence episodes occur without patient awareness. Passive faecal incontinence is the involuntary loss of faeces without the urge to defecate and is predominantly associated with IAS dysfunction. The causes of IAS dysfunction can be classified into two main groups: one type is a morphologically intact but functionally weak IAS (a phenomenon which may occur with age as part of sclerotic degeneration) and the second type is a structurally damaged IAS, which may occur following anal dilatation or ano-rectal surgery, particularly where the IAS has been deliberately divided for a sphincterotomy in the treatment of chronic anal fissure. We have recruited, as mentioned in the materials and methods section, patients with morphologically intact IAS.
Therefore this method offers excellent results compared with surgery by reducing the number and severity of incontinence episodes as expressed by CCF-FI scores, through the improvement of the anal sphincters function. Tibial nerve stimulation was first used in urology to treat urge-incontinence and overactive bladder syndrome [14,15]. The exact mechanism of PTNS is unknown but some studies showed, as the current study, an increase in maximal squeeze pressure suggesting facilitation of striated muscle function [16]. Increased rectal sensitivity to balloon distention suggests that peripheral neuromodulation affects afferent sensory nerves. The tibial nerve borns from the same sacral nerve roots stimulated by sacral nerve stimulation (SNM) [17]. Cortical changes during PTNS have been described, suggesting an important role for the central nervous system. Positron emission tomography (PET) has shown that SNM increases blood flow centrally and it seems that activity in some brain areas can be changed after chronic stimulation [18].
Finazzi-Agro et al. [19] were the first to demonstrate by somatosensitive evoked potentials that a plastic cortical-level reorganization could be the mechanism of action after peripheral stimulation, and they reported close relation-ships between the P100 wave amplitude and possible clinical improvement, so that patients with a better response to treatment had higher wave amplitudes. One aspect that has not yet been clarified is the time over which clinical improvement is maintained in patients who initially respond to PTNS. The optimal treatment protocol for IFI is not known. Various different frequencies have been described in literature, varying from daily for 3 months to every other day for 4 weeks [20]. In most series with high success rates, follow-up is not adequate. There are two studies reporting a success rate of 100%, but with only 1 month of follow-up [21-22]. Follow-up is usually < 10 months in most publications. It is therefore not possible to draw conclusion from these on the duration of relief of symptoms nor on the need for retreatment. In conclusion, our study, going over 10 months, showed medium term improvements in CCF-FI score and anal manometry in patients treated with PTNS.
References
- De la Portilla F, Laporte M, Maestre MV, Díaz-Pavón JM, Gollonet JL, et al. (2013) Percutaneous neuromodulation of the posterior tibial nerve for the treatment of faecal incontinence-mid-term results: is retreatment required? Colorectal Disease 16: 304-310
- Perry S, Shaw C, McGrother C, Matthews RJ, Assassa RP, et al. (2002) Prevalence of faecal incontinence in adults aged 40 years or more living in the community.Gut 50: 480-484.
- Ilnyckyj A (2010) Prevalence of idiopathic fecal incontinence in a community-based sample.Can J Gastroenterol 24: 251-254.
- Sultan AH, Kamm MA (1997) Faecal incontinence after childbirth.Br J Obstet Gynaecol 104: 979-982.
- Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI (1993) Anal-sphincter disruption during vaginal delivery.N Engl J Med 329: 1905-1911.
- Rao SS (2004) Pathophysiology of adult fecal incontinence.Gastroenterology 126: S14-22.
- Sun WM, Donnelly TC, Read NW (1992) Utility of a combined test of anorectal manometry, electromyography, and sensation in determining the mechanism of 'idiopathic' faecal incontinence.Gut 33: 807-813.
- Sørensen G, Liao D, Lundby L, Fynne L, Buntzen S, et al. (2014) Distensibility of the anal canal in patients with idiopathic fecal incontinence: a study with the Functional Lumen Imaging Probe.Neurogastroenterol Motil 26: 255-263.
- Dudding TC, Hollingshead JR, Nicholls RJ, Vaizey CJ (2011) Sacral nerve stimulation for faecal incontinence: patient selection, service provision and operative technique. Colorectal Dis 13: 187-195.
- Maeda Y, Matzel K, Lundby L, Buntzen S, Laurberg S (2011) Postoperative issues of sacral nerve stimulation for fecal incontinence and constipation: a systematic literature review and treatment guideline. Dis Colon Rectum 54: 1443-1460.
- Klingler HC, Pycha A, Schmidbauer J, Marberger M (2000) Use of peripheral neuromodulation of the S3 region for treatment of detrusor overactivity: a urodynamic-based study.Urology 56: 766-771.
- Hotouras A, Murphy J, Walsh U, Allison M, Curry A, et al. (2014) Outcome of percutaneous tibial nerve stimulation (PTNS) for fecal incontinence: a prospective cohort study.Ann Surg 259: 939-943.
- López-Delgado A, Arroyo A, Ruiz-Tovar J, Alcaide MJ, Diez M, et al. (2014) Effect on anal pressure of percutaneous posterior tibial nerve stimulation for faecal incontinence. Colorectal Dis 16: 533-537.
- Van der Pal F, Van Balken MR, Heesakkers JP, Debruyne FM, Bemelmans BL (2006) Percutaneous tibial nerve stimulation in the treatment of refractory overactive bladder syndrome: is maintenance treatment necessary? BJU Inter 97: 547-550
- Wein AJ (2003) Posterior tibial nerve stimulation in the treatment of urge incontinence.J Urol 169: 2429-2430.
- Jarrett ME, Varma JS, Duthie GS, Nichols RJ, Kamm MA (2004) Sacral nerve stimutation for fecal incontinence in the UK. Br J Surg 91: 755-761.
- Agur A, Dalley A (2009) Atlas of Anatomy. Williams & Wilkins, Lippincott.
- Findlay JM, Maxwell-Armstrong C (2011) Posterior tibial nerve stimulation and faecal incontinence: a review.Int J Colorectal Dis 26: 265-273.
- Finazzi-Agrò E, Rocchi C, Pachatz C, Petta F, Spera E, et al. (2009) Percutaneous tibial nerve stimulation produces effects on brain activity: study on the modifications of the long latency somatosensory evoked potentials. Neurourol Urodyn 28:320-324.
- Shafik A, Ahmed I, El-Sibai O, Mostafa RM (2003) Percutaneous peripheral neuromodulation in the treatment of fecal incontinence.Eur Surg Res 35: 103-107.
- Mentes BB, Yüksel O, Aydin A, Tezcaner T, Leventoglu A, et al. (2007) Posterior tibial nerve stimulation for faecal incontinence after partial spinal injury: preliminary report. Tech Coloproctol, 11:115-119.
- Findlay JM, Yeung JM, Robinson R, Greaves H, Maxwell-Armstrong C (2010) Peripheral neuromodulation via posterior tibial nerve stimulation - a potential treatment for faecal incontinence?Ann R Coll Surg Engl 92: 385-390.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11424
- [From(publication date):
April-2016 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 10580
- PDF downloads : 844