Case Report Open Access
Percutaneous Cryoablation for the Treatment of Renal Cell Carcinoma with Paraneoplastic Manifestations
May Jean Counsilman1, Michael J Amirian2, Colette M Shaw3 and Costas D Lallas2*
1Jefferson Medical College, Philadelphia, PA, USA
2Department of Urology, Thomas Jefferson University, Philadelphia, PA, USA
3Department of Radiology, Thomas Jefferson University, Philadelphia, PA, USA
- Corresponding Author:
- Lallas CD
Department of Urology
Thomas Jefferson University
Philadelphia, PA
Tel : (215) 955-6961
E-mail: Costas.lallas@jefferson.edu
Received date:June 20, 2014; Accepted date: August 25, 2014; Published date: September 02,2014
Citation: Counsilman MJ, Amirian MJ, Shaw CM, Lallas CD (2014) Percutaneous Cryoablation for the Treatment of Renal Cell Carcinoma with Paraneoplastic Manifestations. J Clin Diagn Res 2:109. doi:10.4172/2376-0311.1000109
Copyright: 2014 Counsilman MJ, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Clinical Diagnosis and Research
Abstract
We report on a patient who presented with severe myoclonus as a paraneoplastic syndrome due to a renal cell carcinoma. In a patient who had contraindications against definitive extirpative surgery, this is the first instance in which percutaneous cryoablation was used as a successful treatment for the renal cell carcinoma and neurological manifestations.
Keywords
Renal cell carcinoma; Paraneoplastic syndrome; Cryoablation; Neurologic manifestations; Myoclonus
Introduction
Renal cell carcinoma (RCC) is the third most common genitourinary malignancy, and comprises 80-85% of all primary renal neoplasms [1]. While renal cell carcinoma is historically characterized by the classic triad of hematuria, flank mass, and flank pain, less than 40% of patients present with these symptoms. Instead, RCC is increasingly found incidentally, and approximately 20% of patients diagnosed with RCC present with paraneoplastic syndromes [2]. Paraneoplastic syndromes are a group of disorders caused by a remote effect of cancer through mechanisms other than metastases, metabolic and nutritional abnormalities, infections, or coagulopathies. The phenomenon is mediated by humoral factors excreted by tumor cells or by immune responses against the tumor. Paraneoplastic symptoms associated with RCC include elevated erythrocyte sedimentation rate (ESR), hypertension, cachexia, anemia, pyrexia, abnormal liver function, hypercalcemia, polycythemia, varicocele, and neuromyopathies [3]. We present a case of a patient presenting with a neurologic paraneoplastic syndrome and biopsy-proven RCC who was successfully treated with percutaneous cryoablation
Case report
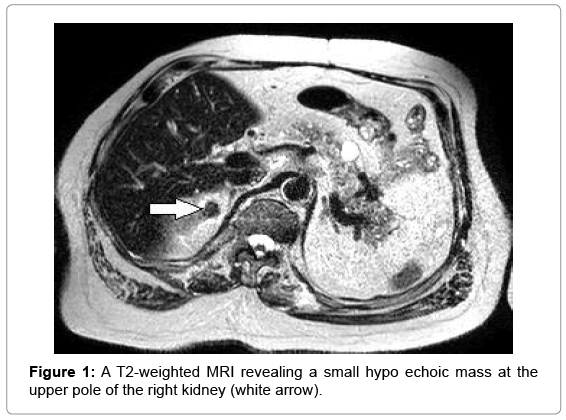
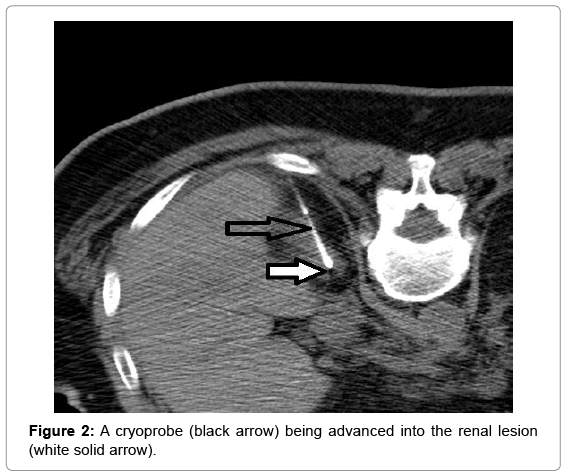
The patient is a 57 year old African-American male with an extensive past medical history, including two previous incidents of renal cell carcinoma treated with two partial nephrectomies, who presented to the Emergency Department with acute mental status change and facial twitching. He had recently been discharged two days prior to this admission from the Neuro intensive care unit (NICU) for status epilepticus and myoclonic jerking. There was a period of lucidity in the Emergency Department before the facial twitching returned, and the patient was unresponsive without return to baseline. After another brief NICU admission with intubation and sedation, an EEG was shown to be diffusely slow with no periodic lateralized epileptiform discharges. Once transferred to the floor, the patient again had an episode of twitching that was thought to be myoclonus, rather than seizure-like activity. An MRI of the brain showed a subtle increased signal on diffusion-weighted images within the mesial temporal lobes that later, on repeat scan, had resolution of the signal change. Myoclonus in conjunction with a negative EEG and resolved MRI suggested a possible paraneoplastic syndrome, which prompted the neurology team to evaluate for an occult malignancy. Work-up included a paraneoplastic autoantibody panel, ultrasound, and a CT of the chest, abdomen, and pelvis. An MRI later revealed a small solid mass in the right kidney measuring 1.5x1.2 cm with decreased T2- weighted signal intensity, suspicious for a papillary renal cell carcinoma Figure 1. The patient was started on intravenous immunoglobulins, and urology was consulted at this time. The supposed RCC was not deemed immediately life-threatening, and because a third ipsilateral nephron-sparing procedure on this patient was thought to be too high-risk, definitive management as an outpatient with cryoablative therapy was proposed. Under interventional radiology’s service, a CTfluoroscopically guided 2.4 mm cryoprobe was advanced into the renal lesion Figure 2. Cryoablation was performed using a standard freeze- thaw-freeze-thaw algorithm, with each freeze period lasting 10 minutes with the temperature of each needle reaching approximately 24 degrees Celsius. The patient then received postablative contrasted MRI scans every 4 months for the last year to confirm successful treatment of the lesion with no new findings. Additionally, he has been symptom-free of myoclonic activity since the initial treatment.
Discussion
Risk factors for a diagnosis of a paraneoplastic neurological disorder include personal or family history of cancer or autoimmunity and a history of smoking [4]. This patient had had two prior RCCs, and we had a high clinical suspicion for a possible carcinoma recurrence. A paraneoplastic antibody screen, a standard basic evaluation when the etiology of myoclonus is unclear, was ordered. The patient’s laboratory results became available several weeks later and were all negative. However, a negative serology does not exclude neurological autoimmunity with or without the associated neoplasia. Therefore imaging for occult malignancy is necessary if no alternative etiology for the myoclonus is found [5]. That was when the third recurrence of RCC was discovered, and treatment options were discussed.
The definitive treatment for RCC, like many cancers, depends on whether the disease is clinically localized or advanced at initial presentation. Surgical resection can be curative for localized disease, which includes stage IA, IB, II and III RCC. When technically feasible, a partial nephrectomy is preferred to preserve renal function. Radiofrequency ablation (RFA) or cryoablation techniques to produce cell tumor death have recently become more common and are a viable alternative to surgery in patients who are otherwise deemed unable to tolerate a surgical procedure, such as the frail elderly population or those with significant comorbidities. Some other indications for thermal ablation to treat RCC include small (<4 cm) masses, or the need for nephron-sparing treatments, such as in a solitary kidney [6]. This patient had extensive comorbidities, including T3 paraplegia from a gunshot wound, syringomyelia, a neurogenic bladder with recurrent urinary tract infections, and hypertension. Because he had undergone two previous partial nephrectomies, we believed that an additional partial nephrectomy would be technically very challenging and percutaneous cryoablation, which has been a proven treatment for cT1a RCC at this institution for the last five years, was instead selected.
Surprisingly, despite the severity of the neurological manifestations from the presumed paraneoplastic syndrome, the symptoms have not returned to date since treatment of the renal mass. This is the first instance that the authors know of in which renal cell carcinoma with neurological paraneoplastic symptoms has been treated with a cryoablative technique rather than a more conventional extirpative procedure. While there have been many studies on these newer nephron-sparing treatments, such as cryoablation and RFA, as options to treat renal cell carcinoma, there have been no reports of these techniques to treat paraneoplastic syndromes from neoplasia.
Conclusion
We present the successful treatment of a small RCC associated with a paraneoplastic syndrome with neurological manifestation with percutaneous cryoablation.
Acknowledgements
We thank Michael Sperling, MD of the Department of Neurology at Thomas Jefferson University for his involvement in patient care and for his supportive scientific discussion on paraneoplastic syndromes
References
- McDougal Ws, Garnick MB (1995) Clinical signs and symptoms of renal cell carcinoma:Comprehensive Textbook of Genitourinary Oncology Edited by NJ,Vogelzang PT, Scardino WU, Shipley ,Coffeey DS Baltimore. Williams & Wilkins Co154-159 and 111-115.
- Kim HL, Belldegrun AS, Freitas DG, Bui MH, Han KR et al. (2003) Paraneoplastic signs and symptoms of renal cell carcinoma: Implications for prognosis.J Urol 170: 1742-1746.
- Ding G X, Song NH, Feng CC, Xia GW, Jiang HW, et al. (2012) Is there an association between advanced stage of renal cell carcinoma and paraneoplastic syndrome?Medical Principles and PracticeMed PrincPract21: 370-374.
- McKeon A, Pittock SJ (2011)Paraneoplasticencephalomyelopathies: Pathology and mechanisms.ActaNeuropatholCommun 122: 381-400.
- Pelosof LC, Gerber DE (2010) Paraneoplastic syndromes: An approach to diagnosis and treatment.Mayo ClinProc85: 838-854.
- Onishi T, Nishikawa K, Hasegawa Y, Yamada Y, Soga N, et al. (2007) Assessment of health-related quality of life after radiofrequency ablation or laparoscopic surgery for small renal cell carcinoma: A prospective study with medical outcomes study 36-item health survey (SF-36).Jpn J ClinOncol37: 750-754.
Relevant Topics
- Back Pain Diagnosis
- Cardiovascular Diagnosis
- Clinical Diagnosis
- Clinical Echocardiography
- COPD Diagnosis
- Diabetes Diagnosis
- Diagnosis Methods
- Diagnosis of cancer
- Diagnosis of CNS
- Diagnosis of Diabetes
- Diagnostic Products
- Diagnostics Market Analysis
- Heart diagnosis
- Immuno Diagnosis
- Infertility Diagnosis
- Medical Diagnostic Tools
- Preimplementation Genetic Diagnosis
- Prenatal Diagnostics
- Ultrasonography
Recommended Journals
Article Tools
Article Usage
- Total views: 14359
- [From(publication date):
December-2014 - Jul 13, 2025] - Breakdown by view type
- HTML page views : 9752
- PDF downloads : 4607