Pattern and Significance of Ocular Injuries Associated with Orbito- Zygomatic Fractures
Received: 30-May-2018 / Accepted Date: 12-Jun-2018 / Published Date: 19-Jun-2018
Keywords: Ophthalmic injuries; Orbito-zygomatic fracture; Orbital blow out fracture
Introduction
The face, orbit, and eyes have a relatively prominent position in the human body making this area more susceptible to trauma. A variety of ophthalmic injuries associated with mid-facial fractures has been reported in the literature [1]. Motor-vehicle accidents, as sault, falling down injuries, occupational, and sport accidents are generally considered as common etiologies of maxillofacial fractures [2].
Zygomatic fractures are the most common facial fractures second only to nasal fractures and these fractures are also the most commonly occurring fractures of the orbit [3]. There is a recognized association between orbitozygomatic fractures and ocular injuries. The reported incidence of ocular injuries in patients with orbital fractures varies widely, ranging from 2.7% to 90% [1,4]. Al-Qurainy et al. developed criteria for appropriate referral to an ophthalmologist. The authors proposed the acronym “BAD ACT,” to represent Blowout, Acuity, Diplopia, Amnesia, and Comminuted Trauma, as a method for easy recall. However, the system is not commonly used in clinical practice [5]. The severity of an injury is related to the site of the fracture and direction of the incoming force. The outcome may range from mild injury such as sub-conjunctival hemorrhage (SCH) to severe damage like globe rupture or permanent visual loss [1,4].
Ophthalmic injuries can be divided into minor and major groups based on the possibility of causing permanent visual loss [5]. Subconjunctival hemorrhage (SCH), peri-orbital ecchymosis, ptosis, crepitation, and laceration of the eyelids are considered as minor injuries. Laceration of the sclera and cornea, ophthalmic infection, traumatic injury of the optic nerve, globe rupture, limitation of eye movements, enophthalmos, proptosis, blurred vision, diplopia, retinal hemorrhage, hyphema and permanent visual loss are categorized as major injuries.
Early diagnosis of potentially serious ophthalmic injuries is paramount not only in minimizing long-term complications of midfacial fractures but also from a medico-legal standpoint. The management of the ophthalmic injuries must be considered as the first priority. Repairing the fractures before treatment of ophthalmic injuries may further compromise visual outcomes, leading to visual loss [5].
Signs and symptoms are usually helpful in diagnosing ophthalmic injuries, but occasionally due to the severity of the incoming trauma, patients may not able to describe their symptoms as they maybe unconscious or intubated [6]. Therefore, considering the fact that potentially serious ophthalmic injuries may ensue in mid-facial fractures, and may inadvertently be overlooked, a retrospective study was designed to evaluate the prevalence of such injuries and their correlations in patients admitted to King Fahad Hospital at Almadina Almunawara from 2014 to 2017.
Patients and Methods
This is a retrospective study of patients presenting with orbitozygomatic bone fractures admitted to Maxillofacial Surgery Department at King Fahad Hospital in Almadinah Almunawara, Saudi Arabia from 2012 to 2017. Patients with isolated zygomatic arch fractures or concomitant midfacial fractures were excluded from the study.
Fractures were diagnosed clinically. The extent of the bony injury was confirmed with computerized tomographic scans (CT). Patient demographics, date of injury, date of presentation to the hospital, fracture etiology, brain injuries status and clinical ocular signs were recorded.
All patients were examined by the ophthalmologist preoperatively, and if needed were also followed up postoperatively. On the basis of clinical examination and pre-treatment, radiograph/CT scan result, the study population was divided into 3 subgroups based on the extent of the bony injury.
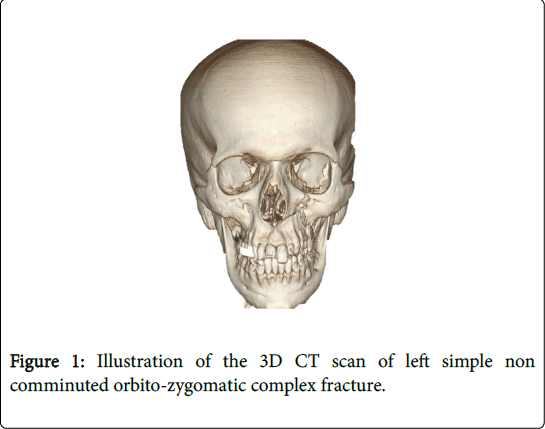
Group-1 consisted of non-comminuted fractures designated as “simple” for the purpose of this study (Figure 1).
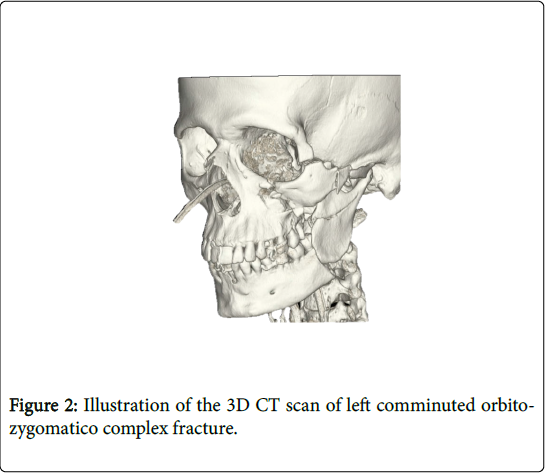
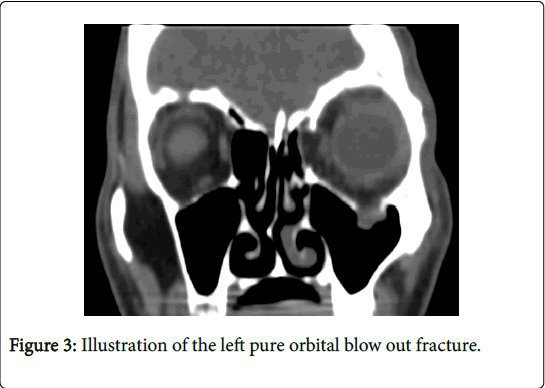
Group-2 was comminuted orbitozygomatic fractures (Note the quadripod fracture at frontozygomatic sutre, zygomatico maxillary sutre, zygomatic arch and orbital floor) (Figure 2). Group-3 was “pure” orbital blowout fractures, involving the floor or medial wall of the orbit and with no associated zygomatic complex fracture (Note the herniation of inferior rectus muscle) (Figure 3).
Results
The study population included 156 patients (142 male and 14 female). There was a peak in incidence for adult compared to female accounting for 91% of the fractures as shown in Table 1.
| Age | Gender | Total | |
|---|---|---|---|
| Male | Female | ||
| Child | 26 | 3 | 29 |
| Adult | 116 | 11 | 127 |
| Total | 142 | 14 | 156 |
Table 1: Male-female cross-tabulation.
Road traffic accident was the most commonly documented mechanism of injury, accounting for 79.5% (n=124) of the fractures, followed by fall down injuries (18%, n=11.5), explosion (0.6%, n=1), assault (4.5%, n=7), and gunshot (0.6%, n=1). This is summarized in Table 2.
| Variables | Frequency | Percentage (%) |
|---|---|---|
| Road traffic accident | 129 | 82.7 |
| Explosion | 1 | 0.6 |
| Assault | 7 | 4.5 |
| Fall down | 18 | 11.5 |
| Gun shot | 1 | 0.6 |
| Total | 156 | 100 |
Table 2: Details about road traffic accidents.
Group-1 (“simple” fractures) accounted for 67.3% (n=105) of the patients, Group-2 (“comminuted” fractures) accounted for 23.7% (n=37), and Group-3 (“orbital blowout”) for 9% (n=14). All orbitozygomatic fractures were unilateral.
There were 2 ocular findings in Group-1 (1.9%). Complete visual loss occurred in one patient. The other patient had mild diplopia. There were 15 ocular findings (n=37, 40.5%) in Group-2.
Resolution occurred in 10 patients. Three patients had permanent visual loss. One has mild exophthalmos and one patient presented with oculomotor nerve neuropathy. There were 7 ocular findings (n=14, 46.6%) in Group-3.
Resolution occurred in 6 patients. One had persistent non disabling diplopia at the extremes of visual field. The data is represented in both Table 3 and 4.
| Variables | Sample size (n) | Percentage (%) |
|---|---|---|
| Zygomatico-maxillary complex fracture | 37 | 23.7 |
| Isolated orbital floor fracture | 14 | 9 |
| Simple non comunuted zygomatico-maxillary fracture | 105 | 67.3 |
| Total | 156 | 100 |
Table 3: Subgroups of zygomatic fractures frequency.
| Category of ocular injury | Type of zygomatic fracture | Total | ||
|---|---|---|---|---|
| Zygomatico-maxillary complex fracture | Isolated orbital floor fracture | Simple noncomunuted zygomatico-maxillary fracture | ||
| Blindness | 3 | 0 | 1 | 4 |
| Free | 22 | 8 | 103 | 133 |
| Occulomotor injury | 5 | 0 | 0 | 5 |
| Rupture globe | 1 | 0 | 0 | 1 |
| Enophthalmos | 5 | 0 | 0 | 5 |
| Diplopia | 0 | 6 | 1 | 7 |
| Exfliated globe | 1 | 0 | 0 | 1 |
| Total | 37 | 14 | 105 | 156 |
Table 4: Frequency of ocular injury associated with zygomatic fracture.
Discussion
Analysis of the data from this retrospective study allows examination of demographic patterns, etiology of injuries, and highlights the ocular morbidity associated with orbitozygomatic trauma. There were no patients in the study population presenting with bilateral orbitozygomatic fractures.
Pan facial and midfacial/nasoethmoid fractures were excluded in order to examine ocular morbidity specifically related to orbitozygomatic fractures. Similar to other studies addressing maxillofacial trauma, there was a peak in incidence for orbitozygomatic fractures in adult males compared to children as shown in Table 1 [7]. Road traffic accident was the most commonly documented mechanism of injury in this study, accounting for 82.7% of patients, followed by fall down (11.5%), and assault (4.5%). This corresponds with other urban trauma studies [8].
The etiology of injury varies geographically: in Western countries with large urban populations, alcohol related assault remains the primary etiologic factor in maxillofacial trauma. However, motor vehicle accidents predominate in many developing countries, in the absence of seat belt legislation and where alcohol-related assault is uncommon [9].
The reported incidence of ocular injuries in patients with orbital fractures varies widely, ranging from 2.7%1 to 90% [2]. The incidence in this study was 14.7%, which is consistent with many other studies. Lower levels reported where ophthalmologic input is absent or only sporadic may indicate that some ocular findings were undetected [3]. On the other hand, variation in reported incidence between studies may represent differences in inclusion criteria.
For example, the 90.6% incidence reported by Al-Qurainy et al. includes subconjunctival hemorrhage as ocular pathology. This is not counted as a significant ocular finding in many other studies, including this study. Furthermore, Al-Qurainy’s study includes all midfacial/ nasoethmoid fractures that were excluded in this study [3].
BAD ACT, scoring system proposed by Al-Qurainy et al. to predict ocular injury risk and therefore allow appropriate referral, is not widely used in clinical practice [6,7]. An estimation of the ocular injury risk associated with specific orbitozygomatic fractures may be useful for assessment of risk. Based on data from this study, “simple fractures” have 2% risk of concomitant ocular finding or injury. However this complication arises from severe brain injuries associated with simple orbito-zygomatic bone fracture.
Comminuted fractures have 40.5% risk (over one third); and blowout fractures a 42.8% risk (over one thirds of patients). We postulate that the varying incidence of ocular finding or injury in the fracture groups (“simple” “comminuted’’, “blow out’’) is related to the mechanism of injury. The higher velocity of impact required to generate a comminuted orbitozygomatic fracture leads to an increased number of ocular findings and injuries in this group when compared with the “simple” fracture group.
The mechanism of injury in orbital blowout fractures has been a source of discussion, but may explain the increased incidence of ocular findings and injuries in the “Blow Out” group. There are 2 main theories, as follows:
• Hydraulic Theory, advocated by Smith and Regan proposes that orbital blowout fractures occur because of a direct impact to the globe. The posterior displacement of the globe leads to an increase in intra-orbital pressure that is relieved by a fracture of the thin walled floor or medial orbital wall. This proposed mechanism should lead to an increased number of direct globe and orbital soft tissue injuries.
• Orbital Rim “Buckling” Theory, investigated by Fujino suggests that the mechanism of injury in blowout fractures is a direct impact to the orbital rim resulting in a distribution of this force throughout the bony orbit with a “buckling” effect and the development of a fracture at a point of weakness, the orbital floor.
The Hydraulic Theory can be adapted to explain both orbital floor and medial wall fractures. However, it is more difficult to assign the Buckling Theory to medial orbital wall fractures, although it does provide an acceptable explanation for floor fractures. As in most clinical matters, a combination of both mechanisms is a probable explanation for orbital blowout fractures.
In this study, the increased numbers of ocular injuries in Group-2 and 3 with high level of significance compared with Groups-1 (revealed in Table 5) would suggest the importance of increased clinical awareness and confirm the need for ophthalmology consultation for these patients. Based on the findings of this study, ocular findings and injuries are a relatively common complication of orbital fractures, occurring in 14.7% of patients (n=23).
| Variables | Sample (n) | 2-sided Pearson Chi-Square | Fisher's Exact Test |
|---|---|---|---|
| Group 1 | 104 | 0.561 | 1 |
| Group 2 | 37 | 0.001 | 0.001 |
| Group 3 | 15 | 0.001 | 0.001 |
| Total | 156 | ||
Table 5: Illustration of the level of significance of Group-1, 2 and 3.
We propose that orbitozygomatic fractures be divided into “simple”/ “noncomminuted” fractures, “comminuted” fractures, and “blowout” fractures, based on clinical and conventional radiographic findings. CT scan should be used to confirm the extent of bony injury, allowing estimation of ocular injury risk.
Ophthalmology consultation is recommended for Group-2 and 3 presenting with orbitozygomatic fractures. Where constraints in available ophthalmology resources exist, preferential referral for comminuted and blowout fractures is recommended based on the high incidence of ocular findings and injuries in these patient subgroups.
Statistical analysis
This study revealed statistically significant made by Group-2 and 3 as predictor for ocular injury as summarized in Table 5.
Analysis of predictors (head injuries and gender) as a contribution factors to ocular injuries are summarized in Tables 6 and 7 using linear regression test. The independent variable as a set accounts for 7% of variance in ocular injuries. The overall regression model was significant. F (1.5.11)=6.4, P value less than 0.05, R square is 0.077. This is illustrated in Table 7.
| Model | R | R Square | Adjusted R Square | Standard error of the Estimate |
|---|---|---|---|---|
| 1 | 0.278a | 0.077 | 0.065 | 0.3439 |
| Note: a: Predictors (Constant), Gender, brain injury | ||||
Table 6: Model Summary.
| Model | Variables | Sum of Squares | df | Mean Square | Frequency | Significance |
|---|---|---|---|---|---|---|
| 1 | Regression | 1.514 | 2 | 0.757 | 6.399 | .002a |
| Residual | 18.095 | 153 | 0.118 | |||
| Total | 19.609 | 155 | 0.875 | |||
| Note: a: Predictors (Constant), Gender, brain injury, b: Dependent Variable (positive cases) | ||||||
Table 7: Illustration of the ANOVA test.
The role of Pharmacological treatment for orbito-zygomatic bone fracture
Ice packs and head elevation are recommended for the Patient with orbital floor fracture for 48 hours to reduce the swelling [10,11]. Moreover, Patient should be informed not to blow the nose to prevent the emphysema for 4 to 6 weeks after the injury.
Patient with limited ocular movements may benefit from short term use of steroids (0.75-1 mg/kg per day of prednisone) if not contraindicated. Steroids treatment helps for peri orbital and extra ocular muscle edema to subside quickly and helps to decide whether this limited ocular movement is transient or if surgery is needed. Nasal decongestant and antibiotics are advised for one week.
Brain injuries made statistically significant contribution to ocular injuries. However, gender made no contributions as shown in Table 8.
| Coefficientsa | ||||||
|---|---|---|---|---|---|---|
| Model | Unstandardized Coefficients | Standardized Coefficients | Significance | |||
| Beta | Standard Error | Beta | Standard Error | |||
| 1 | Constant | 1.829 | 0.11 | 0 | 16.588 | 0 |
| Brain_injury | -0.266 | 0.077 | -0.27 | -3.471 | 0.001 | |
| Gender | 0.059 | 0.097 | 0.048 | 0.616 | 0.539 | |
| Note: a: Dependent Variable (positive ocular finding) | ||||||
Table 8: Level of significance of independent variable.
Limitations of the study
This study includes only the patient with orbito-zygomatic bone fractures admitted under the maxillofacial surgery department of King Fahad Hospital Almadinah from 2013 to 2017. Other associated fractures around the orbit such as nasoethmoidal and frontal bone fractures can make significant contributions to the ocular complications. This should be included in future studies.
Role of care manager
Research is approved with permission from the King Fahad Hospital ethical committee.
Conclusion
Ocular injuries are a relatively common complication of orbitozygomatic fractures occurring in 23 of patients (14.7%) in this study. These injuries are more frequently seen in patients with comminuted orbito-zygomatic fractures 15 (44%) followed by orbital blowout fractures 6 (42.9%). Although simple zygomatic complex fractures has low incidence (n=2, 1.9%), it associated with major ocular complication if brain injuries present. Ophthalmology consultation and ocular examination of at least three components; visual acuity, ocular movement, and pupil reaction to light are strongly recommended for Group-2 and 3 presenting with orbito-zygomatic fractures.
References
- Karabekir HS, Gocmen-Mas N, Emel E, Karacayli U, Koymen R, et al. (2012) Ocular and periocular injuries associated with an isolated orbital fracture depending on a blunt cranial trauma: anatomical and surgical aspects. J Craniomaxillofac Surg 40: e189-e193.
- Magarakis M, Mundinger GS, Kelamis JA, Dorafshar AH, Bojovic B, et al. (2012) Ocular injury, visual impairment, and blindness associated with facial fractures: A systematic literature review. Plast Reconstr Surg 129: 227-233.
- Al-Qurainy IA, Stassen LF, Dutton GN, Moos KF, El-Attar A (1991) The characteristics of midfacial fractures and the association with ocular injury: A prospective study. Br J Oral Maxillofac Surg 29: 291-301.
- Al-Qurainy IA, Dutton GN, Titterington DM, Stassen LF, Moos KF, El-Attar A (1991) Midfacial fractures and the eye: The development of a system for detecting patients at risk of eye injury. Br J Oral Maxillofac Surg 29: 363-367
- Barry C, Coyle M, Idrees Z, Dwyer MH, Kearns G (2008) Ocular findings in patients with orbitozygomatic complex fractures: A retrospective study. J Oral Maxillofac Surg 66: 888-892.
- Ioannides C, Treffers W, Rutten M, Noverraz P (1988) Ocular injuries associated with fractures involving the orbit. J Craniomaxillofac Surg 16: 157-159.
- MacKinnon CA, David DJ, Cooter RD (2002) Blindness and severvsual impairment in facial fractures: An 11-year review. Br J Plast Surg, 55: 1-7.
- Jamal BT, Pfahler SM, Lane KA, Bilyk JR, Pribitkin EA, et al. (2009) Ophthalmic injuries in patients with zygomaticomaxillary complex fractures requiring surgical repair. J Oral Maxillofac Surg. 67: 986-989.
- He D, Blomquist PH, Ellis E (2007) Association between ocular injuries and internal orbital fractures. J Oral Maxillofac Surg 65: 713-720.
- Nagase DY, Courtemanche DJ, Peters DA (2006) Facial fractures-association with ocular injuries: A 13-year review of one practice in a tertiary care center. Can J Plast Surg 14: 167-171.
- Hung J, Poon KJ, Teo NM, Hing EC, Lee HJ, et al.(2017) Conservative management of isolated orbital floor fractures: A retrospective review in a single institution 1: 261.
Citation: Albeshri H, Ahsan B, Samman M, Abusalama A, Waheed S, et al. (2018) Pattern and Significance of Ocular Injuries Associated with Orbito-Zygomatic Fractures. Cosmetol & Oro Facial Surg 4: 132.
Copyright: © 2018 Albeshri H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Usage
- Total views: 5493
- [From(publication date): 0-2018 - Apr 02, 2025]
- Breakdown by view type
- HTML page views: 4484
- PDF downloads: 1009