Research Article Open Access
Patient and Staff Radiation Exposure during Endoscopic Retrograde Cholangio-Pancreatography: Eight Years of Dose Monitoring
Tsapaki V1, Paraskeva DK1, Giannakopoulos A1, Chatzoglou V2, Nikolopoulos D3*, Angelogiannopoulou P1, Papaeuthimiou S1 and Kottou S21Konstantopoulio General Hospital, Nea Ionia of Athens, Greece
2National and Kapodistrian University of Athens, Medical Physics Laboratory, Athens, Greece
3Piraeus University of Applied Sciences (TEI of Piraeus), Electronic Computer Systems Engineering, Athens, Greece
- *Corresponding Author:
- Nikolopoulos Dimitrios
Piraeus University of Applied Sciences (TEI of Piraeus)
Electronic Computer Systems Engineering, Athens, Greece
Tel: +0030-6977-208318
E-mail: dniko@teipir.gr
Received Date: February 02, 2017; Accepted Date: February 07, 2017; Published Date: February 15, 2017
Citation: Tsapaki V, Paraskeva DK, Giannakopoulos A, Chatzoglou V, Nikolopoulos D, et al. (2017) Patient and Staff Radiation Exposure during Endoscopic Retrograde Cholangio-Pancreatography: Eight Years of Dose Monitoring. OMICS J Radiol 6:253. doi: 10.4172/2167-7964.1000253
Copyright: © 2017 Tsapaki V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Radiology
Abstract
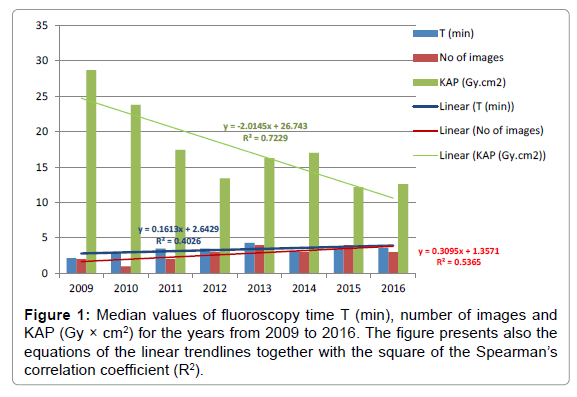
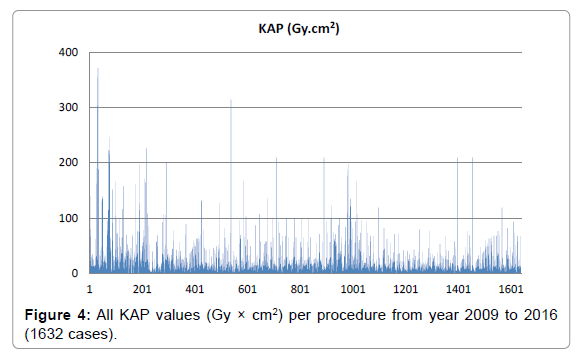
The aim of the study was to analyze eight years of patient and staff radiation exposure data during Endoscopic Retrograde Cholangio-Pancreatography (ERCP). Parameters recorded and calculated were: patient age, kermaarea product (KAP), fluoroscopy time (T) and total number of images (I) in 1632 ERCP procedures. An experienced endoscopist (more than 10 years of practice) performed the ERCPs and was monitored by a thermoluminescent dosemeter worn over a 0.25 mm lead apron. Patient mean (SD) age was 70.6 (14.8) years. Median (max) of KAP value was 15.6 (371.2) Gy.cm2. Median (max) of T and I were 3.3 (50.0) min and 3 (10) images, respectively. Median values of KAP showed a reduction over the eight years, although median values of T and I showed a slight increase during the same period. KAP and T values of the present study appeared to be close to those reported in similar studies in the literature. Monthly endoscopist radiation dose was negligible due to the proper use of lead apron, collar and two leadarticulated ceiling mounted shields (90 cm width each).
Keywords
ERCP; Patient dose; Staff dose; Thermoluminescent
Introduction
Endoscopic Retrograde Cholangio-Pancreatography (ERCP) uses endoscopic and radiological guidance to accomplish diagnosis and therapy of biliary and pancreatic disorders. ERCP is one the most complicated gastrointestinal procedures routinely performed. In addition to endoscopic skills it requires the ability to interpret radiologic images in real time. The American Society for Gastrointestinal Endoscopy (ASGE) and the American College of Gastroenterology (ACG) established a task force in 2006 to create quality metrics for endoscopy including ERCP [1]. Many studies have tried to estimate the radiation dose delivered to patients and medical staff during ERCP procedures, in hospital centers or even more, to establish local Dose Reference Levels (DRLs) [2-12]. Monitoring the doses reported from ERCP procedures is essential; not only in order to optimize the techniques and protocols in each center, but also to manage the probably increasing radiation dose delivered to patients. By definition ERCP requires radiation exposure to the patient which should be kept to the lowest level to allow the procedure to be completed safely in accordance with the “as low as reasonably achievable” principle. During the last decades ERCP had proved to be very useful in diagnosis, however the introduction of new, non-invasive imaging modalities, such as magnetic resonance cholangio-pancreatography and Endoscopic Ultrasonography (EUS), have led the ERCP to be mainly used for therapeutic purposes [13]. ERCP is nowadays mainly a therapeutic endoscopic procedure that under fluoroscopy guidance provides treatment in various benign and malignant diseases of biliary and pancreatic ducts.
There is a wide range of KAP values during ERCP reported in the literature. Although the establishment of DRLs would be very useful in view of the large range of KAP values reported during ERCP, little progress has been made so far. The aim of the present study was to (a) analyze and report eight years of patient and staff radiation exposure data during ERCP procedures, in one hospital, by an experienced single operator and (b) to analyze trends and compare with national and international literature.
Material and Methods
The study was conducted in Konstantopoulio General Hospital (a tertiary center) in Athens. The ERCPs were carried out using an overcouch Philips Essenta X-ray machine (Philips Medical Systems, Best, The Netherlands), with a 30 cm diameter image intensifier and a high-frequency generator. The X-ray equipment has automatic exposure control for radiography, automatic brightness control for fluoroscopy and a last image hold capability. The collimator diaphragms are automatically set to the size of the cassette inserted in the tray and one to three images can be taken in one film (37 × 43 cm). The X-ray machine has a KAP meter installed in the X-ray tube housing. The meter was calibrated according to the method summarised in the ‘National Protocol for patient dose measurements in Diagnostic Radiology’ developed by the National Radiological Protection Board [14].
Data were analyzed for the last eight years (January 2009 - May 2016). Patients referred to the radiology department of the Konstantopoulio Hospital for ERCP examination were included without setting any restrictions on patient weight, sex or clinical condition. Written informed consent was obtained from all patients in accordance with guidelines set forth by the institutional board of the hospital. All ERCP procedures were therapeutic and were done under sedation provided by an anesthesiologist and with a fixed setup for the patient. This meant that each patient remained in the same position, so the same anatomical area was exposed during the entire examination. The techniques were performed by a single endoscopist with 15 years of experience. There was no digression from standard unit practice in terms of the procedures performed. The X-ray equipment was controlled by the radiographer who remained in the control room and performed fluoroscopy and radiography according to the requirements of the endoscopist. The endoscopist was positioned next to the patient, behind two articulated ceiling suspended lead equivalent protective screens, 90 cm wide, during the whole procedure, wearing a two piece (front and back) protection apron 0.25 mmPb equivalent, a lead collar and lead protective glasses. She was also monitored using a Thermoluminescent Dosemeter badge (TLD) provided monthly by the Greek Atomic Energy Commission and worn over the lead apron, according to the Greek Radiation Protection Law to provide an estimation of eye lens radiation dose if needed.
Patient data included age in years, radiation exposure in terms of Kerma-Area Product (KAP, in Gy.cm2), fluoroscopy time (T, in min) and total number of images (I).
Results
The sample included 1632 therapeutic ERCP procedures. Mean (SD) patient age did not change significantly through the years, ranging from 68.1 (15.5) to 74 (13.7) years. Over the years, median values of number of images ranged from 1 to 4, of T from 2.15 to 4.3 min and for KAP from 12.2 to 28.7 Gy.cm2 (Table 1). For staff, the radiation exposure values provided by the authorities were always close to 0 μSv.
| Year | No. of patients | No. of images median | No. of images max | T median (min) |
T mean (min) | T max (min) | KAP median (Gy‚??cm2) | KAP mean (Gy‚??cm2) | KAP max (Gy‚??cm2) |
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 89 | 2 | 4 | 2.15 | 3.64 | 26 | 28.7 | 63.6 | 371.2 |
| 2010 | 185 | 1 | 4 | 3.0 | 4.51 | 24.3 | 23.8 | 34.5 | 226.1 |
| 2011 | 189 | 2 | 4 | 3.5 | 4.73 | 27.5 | 17.4 | 26.0 | 201.3 |
| 2012 | 219 | 3 | 10 | 3.5 | 5.37 | 50 | 13.4 | 23.2 | 314.4 |
| 2013 | 232 | 4 | 9 | 4.3 | 5.59 | 22.2 | 16.3 | 23.9 | 209.3 |
| 2014 | 245 | 3 | 9 | 3.2 | 4.72 | 31.7 | 17.0 | 30.2 | 198.0 |
| 2015 | 222 | 4 | 8 | 3.7 | 4.96 | 24.1 | 12.2 | 16.2 | 79.27 |
| 2016 | 251 | 3 | 9 | 3.7 | 5.18 | 31.7 | 12.6 | 21.4 | 209.3 |
| All years | 1632 | 3 | 10 | 3.5 | 4.96 | 50 | 15.6 | 26.9 | 371.2 |
Table 1: Median and maximum values of number of images and median, mean and maximum values of T and KAP, along with the number of cases per year.
A summary of the results (median, mean and maximum values) is shown in Table 1 and Figure 1. Corresponding minimum values are not included, as they have no practical meaning, especially in studies with large number of cases (unselected), where minimum values are often close to zero.
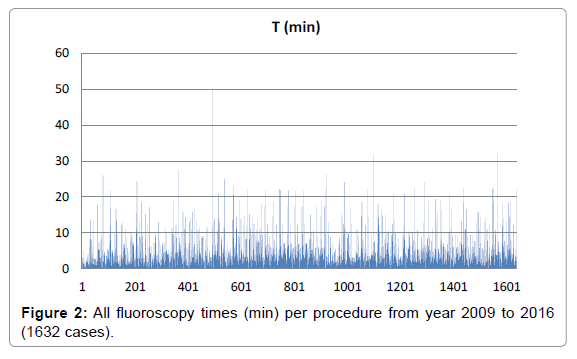
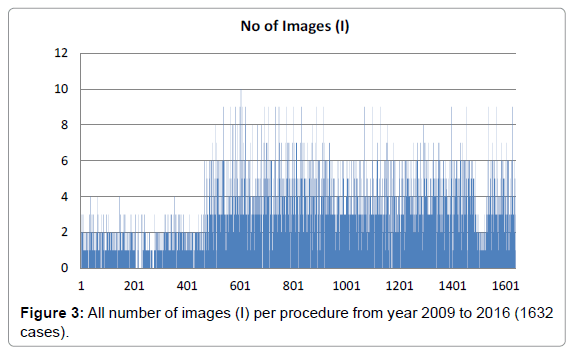
All measured values of T (in min), number of images (I) and KAP (in Gy × cm2) are presented in Figures 2-4 respectively.
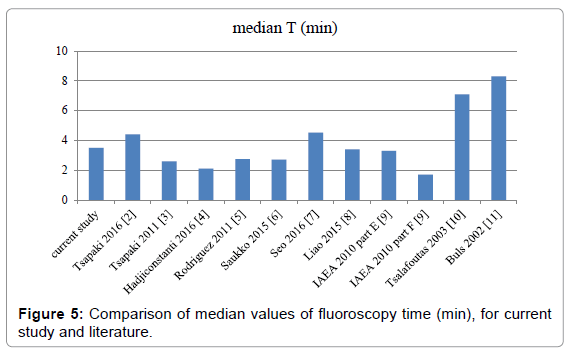
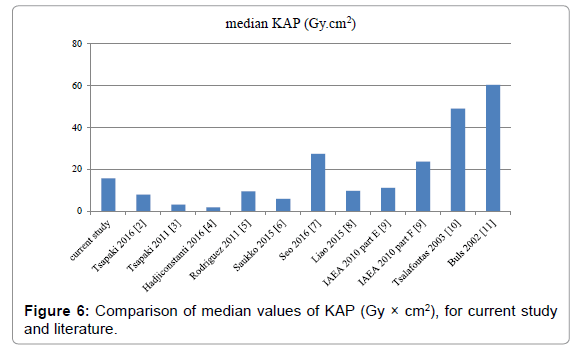
In Table 2 and Figures 5 and 6, the comparison of median values of the quantities T (min) and KAP (Gy.cm2) is presented, between the results of this study and the corresponding results of similar published data.
| Cases | Mesdian T (min) |
Median KAP (Gy.cm2) | |
|---|---|---|---|
| Current study | 1632 | 3.5 | 15.6 |
| Tsapaki et al. [2] | 200 | 4.4 | 7.8 |
| Tsapaki et al. [3] | 157 | 2.6 | 3.1 |
| Hadjiconstanti et al. [4] | 15 | 2.1 | 1.7 |
| Rodriguez et al. [5] | 340 | 2.75 | 9.4 |
| Saukko et al. [6] | 227 | 2.7 | 5.83 |
| Seo et al. [7] | 126 | 4.52 | 27.35 |
| Liao et al. [8] | 331 | 3.4 | 9.56 |
| IAEA part E [9] | 10 | 3.3 | 11.1 |
| IAEA part F [9] | 39 | 1.7 | 23.6 |
| Tsalafoutas et al. [10] | 21 | 7.1 | 48.9 |
| Buls et al. [11] | 54 | 8.3 | 60.3 |
Table 2: Comparison of median T (min) and KAP (Gy.cm2) values with the corresponding values from the literature.
Discussion
ERCP is nowadays mainly a therapeutic endoscopic procedure that under fluoroscopy guidance provides treatment in various benign and malignant diseases of biliary and pancreatic ducts. The use of fluoroscopy is inherent to ERCP. Quality measures reflecting patient radiation exposure during ERCP are needed and as such, I, T and KAP have been recommended to estimate patient radiation exposure. However, there is a great variation in the literature of the reported ERCP KAP values and patient radiation dose values [3,5,6,10,11]. This is reflected in our results too, as it can be seen in Table 1 and Figure 1, although a single, well-experienced endoscopist, using the same X-ray imaging system, performed all 1632 ECRP procedures. Factors affecting radiation dose, in addition to gastroenterologist’s experience, include patient body habitus, use of copper filtration, and distance of patient to the radiation source, magnification, oblique views and spot images. Familiarization of the staff with the technological evolution could probably explain the continuous reduction of KAP values, most profound during 2009 to 2012. On the other hand, the endoscopists, feeling more secure in the improved environment, undertake ERCP cases of increasing complexity (e.g. insertion of single or multiple stents, bile duct strictures beyond or under liver hilum, single or difficult bile duct stones etc.) [15,16]. This could explain the fact that KAP value is less downgrade after year 2012 (Figures 1 and 4), together with the finding of the slight increase for the number of images and the fluoroscopy time (Figures 1-3).
Comparison of these results with the literature, leads to the ascertainment that median T value of the present study is higher than those of the references 3-6 and 9, probably due to the fact that older data is included in this study. Concerning the findings of reference 2, median T value is higher, probably because their study includes data from a set of 200 randomly selected patients treated in four large hospitals. Comparison between KAP values leads to similar conclusion, i.e., this study appears to give higher radiation doses to patients than these reported in references 2-6 and 8. Higher KAP values are reported in references 7-11. Reference 17 suggested that radiation doses during ERCP may have declined in recent years partly due to better equipment and partly due to the experience gained in ERCP. Different levels of interventionalists’ experience are a main factor, as they have the ability to control additional factors such as the fluoroscopy image rate, degree of magnification, collimation, and imaging geometry, all of which can modulate the radiation dose received by patients over the same duration of T [8]. In reference 8 the investigators studied the impact of endoscopist’s experience on patient radiation exposure during ERCP and concluded that ERCPs performed by ‘low-volume’ endoscopists are associated with significantly higher radiation exposure to patients as compared with ERCPs performed by ‘high-volume’ endoscopists despite the fact that procedures performed by ‘high-volume’ endoscopists are of greater complexity.
As aforementioned, KAP value reflect multiple procedural factors not reflected by T, including the patient size and position, the geometry and setting of the fluoroscopy equipment, collimation, magnification, total number of acquisition images obtained and radiation filtration. While some factors, such as patient size, are not controllable by the endoscopist, many are modifiable. Furthermore, some factors can be modified a priori and for all procedures, like the equipment settings including pulse per second and filtration. For example changing the pulse rate on the machine can significantly decrease patient radiation doses. This is not reflected in T value. It is recommended to use pulsed fluoroscopy with the lowest possible pulse rate, rather than continuous fluoroscopy; to store, when possible, the “last image hold” as an alternative to taking a radiograph; to collimate the X-ray beam to the smallest practical size; to increase tube voltage as far as possible without compromising image quality; and to use magnification modes only if necessary and reverting back to the lowest needed magnification once the higher resolution is no longer needed. The use of time limited fluoroscopy may also be considered if this is not too impractical [15]. Mean values of KAP reported for diagnostic and therapeutic ERCP are in the range of 3–115 Gy‚??cm2 and 8–333 Gy‚??cm2 [15], respectively, with the maximum values of which to be significantly higher than those found in this study (mean KAP values ranged from 21.4 to 63.6 Gy‚??cm2). In more general sense, higher level of patient radiation protection might be a result of advances in radiological equipment, technical considerations and staff awareness as well as different operating methods and culture.
Endoscopy societies are of increasing awareness of the radiation exposure effects on both patient and staff and have published Radiation protection guidelines [15-18]. Measurement and documentation of fluoroscopy time and radiation dose during ERCP are set as quality indicators of ERCP procedures.
Few studies that evaluate radiation exposure to staff during ERCP are found in the recent literature [11,19-23]. These studies confirm that the radiation exposure to personnel undertaking ERCP is not negligible and radiation protection measures should be taken. Furthermore, gastroenterologists who are involved in ERCP procedures may work at specialised centres and may perform multiple procedures daily. Effective dose to endoscopists has been estimated to be 2–90 μSv per ERCP based on measurements using two dosimeters and as 3–70 μSv when one dosimeter was used (15). In this study, staff radiation exposure values provided by the authorities were always close to 0 μSv, although staff radiation exposure may be significantly higher with ‘over-couch’ X-ray systems (and mobile C-arm units) compared with stationary under-couch X-ray systems [15]. Close monitoring of patient and staff radiation doses by the medical physics staff (as in our hospital) can help indeed in this.
While the effects of radiation from one ERCP are unlikely to have any negative effects on patients’ health, the cumulative effects of multiple radiologic procedures including ERCPs can be detrimental. Acknowledging this need, the World Gastroenterology Organization, in a joint collaboration with the International Atomic Energy Agency and the European Society of Gastroenterology (ESGE) and the American Society for Gastrointestinal Endoscopy, has developed guidelines on minimizing radiation exposure for patients and staff in endoscopy [15,18]. In these guidelines, recording radiation exposure factors for the patient, such as fluoroscopy time (T) and kerma-area product (KAP) and measuring radiation dose for the staff are recommended for dose optimisation. This is a reason for routine radiation dose monitoring as a valuable tool for reducing both patient and staff radiation levels. The number of procedures per endoscopist, the ERCP type (diagnostic and therapeutic) and, mainly, the complexity of each clinical case will definitely affect radiation dose. With the lowering of the recommended radiation dose limit for the eye lens to 20 mSv/year, monitoring of radiation doses at the level of the eye lens will be needed, especially with over-couch systems that do not have adequate Radiation Protection shielding [15].
Conclusion
The eight years evaluation of patient and staff radiation exposure was presented. Although all 1632 ECRP procedures were performed by a single, well experienced endoscopist, using the same X-ray imaging system, additional factors, such as behavior modification during the procedure and the complexity of each clinical case definitely affect radiation dose. The number of procedures per endoscopist, the ERCP type (diagnostic and therapeutic) and, mainly, the complexity of each clinical case affect staff radiation dose too. KAP and T values of the present study appeared to be close to those reported in similar studies in the literature. Monthly endoscopist’s radiation dose was negligible due to the high level of experience and the proper use of all radiation protection equipment of the endoscopic gastroenterology department.
References
- Baron TH, Petersen BT, Mergener K, Chak A, Cohen J, et al. (2006) Quality indicators for endoscopic retrograde cholangiopancreatography. Gastrointest Endosc 63: S29-S34.
- Tsapaki V, Delinikolas P, Paraskeva KD, Paspatis IAG, Scotiniotis H, et al. (2016) Preliminary diagnostic reference levels for endoscopic retrograde cholangio-pancreatography in Greece. Phys Medica 32: 607-611.
- Tsapaki V, Paraskeva KD, Mathou N, Andrikopoulos E, Tentas P, et al. (2011) Patient and endoscopist radiation doses during ERCP procedures. Radiat Prot Dosim 147: 111-113.
- Hadjiconstanti AC, Messaris GA, Thomopoulos KC, Panayiotakis GS (2017) Patient dose during therapeutic endoscopic retrograde cholangiopancreatography procedure. Radiat Prot Dosimetr.
- Rodríguez-Perálvarez ML, Miñano-Herrrero JA, Hervás-Molina AJ, Benítez-Cantero JM, García-Sánchez V, et al. (2011) Radio induced cancer risk during ERCP. Is it a real clinical problem. Rev Esp Enferm Dig 103: 191-195.
- Saukko E, Henner A, Ahonen SM (2015) Radiation exposure to patients during endoscopic retrograde cholangiopancreatography: A multicenter study in Finland. Radiography 21: 131-135.
- Seo D, Kim KH, Kim JS, Han S, Park K, et al. (2015) Evaluation of radiation doses in patient and medical staff during endoscopic retrograde cholangiopancreatography procedures. Radiat Prot Dosim 168: 516-522.
- Liao C, Thosani N, Kothari S, Friedland S, Chen A, et al. (2015) Radiation exposure to patients during ERCP is significantly higher with low-volume endoscopists. Gastrointest Endosc 81: 391-398.
- Patient dose optimization in fluoroscopically guided interventional procedures: Final report of a coordinated research project (2010) IAEA-TECDOC-1641. International Atomic Energy Agency.
- Tsalafoutas IA, Paraskeva KD, Yakoumakis EN, Vassilaki AE, Maniatis PN, et al. (2003) Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Radiat Prot Dosim 106: 241-246.
- Buls N, Pages J, Mana F, Osteaux M (2002) Patient and staff exposure during endoscopic retrograde cholangiopancreatography. Br J Radiol 75: 435-443.
- Saukko E, Henner A, Nieminen MT, Ahonen SM (2016) The establishment of local diagnostic reference levels in endoscopic retrograde Cholangiopancreatography: A practical tool for the optimization and quality assurance management. Radiat Prot Dosim ncw018.
- Varghese JC, Liddell RP, Farrell MA, Murray FE, Osborne DH, et al. (2000) Diagnostic accuracy of magnetic resonance cholangiopancreatography and ultrasound compared with direct cholangiography in the detection of choledocholithiasis. Clin Radiol 55: 25-35.
- National Radiological Protection Board and College of Radiographers (1997) National Protocol for patient dose measurements in Diagnostic Radiology. National Radiological protection Board.
- Dumonceau JM, Garcia-Fernandez FJ, Verdun FR, Carinou E, Donadille L, et al. (2012) Radiation protection in digestive endoscopy: European Society of Digestive Endoscopy (ESGE) Guideline. Endoscopy 44: 408-424.
- Paraskeva KD, Tsapaki V, Giannakopoulos A, Mathou NI, Evgenidou E, et al. (2012) Patients radiation during interventional ERCP is related to the complexity and technical difficulty of the procedures.
- Kachaamy T, Harrison E, Pannala R, Pavlicek W, Crowell MD, et al. (2015) Measures of patient radiation exposure during endoscopic retrograde cholangiography: beyond fluoroscopy time. World J Gastrointest 21: 1900.
- World Gastroenterology Organisation (2010) Practice guideline: Radiation protection in the endoscopy suite–minimizing radiation exposure for patients and staff in endoscopy: a Joint ASGE/IAEA/WGO Guideline, November 2009. Gastrointestinal Endoscopy 72: 227-223.
- Olgar T, Bor D, Berkmen G, Yazar T (2009) Patient and staff doses for some complex Χ-ray examinations. J Radiol Prot 29: 393-407.
- Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM (1996) Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc 44: 287-292.
- Johlin FC, Pelsang RE, Greenleaf M (2002) Phantom study to determine radiation exposure to medical personnel involved in ERCP fluoroscopy and its reduction through equipment and behavior modifications. Am J Gastroenterol 97: 893-897.
- Naidu LS, Singhal S, Preece DE, Vohrah A, Loft DE (2005) Radiation exposure to personnel performing endoscopic retrograde cholangiopancreatography. Postgrad Med J 81: 660-662.
- Uradomo LT, Goldberg EM, Darwin PE (2007) Time-limited fluoroscopy to reduce radiation exposure during ERCP: a prospective randomized trial. Gastrointest Endosc 66: 84-89.
Relevant Topics
- Abdominal Radiology
- AI in Radiology
- Breast Imaging
- Cardiovascular Radiology
- Chest Radiology
- Clinical Radiology
- CT Imaging
- Diagnostic Radiology
- Emergency Radiology
- Fluoroscopy Radiology
- General Radiology
- Genitourinary Radiology
- Interventional Radiology Techniques
- Mammography
- Minimal Invasive surgery
- Musculoskeletal Radiology
- Neuroradiology
- Neuroradiology Advances
- Oral and Maxillofacial Radiology
- Radiography
- Radiology Imaging
- Surgical Radiology
- Tele Radiology
- Therapeutic Radiology
Recommended Journals
Article Tools
Article Usage
- Total views: 4891
- [From(publication date):
February-2017 - Jul 16, 2025] - Breakdown by view type
- HTML page views : 3913
- PDF downloads : 978