Research Article Open Access
Parent Physical and Mental Health Comorbidity and Adolescent Behavior
Lisa M. Gargano*, Sean Locke, Robert M. BrackbillWorld Trade Center Health Registry, Division of Epidemiology, New York City Department of Health and Mental Hygiene, New York, NY 10013
- Corresponding Author:
- Lisa M. Gargano
World Trade Center Health Registry, Division of Epidemiology
New York City Department of Health and Mental Hygiene, New York, NY 10013
E-mail: lgargano1@health.nyc.gov
Visit for more related articles at International Journal of Emergency Mental Health and Human Resilience
Abstract
The objectives of this study were to ascertain behavioral outcomes 10-11 years after 9/11 in adolescents ages 11-18 years (0-8 years old at the time of 9/11) enrolled in the World Trade Center Health Registry (Registry), and relate these outcomes to their 9/11-exposures and to parent health. Behavioral difficulties among adolescents were assessed using the adolescent-reported Strengths and Difficulties Questionnaire (SDQ). Parental post-traumatic stress disorder (PTSD) was assessed using a 9/11-specific PTSD Checklist-Civilian Version, a cut-off score of 44 or greater was considered probable PTSD. Multivariable logistic regression was used to estimate associations of 9/11-exposure and parental health with abnormal/borderline SDQ scores, adjusting for demographic variables that were significantly associated with the SDQ score in bivariate analyses. Of the 449 adolescents, 12.5% (n=56) had abnormal/borderline SDQ scores. In the multivariable model, adolescents with severe/ moderate 9/11-exposures were 2.4 times more likely to have abnormal/borderline SDQ scores compared to adolescents with mild 9/11-exposures (95% Confidence Interval (CI): 1.1-6.4). Adolescents who had a parent with 9/11-related PTSD and at least one comorbid chronic condition were 4.2 times more likely to have abnormal/borderline SDQ scores compared to adolescents with a parent who had no reported chronic health conditions. Adolescents whose parent reported 14 or more poor mental health days in the preceding 30 days were 3.4 times more likely to have abnormal/borderline SDQ scores (95% CI: 1.2-9.5) The finding that parents’ health appears to influence adolescent behavior problems 10-11 years following a disaster may have implications for healthcare practitioners and disaster response planners.
Keywords
Adolescent; World Trade Center; Behavior Problems
Abbreviations
WTC – World Trade Center, PTSD – Post-traumatic stress disorder, SDQ – Strengths and Difficulties Questionnaire, QoL – Quality of life
What Is Known?
• World Trade Center (WTC) exposure has been associated with behavior problems in adolescents 6-7 years after the event.
• WTC-related post-traumatic stress disorder (PTSD) among parents has been associated with behavior problems in their adolescents.
What This Paper Adds?
• Even 10-11 years later, adolescents with moderate/severe WTC-exposure were more likely to have behavior problems.
• Adolescents whose parent had comorbid PTSD and at least one other chronic health condition were more likely to have behavior problems than adolescents whose parents had PTSD only or chronic health condition only.
• Parents who reported 14 or more poor mental health days were more likely to have an adolescent with behavior problems.
Introduction
Mental health disorders like depression or anxiety and physical health conditions such as asthma, other respiratory diseases, diabetes, or heart disease are becoming increasingly recognized for their importance in long-term health and quality of life among those who were affected by the terrorist attacks on the World Trade Center in New York City (NYC) on September 11, 2001 (9/11) (Caramanica et al., 2014; Jordan et al., 2011; Li et al., 2011; Miller-Archie et al., 2014; Shiratori & Samuelson, 2012). In addition, there is a wide range of serious 9/11-related mental health and behavioral outcomes affecting children and adolescents who were directly exposed to the disaster (Chemtob et al., 2010; DeVoe et al., 2006; Mann et al., 2015; J. M. Stellman et al., 2008; Stuber et al., 2005). The collection of 9/11-exposures experienced by children often included one in which one or both parents suffered 9/11-related physical or mental health outcomes. This in turn may influence children’s own mental health and behavior.
Families are fundamental to children’s well-being and have a profound direct and indirect influence on the challenges they encounter and the resources available for their needs. The range of needed inputs is broad and includes material and monetary resources, time, social connections, and institutions that parents and communities may use to encourage children’s development (National Research Council and Institute of Medicine, 1995). Family influences that affect child behavior include both family demography and processes. Family demography consists of the readily measured facts of family life: composition (e.g., one versus two parents), financial status, and parental education. Family processes consist of the ways in which family influences operate to affect children’s well-being. They include parenting styles, the provision of family environments, parent mental health, and parent substance abuse (National Research Council & Medicine, 2004). Although the nature and degree of family influences on children change over time, both experimental and nonexperimental evidence indicates that the family continues to have direct influence on a child’s decision making well into adolescence (Larson, 1974; Romer, 1994).
Chronic illness in a family member can create an environment that leads to emotional distress throughout the family, particularly the children. Children may react by isolating themselves, feeling guilty and worrying about changes in parental health. Other reactions can be symptoms of depression, anxiety, as well as withdrawn behavior and physical complaints, all of which describe internalizing problem behavior (Pakenham et al., 2006). Moreover, under these circumstances children may also act out exhibiting externalizing problems through aggressive and delinquent behavior (Diareme et al., 2006). There may also be a combination of externalizing, internalizing, social, identity and thought problems (Rodrigue & Houck, 2001). Effects of parental mental health problems due to 9/11 on child behavior have been reported in a number of studies, most of which focused on younger children (Chemtob et al., 2010; DeVoe et al., 2006; Mann et al., 2015; J. M. Stellman et al., 2008; Stuber et al., 2005). In addition, most of the pediatric studies utilized data gathered in the months after 9/11 and do not represent more recent health or behavioral status. One exception was a study conducted six to seven years after 9/11, which found that behavior problems were significantly associated with 9/11-exposure, fear for one’s own safety on 9/11, and 9/11-related PTSD in the parent (Mann et al., 2015). All of the previous 9/11 research has focused on the mental health of the parent; in this study we expanded parent health to include physical health conditions and comorbidities.
Exposure to disasters is associated with reduced quality of life (QoL), (Adams & Boscarino, 2005; Slottje et al., 2007; Wen et al., 2012) a concept that broadly refers to an individual’s everyday functioning and well-being (Bayliss et al., 2012). Studies of rescue and recovery workers found that New York City Firefighters with respiratory conditions had impaired QoL (Berninger et al., 2010). Adams and Boscarino (2005) reported that WTC-exposure was associated with poorer QoL in New York City adult residents one year after the attacks (Adams & Boscarino, 2005). Similarly, another study conducted one year after 9/11 found that QoL was inversely related to mental health symptoms (Simeon et al., 2005). A study conducted 5-6 years after 9/11 found that adults with self-reported diagnosed PTSD and/or PTSD symptoms were more likely to report 14 or more poor mental health days (Brackbill et al., 2013). To date, there have been no studies examining the relationship between parent QoL and adolescent behavior among a 9/11-exposed population.
The first objective of this study was to assess the relationship between 9/11 exposures and behavioral difficulties among adolescents ages 0-8 at the time of 9/11. The second objective was to examine the potential association between parental health and adolescent behavior difficulties among adolescents whose parents are also World Trade Center Health Registry (Registry) enrollees. We hypothesize that adolescents with direct WTC exposure and/ or family exposure will be more likely to have behavior problems. We also hypothesize that adolescents whose parents have comorbid PTSD and at least one other chronic health condition will be more likely to have behavior problems than adolescents whose parent have no health conditions. Finally, we hypothesize that adolescents whose parents report poor quality of life will be more likely to have behavior problems.
Methods
World Trade Center Health Registry (Registry)
The Registry longitudinally follows a cohort of over 71,000 individuals. Eligibility for the Registry included: being a rescue and recovery worker, a resident living in lower Manhattan south of Canal Street, being a student or staff at a school south of Canal Street, a building occupant, or a passersby south of Chambers Street on 9/11; details have been presented elsewhere (Brackbill et al., 2009; Farfel et al., 2008). Briefly, children <18 years of age were recruited through their parents and active outreach to community organizations and schools. Schools south of Canal Street in Manhattan, which included child care centers, nursery schools, and public and private schools with grades kindergarten through 12th (K–12), were contacted by mail and telephone. Registry staff gave presentations about the project to teacher and parent groups. In addition, the New York City Department of Education and several private schools endorsed the Registry project to families with potentially exposed children.
For enrollees less than 18 years of age parents or guardians completed the Wave 1 (enrollment) questionnaire which gathered data on demographics, medical history, 9/11 experiences and exposures, and current health, and, except for sections on mental health, was identical for adults and children. Follow-up surveys (Wave 3) were conducted in 2011-2012. At Wave 3, parents of adolescents completed an “adult” questionnaire that provided data on their relationship to the adolescent, household composition and income, the parent’s own emotional health, and the adolescent’s 9/11-exposures and physical health. Adolescents completed a separate questionnaire about their behavior and mental and physical health, for which a separate return envelope was provided for confidentiality (S. D. Stellman et al., 2013). Parents who were also Registry enrollees completed a separate survey that is taken by adult enrollees.
Study Sample
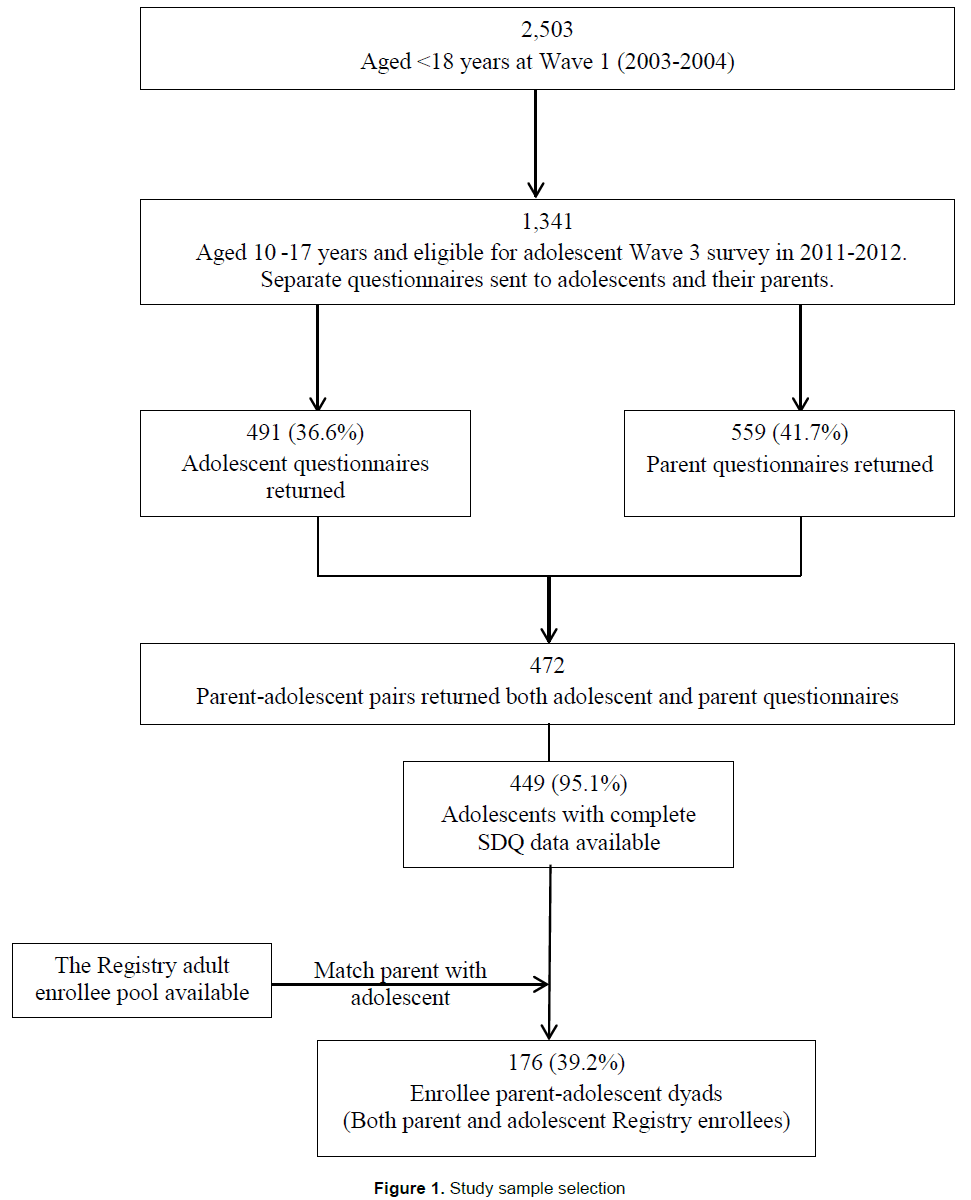
Figure 1 shows the development of the two study samples. Wave 3 collected 472 paired parent-adolescent questionnaires. Of these, 449 pairs had complete data on adolescent behavior, and were used in the first part of the analysis. For second part of the analysis we used 176 (of 449) pairs for which the parent was also a Registry enrollee and parent had complete PTSD data. These “enrollee dyads” were used to relate parental comorbidity and adolescent behavior. The Institutional Review Boards of the NYC Department of Health and Mental Hygiene and the Centers for Disease Control and Prevention approved this study.
Behavioral Assessment
Behavioral difficulties among adolescents were assessed at Wave 3 (2011-12) using the adolescent-reported Strengths and Difficulties Questionnaire (SDQ). The SDQ is a reliable screening instrument for child and adolescent behavioral problems that asks about 25 positive and negative behaviors, scored as 0, 1, and 2 for responses of “not true,” “somewhat true,” and “certainly true,” respectively (Bourdon et al., 2005; R. Goodman, 2001; R. Goodman et al., 2000; Richter et al., 2011). Higher borderline and abnormal SDQ scores have been correlated with other questionnaire and interview measures, and clinician diagnoses of child mental disorders (A. Goodman & Goodman, 2009; R. Goodman et al., 2000). The 25 SDQ items are divided into 5 domains: conduct problems, hyperactivity, emotional symptoms, peer problems, and prosocial behavior. A total difficulties score, which sums items on the 4 problem subscales (all domains except prosocial behavior) was used as the outcome of interest. In our analysis, the difficulties scores ranged from 0-40 and were categorized as normal (0–15), borderline (16–19), or abnormal (20– 40) as in previous studies of mental health assessments of children (Anmyr et al., 2012). Abnormal and borderline individual domain scores were combined into a single outcome due to small numbers.
Adolescent 9/11-Exposure
Adolescent 9/11-related exposures were assessed using information from the adolescent’s Wave 1 questionnaire as reported by a parent proxy, the Wave 3 parent questionnaire, and the Wave 3 adolescent questionnaire. Exposures included direct exposure, family WTC exposure, and a combined index. Direct exposure, reported at Wave 1, was defined as having experienced two or more of the following on 9/11: (1) witnessed one or more disturbing events during and after the WTC attacks (airplane crashing into a tower, buildings collapsing, people running away from a cloud of smoke, or people being injured, killed, falling, or jumping from one of the towers), (2) sustained an injury as a result of the attacks (burn, broken bone, concussion, cut, sprain, or other injury), (3) was caught in the dust cloud that resulted from the collapse of the WTC towers, (4) evacuated from school, and (5) thought loved one might be injured or killed on 9/11. Family exposure, reported by the parent on the Wave 3 survey, was defined as having a family member (mother, father, sibling, grandparent or any other family member) who was injured or killed in the attacks, or was in the WTC disaster and escaped unharmed. At Wave 3, adolescent reported fear for personal safety on 9/11 was also assessed in addition to direct and family exposures.
Parental Health Measures
In Wave 3, parent-enrollees were asked whether they had ever been told by a doctor that they had any of the listed health conditions. Chronic health conditions selected in this analysis have been reported to be elevated among 9/11-exposed individuals; these included heart disease (angina, heart attack, or other heart disease), diabetes, other mental health conditions (depression or anxiety), lung disease (chronic bronchitis, emphysema, reactive airway disease, sarcoidosis, or other lung diseases), and asthma (Brackbill et al., 2009; Caramanica et al., 2014; Farfel et al., 2008; Jordan et al., 2011; Li et al., 2011; Miller-Archie et al., 2014). Probable PTSD was also assessed at Wave 3 using a 9/11 specific PTSD Checklist- Civilian Version (PCL-17). As in prior published Registry analyses, enrollees with a cut-off score of 44 or greater were considered to have probable PTSD (Brackbill et al., 2009; Caramanica et al., 2014). Use of the PCL has been validated in numerous studies of civilian populations exposed to trauma including assault, motor vehicle trauma, major illnesses, and terrorism, including the 9/11 attacks (Blanchard et al., 1996; Chiu et al., 2011; McDevitt-Murphy et al., 2005; Ruggiero, Del Ben, Scotti, & Rabalais et al., 2003; Smith et al., 1999) and it has demonstrated strong psychometric properties (sensitivity=0.94–0.97, specificity=0.86–0.99) in other populations using a cutoff of 44 (Blanchard et al., 1996; Ruggiero et al., 2003). Comorbidity of chronic conditions and PTSD was defined as co-occurrence of any of these six types of self-reported diagnosed chronic conditions and probable PTSD.
Parental Quality Of Life Measures
Quality of life (QoL) for the parent enrollees was measured at Wave 3 by the number of days the parent reported poor physical or mental health out of the past 30 days. Consistent with other studies (Caramanica et al., 2014; Zahran et al., 2005), respondents were classified as having poor QoL if they reported 14 or more days in the past 30 days in which their physical or mental health was not good.
Statistical Analyses
Bivariate associations between SDQ score categories and demographic indicators were assessed using Pearson’s chi-squared test. For the first phase of analysis on the 449 adolescent-parent survey pairs, multivariable logistic regression was used to estimate associations between 9/11-exposures and SDQ score, adjusting for demographic variables that were significantly associated with SDQ score in bivariate analyses. The second phase of analysis on the 176 parent-adolescent enrollee dyads, examined the associations parental health and QoL measures and adolescent SDQ score using multivariable logistic regression models comparing individuals scoring in the abnormal or borderline range with those scoring in the normal range. All analyses were performed using SAS software version 9.4 (SAS Institute, Inc., Cary, NC), and tests were 2-sided with a significance level of P < 0.05.
Results
Demographics and SDQ Status
Demographic characteristics, household information, indication of health care need and utilization, and adolescents’ SDQ score are presented in Table 1 for phase one analysis of 449 pairs. This analysis included adolescents aged from 10-18 at Wave 3, with approximately two-thirds (62.1%) in age group 10-14 years. Boys’ and girls’ sample size are about the same (50.3% and 49.7% respectively). Over half of the sample population was non-Hispanic white (53.7%), and about two-thirds of them reported household income of more than $75,000 in 2010 (62.9%). Only 15.5 % of adolescents lived in one-parent household, and 7.8% parents reported unmet health need for the children while one-fifth (18.7%) of parents reported talking to a professional about the children’s mental or emotional problem during the preceding year. Twenty-one percent of adolescents reported having ever smoked, drank alcohol, or used marijuana. In addition, 2.9% of adolescents screened positive for PTSD.
| Total | Abnormal/Borderline (SDQ: 16-40) | Normal (SDQ: 0-15) | P-value | ||||
|---|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | No. | (%) | ||
| Total No. | 449 | -100 | 56 | -12.5 | 393 | -87.5 | |
| Age on 9/11 | |||||||
| 0-4 years | 279 | -62.1 | 33 | -11.8 | 246 | -88.2 | 0.5966 |
| 5-8 years | 170 | -37.9 | 23 | -13.5 | 147 | -86.5 | |
| Gender | |||||||
| Male | 226 | -50.3 | 31 | -13.7 | 195 | -86.3 | 0.4216 |
| Female | 223 | -49.7 | 25 | -11.2 | 198 | -88.8 | |
| Race/Ethnicity | |||||||
| Non-Hispanic White | 241 | -53.7 | 22 | -9.1 | 219 | -90.9 | 0.1371 |
| Non-Hispanic Black | 25 | -5.6 | 4 | -16 | 21 | -84 | |
| Hispanic | 48 | -10.7 | 7 | -14.6 | 41 | -85.4 | |
| Asian/Multiracial/Other | 135 | -30.1 | 23 | -17 | 112 | -83 | |
| Household gross income in 2010, $ | |||||||
| ≤75,000 | 157 | -37.1 | 29 | -18.5 | 128 | -81.5 | 0.0046 |
| >75,000 | 266 | -62.9 | 24 | -9 | 242 | -91 | |
| Parental education, Wave 3 | |||||||
| High school graduate or less | 61 | -14.5 | 8 | -13.1 | 53 | -86.9 | 0.942 |
| Some college or higher | 360 | -85.5 | 46 | -12.8 | 314 | -87.2 | |
| Household composition, Wave 3 | |||||||
| Single parent | 66 | -15.5 | 15 | -22.7 | 51 | -77.3 | 0.0126 |
| Two parent/Other | 359 | -84.5 | 41 | -11.4 | 318 | -88.6 | |
| Someone smokes at home, Wave 3 | |||||||
| No | 412 | -91.8 | 51 | -12.4 | 361 | -87.6 | 0.8414 |
| Yes | 37 | -8.2 | 5 | -13.5 | 32 | -86.5 | |
| Child’s unmet healthcare need in last 12 months | |||||||
| No | 414 | -92.2 | 43 | -10.4 | 371 | -89.6 | <0.0001 |
| Yes | 35 | -7.8 | 13 | -37.1 | 22 | -62.9 | |
| Talked to professional about child’s mental or emotional problem last 12 months | |||||||
| No | 365 | -81.3 | 33 | -9 | 332 | -91 | <0.0001 |
| Yes | 84 | -18.7 | 23 | -27.4 | 61 | -72.6 | |
| Adolescent probable PTSD | |||||||
| No | 436 | -97.1 | 46 | -10.6 | 390 | -89.4 | <0.0001 |
| Yes | 13 | -2.9 | 10 | -76.9 | 3 | -23.1 | |
| Adolescent substance use (any*) | |||||||
| No | 361 | -79 | 41 | -11.4 | 320 | -88.6 | 0.3879 |
| Yes | 96 | -21 | 14 | -14.6 | 82 | -85.4 | |
Table 1: Prevalence of Abnormal/borderline SDQ by demographic characteristics of adolescents aged 10-18 years by self-reported Strengths and Difficulties Questionnaire (SDQ) Total Score at Wave 3, WTCHR
Among 449 adolescents in the study, 393 (87.5%) had normal SDQ scores and 56 (12.5%) had abnormal/borderline SDQ scores. Two sociodemographic characteristics were significantly associated with SDQ score: lower household income at 2010 (≤$75,000 per year, P-value=.0046) and living in a single-parent household (P=.0126). Parent report of the child having unmet health care need in last 12 months (P<.0001) and having talked to a professional about child’s mental or emotional problem in last 12 months (P<.0001) was associated with SDQ score. In addition, SDQ score was associated with adolescents with probable PTSD (P < 0.001).
Adolescent SDQ and 9/11-Exposure
Almost 81% of adolescents had severe/moderate WTC exposure (Table 2). Among the 449 adolescents, 34.7% had a family exposure with 1.3% having a family member who died in the attacks. Fourteen percent of adolescents thought that their parent(s) might be hurt or killed in the attacks. For adolescents with mild WTC exposure, 5.8% had abnormal/borderline SDQ scores, compared to 14.0% of adolescents with severe/moderate exposure. Among those adolescents with a family exposure, 16.0% had abnormal/borderline SDQ while 10.6% had abnormal/borderline SDQ scores among those without a family exposure. Among adolescents who reported fearing that their parent(s) might be hurt or killed in the attacks, 20.6% had abnormal/borderline SDQ scores, compared to 11.1% of adolescents who did not report fearing for their parents’ safety (Table 2).
| Model # | WTC exposure | Total | Abnormal/Borderline (SDQ: 16-40) | Normal (SDQ: 0-15) | Adjusted OR (95% CI)a | |||
|---|---|---|---|---|---|---|---|---|
| No. | (%) | No. | (%) | No. | (%) | |||
| 1 | WTC exposure index | |||||||
| Mild | 86 | -19 | 5 | -5.8 | 81 | -94.2 | REF | |
| Severe/moderate | 363 | -81 | 51 | -14 | 312 | -86 | 2.4 (1.1-6.4) | |
| 2 | Direct WTC exposure | |||||||
| 0-1 exposure | 245 | -55 | 30 | -12.2 | 215 | -87.8 | REF | |
| 2-5 | 204 | -45 | 26 | -12.7 | 178 | -87.3 | 1.0 (0.5-1.8) | |
| 3 | Any family exposed to WTC attacks (family exposures) a | |||||||
| No | 293 | -65 | 31 | -10.6 | 262 | -89.4 | REF | |
| Yes | 156 | -35 | 25 | -16 | 131 | -84 | 2.0 (1.1-3.7) | |
| 4 | Any family member die in the WTC disaster b | |||||||
| No | 443 | -99 | 54 | -12.2 | 389 | -87.8 | REF | |
| Yes | 6 | -1 | 2 | -33.3 | 4 | -66.7 | 3.5 (0.6-22.4) | |
| 5 | Any family member injured or hurt in the WTC disaster b | |||||||
| No | 439 | -98 | 52 | -11.9 | 387 | -88.1 | REF | |
| Yes | 10 | -2 | 4 | -40 | 6 | -60 | 3.7 (0.8-17.6) | |
| 6 | Thought self might be hurt or killed in WTC disaster | |||||||
| No | 394 | -88 | 47 | -11.9 | 347 | -88.1 | REF | |
| Yes | 55 | -12 | 9 | -16.4 | 46 | -83.6 | 1.5 (0.7-3.3) | |
| 7 | Though parents might be hurt or killed in WTC disaster | |||||||
| No | 386 | -86 | 43 | -11.1 | 343 | -88.9 | REF | |
| Yes | 63 | -14 | 13 | -20.6 | 50 | -79.4 | 2.3 (1.1-4.8) | |
a Each model contains only the indicated WTC exposure variable along with the adjustment variables: household income and household composition.
b One of family exposure components.
Table 2: WTC disaster related exposures and their associations with adolescent total SDQ score
The adjusted odds ratio (AOR) for the association between more severe 9/11-exposure index and abnormal/borderline SDQ score was 2.4 compared with those with milder exposure (95% Confidence interval (CI): 1.1-6.4) (Table 2). After 10 years, direct 9/11-exposure was not associated with SDQ, but having any family exposure to the 9/11-attacks was associated with abnormal/borderline SDQ score compared to those adolescents who did not have a family exposure (AOR:2.0; 95% CI: 1.1-3.7). Also, adolescents who reported fearing for their parent(s) safety on 9/11 were 2.3 times more likely to have an abnormal/borderline SDQ score compared to those adolescents who did not fear for the safety of their parent(s) (95% CI: 1.1-4.8) (Table 2).
Adolescent SDQ In Relation To Parent Health
In part II of the analysis, using the 176 parent-adolescent enrollee dyads, we examined parental factors that influenced SDQ among adolescents. Adolescent SDQ was not associated with a parent who had either PTSD-only or at least one chronic condition (Table 3). However, having a parent with both PTSD and at least one chronic condition had a significant four-fold odds of having abnormal/ borderline SDQ score compared to those adolescents whose parent had no health conditions (AOR=4.2; 95% CI:1.4-13.2). Moreover, in a more general measure of parental health status, parents who reported 14 or more days of poor mental health in the past 30 days were three times more likely to have adolescents with abnormal/ borderline SDQ scores, as compared to those whose parent reported 13 or fewer days (AOR=3.4; 95% CI: 1.2-9.5). There was no significant association between parents reporting 14 or more days of poor physical health a month and adolescent’s SDQ score (Table 3).
| Parent | Adolescent total SDQ score | ||
|---|---|---|---|
| Abnormal/Borderline (16-40) | Normal (0-15) | Adjusted OR (95% CI)+ | |
| No. (%) | No. (%) | ||
| Comorbidity* | |||
| Neither | 8 (8.9) | 82 (91.1) | REF |
| PTSD only or at least one chronic condition only | 4 (6.5) | 58 (93.5) | 0.7 (0.2-2.5) |
| PTSD+ at least one chronic condition | 7 (29.2) | 17 (70.8) | 4.2 (1.4-13.2) |
| Quality of Life | |||
| Poor Physical Health Days | |||
| ≤13 days | 16 (10.4) | 138 (89.6) | REF |
| ≥14 days | 3 (13.6) | 19 (86.4) | 1.4 (0.4-5.1) |
| Poor Mental Health Days | |||
| ≤13 days | 12 (8.3) | 133 (91.7) | REF |
| ≥14 days | 7 (23.3) | 23 (76.7) | 3.4 (1.2-9.5) |
Chronic conditions include heart disease (angina, heart attack, hypertension, coronary hear t disease); diabetes; lung disease (chronic bronchitis, emphysema, COPD, RADS, sarcoidosis, pulmonary fibrosis); autoimmune disease (rheumatoid arthritis, other autoimmune disease); GERD; mental health disorder (depression, anxiety); asthma; + adjusted for household income and household composition.
Table 3: Adjusted odds ratios (AOR) for association of parental comorbidity with adolescent SDQ among 176 enrollee parent-adolescent dyads
Limitations
Among the limitations is that the 449 adolescents represent a response rate of 37%. Enrollment in the Registry is voluntary therefore findings may not be generalizable to all 9/11-exposed youth. Adolescents who did not complete Wave 3 were similar to those who did with regard to age at 9/11, sex, parent education, and all WTC exposures. However, using chi-square tests there was a significantly greater proportion of white than black or Hispanic adolescents among those completing the Wave 3 survey (p<0.0001) as well as a greater proportion of those whose parents reported a 2002 income of more than $50,000 (p=0.01). SDQ assessment was not done at baseline, so that change in degree of behavioral difficulties could not be evaluated. In addition, we did not collect information on other factors known to be associated with behavior problems in adolescents, such as parenting style, parent substance use, or peer influence.
Discussion
Ten to eleven years after the World Trade Center attacks, 12.5% of adolescents with direct and substantial exposures to the attacks when they were 0-8 years old had behavioral difficulties. Based on parental reporting, this figure is higher than US population rates among adolescents’ ages 11–17 years (9.2%) (Bourdon et al., 2005). Although our data on behavioral difficulties were obtained from adolescents themselves, there is reasonable agreement among parent-, teacher-, and adolescent-derived SDQ scores in UK adolescents (Calam et al., 2005).
We also observed strong associations between poor parental health and adolescent behavior problems. Similar to findings from the general population (Diareme et al., 2006; Pakenham et al., 2006; Rodrigue & Houck, 2001), we found that the adolescents of parents with comorbid health conditions were more likely to have behavioral difficulties, compared to adolescents whose parents did not have any adverse health condition. Previous work on the effects of parental stress from 9/11 on child behavior has mostly been conducted in very young children (Chemtob et al., 2010; DeVoe et al., 2006), and only a few studies have looked at adolescent behavior. A study by Stuber and colleagues conducted 4 months after 9/11, found that parents with PTSD or depression were significantly more likely to have a child with behavior problems (Stuber et al., 2005). Another study of World Trade Center rescue and recovery workers found that those with PTSD were more likely to report psychological symptoms and behavioral problems in their children compared to those workers without PTSD (J. M. Stellman et al., 2008). A previous Registry study found that adolescent behavior and mental health problems were associated with parental 9/11-exposure and related PTSD (Mann et al., 2015).
Many families experienced common exposures on 9/11 including evacuation of home or school, destruction or damage to their home, loss of parental employment, and abrupt changes in the child’s social network (Comer et al., 2010). Fourteen percent of the adolescents in this study reported having perceived a threat to, or feared for the life or safety of parents/loved one on 9/11, and 34.7% reported having a family member injured or killed as a result of the WTC attack or present at the attacks but escaped. Consequently, a child’s individual exposures were in addition to a family environment in which one or both parents may have suffered from 9/11-related health outcomes such as asthma, PTSD, or depression. Family exposure and fear for parent/loved one’s life or safety was independently associated with behavioral difficulties. However, since these adolescents were very young on 9/11, their perceptions of parent/loved one’s perceived safety on 9/11 may have been biased by the impact of the event on their lives during the 10-11 years prior to being surveyed. Associations between parental PTSD and behavioral problems in adolescents may also be a result of their witnessing and emulating their parents’ behaviors. Another pathway for the influence of parental PTSD on adolescent behavior may be a feedback loop by which distress in one triggers distress in the other (Hoven et al., 2009).
Overall health depends on both physical and mental well-being. Measuring the number of days when parents report that their mental or physical health was not good represents an important facet of health-related QoL (Zahran et al., 2005). QoL measures have not been well studied in their relationship with adolescent behavior. We found that the number of poor mental health days reported by parents, but not physical health days, was associated with adolescent behavior problems. Continued research is needed on this relationship as QoL is more of a measure of functioning, beyond just mental or physcial illness.
Similar to previous studies (Mann et al., 2015; Schwartz et al., 1994), we found that behavioral problems were more often observed in adolescents who lived in lower income and/or singleparent homes. Unlike previous studies, we did not find an association between behavioral problems and race/ethnicity (Mann et al., 2015).
We also found that 13 (2.9%) of the 449 adolescents had probable PTSD. There is limited normative prevalence data for PTSD among adolescents in New York City prior to 9/11, one report of performance testing of the DISC Version 2.3 in the early 1990s in 4 cities including New York City found a prevalence of 1.6% for any anxiety disorder using DSM-III-R Criteria with diagnosis-specific impairment criteria (Shaffer et al., 1996).
One limitation to previous 9/11 work is that most studies have focused on measuring solely one condition in the parent, usually PTSD. In this study we found that parents with PTSD co-morbid with one or more other chronic condition were at increased risk of having an adolescent with behavior problems. This did not hold true if the parent had PTSD only or at least one chronic condition only. The only other 9/11 study that assessed multiple health outcomes in parents looked only at multiple mental health conditions and found that preschool children of mothers with two mental health disorders were at a greater risk for behavioral problems compared to children of mothers with only one disorder (Nomura & Chemtob, 2009). Healthcare practitioners should be aware of the relationship between parent health and adolescent behavior and refer children with problem behavior to health professionals provding interventions. It is recommended that medical doctors receive education about how illness can impact families and how to treat behaviors and emotional problems of family members (Gorter et al., 2010).
A number of theories that may help to explain the association between parental exposure to traumatic events and their children’s reactions have been proposed. These include the child’s biological predisposition, impaired parenting connected to mental health problems, child’s modeling from parents’ actions, and mutually experienced social milieu, such as SES and inadequate social support, or other environmental exposure or factors (Schwartz et al., 1994). It is also known that parents with a psychiatric disorder are more likely to exhibit maladaptive behavior, which is associated with psychiatric symptoms in their children (Johnson et al., 2001). According to the stress and coping theory, the threat of worsening parental health is considered a continuous stressor exceeding children’s coping resources and increasing the probability of problem behavior (Forehand et al., 1998; Pakenham et al., 2006; Pedersen & Revenson, 2005). Parental disease can be perceived as stressful by a child depending on factors directly relating to the child and factors associated with the situation (Lazarus, 1974). Longitudinal studies are needed to determine if the association between adolescent behavior problems and parent health develops into social or physical health problems later in life.
Conclusions
The associations between parent comorbid health conditions and child behavior problems highlight the need for family-based prevention and treatment in disaster planning and response, especially when family members collectively experience a traumatic event. The present findings are important in demonstrating that exposure to terrorism can be correlated with a diverse range of child psychosocial problems. Elevated rates of post-traumatic stress have been the most frequently reported outcome among terrorism exposed populations, (Comer et al., 2010; Furr et al., 2010) but this may be in part because PTSD is most commonly assessed (La Greca, 2007). Comprehensive surveys assessing a range of emotional and behavioral problems after terrorism, in the short- and long-term, are needed to best inform clinical practices for affected youth.
Acknowledgements
This publication was supported by Cooperative Agreement Number 5U50/OH009739 and 5U50/OH009739 from the National Institute for Occupational Safety and Health (NIOSH) of the Centers for Disease Control and Prevention (CDC); U50/ATU272750 from the Agency for Toxic Substances and Disease Registry (ATSDR), CDC, which included support from the National Center for Environmental Health, CDC; and by the New York City Department of Health and Mental Hygiene (NYC DOHMH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH-CDC or the Department of Health and Human Services.
References
- Adams, R. E., &Boscarino, J. A. (2005). Stress and Well-Being in the Aftermath of the World Trade Center Attack: the Continuing Effects of a Communitywide Disaster. Journal of Community Psychology, 33(2), 175-190
- Anmyr, L., Larsson, K., Olsson, M., &Freijd, A. (2012). Strengths and difficulties in children with cochlear implants–comparing self-reports with reports from parents and teachers. International Journal of Pediatric Otorhinolaryngology, 76(8), 1107-1112
- Bayliss, M., Rendas-Baum, R., White, M. K., Maruish, M., Bjorner, J., & Tunis, S. L. (2012). Health-related quality of life (HRQL) for individuals with self-reported Chronic Physical And/Or Mental Health Conditions: Panel Survey Of An Adult Sample In The United States. Health and Quality of life outcomes, 10(1), 154
- Berninger, A., Webber, M. P., Weakley, J., Gustave, J., Zeig-Owens, R., Lee, R., et al. (2010).Quality of life in relation to upper and lower respiratory conditions among retired 9/11-exposed firefighters with pulmonary disability.Quality of Life Research, 19(10), 1467-1476
- Blanchard, E. B., Jones-Alexander, J., Buckley, T. C., &Forneris, C. A. (1996).Psychometric properties of the PTSD Checklist (PCL).Behaviour Research and Therapy, 34(8), 669-673
- Bourdon, K. H., Goodman, R., Rae, D. S., Simpson, G., &Koretz, D. S. (2005). The Strengths and Difficulties Questionnaire: US normative data and psychometric properties. Journal of the American Academy of Child & Adolescent Psychiatry, 44(6), 557-564
- Brackbill, R. M., Hadler, J. L., DiGrande, L., Ekenga, C. C., Farfel, M. R., Friedman, S., et al. (2009).Asthma and posttraumatic stress symptoms 5 to 6 years following exposure to the World Trade Center terrorist attack.JAMA, 302(5), 502-516
- Brackbill, R. M., Stellman, S. D., Perlman, S. E., Walker, D. J., & Farfel, M. R. (2013). Mental health of those directly exposed to the World Trade Center disaster: unmet mental health care need, mental health treatment service use, and quality of life. Social Science & Medicine, 81, 110-114
- Calam, R., Gregg, L., & Goodman, R. (2005). Psychological adjustment and asthma in children and adolescents: the UK Nationwide Mental Health Survey. Psychosomatic Medicine, 67(1), 105-110
- Caramanica, K., Brackbill, R. M., Liao, T., &Stellman, S. D. (2014).Comorbidity of 9/11Related PTSD and Depression in the World Trade Center Health Registry 10–11 Years Postdisaster.Journal of Traumatic Stress, 27(6), 680-688
- Chemtob, C. M., Nomura, Y., Rajendran, K., Yehuda, R., Schwartz, D., &Abramovitz, R. (2010).Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children’s behavior.Child Development, 81(4), 1129-1141
- Chiu, S., Webber, M. P., Zeig-Owens, R., Gustave, J., Lee, R., Kelly, K. J., et al. (2011). Performance characteristics of the PTSD Checklist in retired firefighters exposed to the World Trade Center disaster. Annals of Clinical Psychiatry, 23(2), 95-104
- Comer, J. S., Fan, B., Duarte, C. S., Wu, P., Musa, G. J., Mandell, D. J., et al. (2010). Attack-related life disruption and child psychopathology in New York City public schoolchildren 6-months post-9/11.Journal of Clinical Child & Adolescent Psychology, 39(4), 460-469
- DeVoe, E. R., Bannon, W. M., & Klein, T. P. (2006).Post9/11 Helpseeking by New York City Parents on Behalf of Highly Exposed Young Children.American Journal of Orthopsychiatry, 76(2), 167-175
- Diareme, S., Tsiantis, J., Kolaitis, G., Ferentinos, S., Tsalamanios, E., Paliokosta, E., et al. (2006).Emotional and behavioural difficulties in children of parents with multiple sclerosis.European Child & Adolescent Psychiatry, 15(6), 309-318
- Farfel, M., DiGrande, L., Brackbill, R., Prann, A., Cone, J., Friedman, S., et al. (2008).An overview of 9/11 experiences and respiratory and mental health conditions among World Trade Center Health Registry enrollees.Journal of Urban Health, 85(6), 880-909
- Forehand, R., Biggar, H., &Kotchick, B. A. (1998). Cumulative risk across family stressors: Short-and long-term effects for adolescents. Journal of Abnormal Child Psychology, 26(2), 119-128
- Furr, J. M., Comer, J. S., Edmunds, J. M., & Kendall, P. C. (2010). Disasters and youth: a meta-analytic examination of posttraumatic stress. Journal of Consulting and Clinical Psychology, 78(6), 765-780
- Goodman, A., & Goodman, R. (2009).Strengths and difficulties questionnaire as a dimensional measure of child mental health.Journal of the American Academy of Child & Adolescent Psychiatry, 48(4), 400-403
- Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire.Journal of the American Academy of Child & Adolescent Psychiatry, 40(11), 1337-1345
- Goodman, R., Ford, T., Simmons, H., Gatward, R., & Meltzer, H. (2000).Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample.The British Journal of Psychiatry, 177(6), 534-539
- Gorter, J. W., VisserMeily, A., &Ketelaar, M. (2010).The relevance of familycentred medicine and the implications for doctor Education.Medical Education, 44(4), 332-334
- Hoven, C. W., Duarte, C. S., Wu, P., Doan, T., Singh, N., Mandell, D. J., et al. (2009). Parental exposure to mass violence and child mental health: The first responder and WTC evacuee study. Clinical Child and Family Psychology Review, 12(2), 95-112
- Johnson, J. G., Cohen, P., Kasen, S., Smailes, E., & Brook, J. S. (2001).Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring.Archives of General Psychiatry, 58(5), 453-460
- Jordan, H. T., Miller-Archie, S. A., Cone, J. E., Morabia, A., &Stellman, S. D. (2011). Heart disease among adults exposed to the September 11, 2001 World Trade Center disaster: results from the World Trade Center Health Registry. Preventive Medicine, 53(6), 370-376
- La Greca, A. M. (2007). Understanding the psychological impact of terrorism on youth: Moving beyond posttraumatic stress disorder. Clinical Psychology: Science and Practice, 14(3), 219-223
- Larson, L. E. (1974). An examination of the salience hierarchy during adolescence: The influence of the family. Adolescence, 9(35), 317
- Lazarus, R. S. (1974). Psychological stress and coping in adaptation and illness. The International Journal of Psychiatry in Medicine, 5(4), 321-333
- Li, J., Brackbill, R. M., Stellman, S. D., Farfel, M. R., Miller-Archie, S. A., Friedman, S., et al. (2011). Gastroesophageal reflux symptoms and comorbid asthma and posttraumatic stress disorder following the 9/11 terrorist attacks on World Trade Center in New York City. The American Journal of Gastroenterology, 106(11), 1933-1941
- Mann, M., Li, J., Farfel, M. R., Maslow, C. B., Osahan, S., &Stellman, S. D. (2014).Adolescent behavior and PTSD 6–7 years after the World Trade Center terrorist attacks of September 11, 2001.Disaster Health, 2(3-4), 121-129.`
- McDevittMurphy, M. E., Weathers, F. W., & Adkins, J. W. (2005).The use of the Trauma Symptom Inventory in the assessment of PTSD symptoms.Journal of Traumatic Stress, 18(1), 63-67
- Miller-Archie, S. A., Jordan, H. T., Ruff, R. R., Chamany, S., Cone, J. E., Brackbill, R. M., et al. (2014).Posttraumatic stress disorder and new-onset diabetes among adult survivors of the World Trade Center disaster.Preventive Medicine, 66, 34-38
- National Research Council. (2004). Children's health, the nation's wealth: assessing and improving child health. National Academies Press
- Brooks-Gunn, J., Brown, B., Duncan, G. J., & Moore, K. A. (1995, October). Child development in the context of family and community resources: An agenda for national data collections. In Integrating federal statistics on children: Report of a workshop. Commission on Behavioral and Social Sciences and Education.The National Academy of Sciences, pp. 27-97
- Nomura, Y., &Chemtob, C. M. (2009). Effect of maternal psychopathology on behavioral problems in preschool children exposed to terrorism: use of generalized estimating equations to integrate multiple informant reports. Archives of Pediatrics& Adolescent Medicine, 163(6), 531-539
- Pakenham, K. I., Bursnall, S., Chiu, J., Cannon, T., &Okochi, M. (2006). The psychosocial impact of caregiving on young people who have a parent with an illness or disability: Comparisons between young caregivers and noncaregivers. Rehabilitation Psychology, 51(2), 113
- Pedersen, S., &Revenson, T. A. (2005). Parental illness, family functioning, and adolescent well-being: a family ecology framework to guide research. Journal of Family Psychology, 19(3), 404
- Richter, J., Sagatun, Å., Heyerdahl, S., Oppedal, B., &Røysamb, E. (2011). The strengths and difficulties questionnaire (SDQ)–SelfReport.An analysis of its structure in a multiethnic urban adolescent sample.Journal of Child Psychology and Psychiatry, 52(9), 1002-1011
- Rodrigue, J. R., & Houck, C. D. (2001).Parental health and adolescent behavioral adjustment.Children's Health Care, 30(2), 79-91
- Romer, D. (1994). Using mass media to reduce adolescent involvement in drug trafficking. Pediatrics, 93(6), 1073-1077
- Ruggiero, K. J., Ben, K. D., Scotti, J. R., &Rabalais, A. E. (2003). Psychometric properties of the PTSD Checklist—Civilian version.Journal of Traumatic Stress, 16(5), 495-502
- Schwartz, S., Dohrenwend, B. P., &Levav, I. (1994).Nongenetic familial transmission of psychiatric disorders?Evidence from children of Holocaust survivors.Journal of Health and Social Behavior, 385-402
- Shaffer, D., Fisher, P., Dulcan, M. K., Davies, M., Piacentini, J., Schwab-Stone, M. E., ...&Canino, G. (1996). The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, acceptability, prevalence rates, and performance in the MECA study. Journal of the American Academy of Child & Adolescent Psychiatry, 35(7), 865-877
- Shiratori, Y., & Samuelson, K. W. (2012). Relationship between posttraumatic stress disorder and asthma among New York area residents exposed to the World Trade Center disaster. Journal of Psychosomatic Research, 73(2), 122-125
- Simeon, D., Greenberg, J., Nelson, D., Schmeidler, J., & Hollander, E. (2005). Dissociation and posttraumatic stress 1 year after the World Trade Center disaster: follow-up of a longitudinal survey. The Journal of Clinical Psychiatry, 66(2), 231-237
- Slottje, P. L., Twisk, J. W., Smidt, N., Huizink, A. C., Witteveen, A. B., Van Mechelen, W., et al. (2007). Health-related quality of life of firefighters and police officers 8.5 years after the air disaster in Amsterdam.Quality of Life Research, 16(2), 239-252
- Smith, M. Y., Redd, W., DuHamel, K., Vickberg, S. J., & Ricketts, P. (1999). Validation of the PTSD checklist–civilian version in survivors of bone marrow transplantation.Journal of Traumatic Stress, 12(3), 485-499
- Stellman, J. M., Smith, R. P., Katz, C. L., Sharma, V., Charney, D. S., Herbert, R., et al. (2008). Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environmental Health Perspectives, 116(9), 1248
- Stellman, S. D., Thomas, P. A., S. Osahan, S., Brackbill, R. M., & Farfel, M. R. (2013). Respiratory health of 985 children exposed to the World Trade Center disaster: report on World Trade Center Health Registry wave 2 follow-up, 2007–2008. Journal of Asthma, 50(4), 354-363
- Stuber, J., Galea, S., Pfefferbaum, B., Vandivere, S., Moore, K., &Fairbrother, G. (2005). Behavior problems in New York City's children after the September 11, 2001, terrorist attacks.American Journal of Orthopsychiatry, 75(2), 190
- Wen, J., Shi, Y. K., Li, Y. P., Yuan, P., & Wang, F. (2012). Quality of life, physical diseases, and psychological impairment among survivors 3 years after Wenchuan earthquake: a population based survey. PloSOne, 7(8), e43081
- Zahran, H. S., Kobau, R., Moriarty, D. G., Zack, M. M., Holt, J., Donehoo, R., &Centers for Disease Control and Prevention (CDC). (2005). Health-related quality of life surveillance—United States, 1993–2002.MMWR SurveillSumm, 54(4), 1-35.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 4654
- [From(publication date):
June-2017 - Apr 04, 2025] - Breakdown by view type
- HTML page views : 3782
- PDF downloads : 872