Paratesticular Plexiform Schwannoma: A Case Report
Received: 03-Jul-2020 / Accepted Date: 25-Jul-2020 / Published Date: 31-Jul-2020 DOI: 10.4172/2167-7964.1000327
Abstract
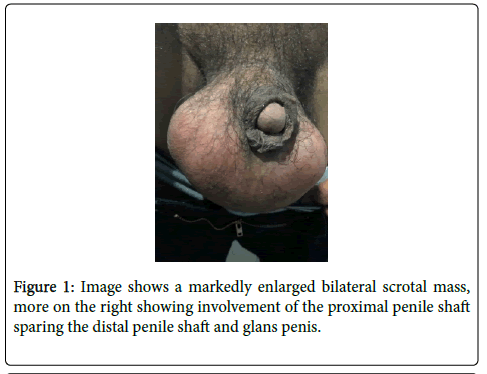
Schwannomas of the paratesticular region are rare. Various types of schwannomas have been reported. However, the plexiform type of schwannoma (PS) is extremely rare comprising of 4.3% of schwanommas. Although this type of schwannoma is benign and does not possess malignant potential, it is important to diagnose such for the management of the patient. This is a case of a 55-year old male presenting with a 20-year indolent course of an enlarging scrotal mass with no other associated symptoms until 2 years prior to admission where the patient complained of intermittent pain in the scrotal region. Ultrasound and plain abdominal CT scan showed complex scrotal mass with normal testes and epididymis. Initial impression was a fibrous pseudotumor, rule out paratesticular sarcoma. Patient underwent right radical orchiectomy. The histologic features were suggestive of paratesticular plexiform neurilemoma (plexiform schwannoma) with no abnormality in the testis.
Keywords: Schwannoma; Paratesticular sarcoma
Introduction
Schwannomas are benign, encapsulated neurogenic tumors have diverse histological subtypes. The plexiform schwannoma type represent 4.3% of schwannomas and are commonly encountered in the head and neck region and are extremely rare in the penis. A study published by Gkekas C, Kalyvas V et. al published last April 2019 reviewed published literature identifying only 34 cases of penile schwannomas, and 3 cases were characterized as plexiform schwannoma variant isolated in the penis [1].
Plexiform schwannomas mostly affect younger adults, with no pronounced sex predilection. Most are solitary, sporadically occurring tumors [2]. Schwannoma arises frequently from the acoustic nerve. In the peripheral nervous system, it is usually found in the main nerves of the limbs (elbow, wrist, and knee) [3]. Although schwannoma is the most common peripheral nerve sheath tumor, it is extremely rare in the paratesticular area. To date, intrascrotal schwannomas have been reported in only seven cases in the medical literature written in English [4]. No published literature can be found involving the paratesticular region plexiform schwannoma type.
This is a complete case report including clinical, diagnostic imaging, intra-operative and histopathological findings of a paratesticular schwannoma (plexiform type).
Case Presentation
Chief complaint
DC is a 55-year-old, male, married, Roman Catholic from Taytay, Palawan came in due to a enlarging scrotal mass of ~20 years duration. History of present illness
~20 years prior to admission, the patient noticed bilateral enlargement of the scrotal region with no associated symptoms. Patient did not consult any physician since it did not alter his daily activities as well as his sexual activity.
~9 years prior to admission, patient noticed further bilateral enlargement of the scrotal region with no associated symptoms.
~2 years prior to admission, the patient’s scrotal mass was still enlarging, now with associated tenderness in the scrotal area, intermittent and pulsating in character. There was also note of unintentional weight loss. However, still no consult done.
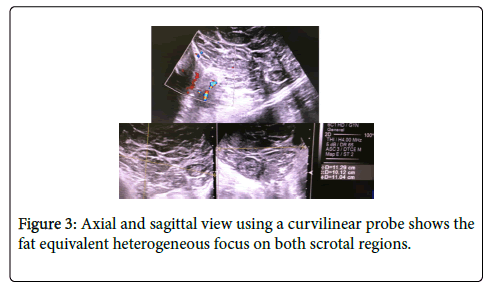
~1 month prior to admission, patient underwent scrotal ultrasound. Scrotal ultrasound showed a fat equivalent heterogeneous focus on both scrotal regions, consider neoplastic process. Testes and epididymis are normal. Normal sized bilateral inguinal lymph nodes.
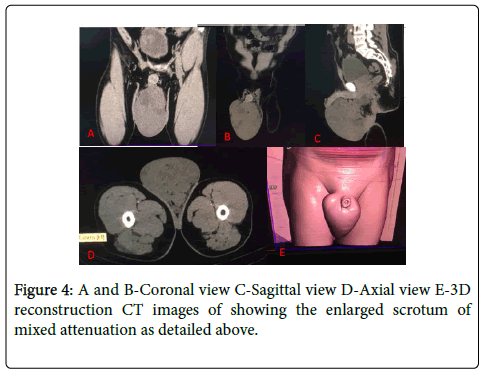
Subsequent plain abdominal CT scan was then done showing a complex scrotal mass measuring 11.3 x 11.0 x 10.3-cm compressing and pushing both testes laterally.
Eleven days prior to admission, due to diagnostic findings patient sought consult at OLLH-ER where patient was advised and scheduled for bilateral orchiectomy. Hence, admission.
Past health history
Patient was diagnosed with hypertension last 2004 taking losartan +amlodipine (Amlife) 50/5 mg twice a day (compliant). He was diagnosed with PTB (2006) and completed treatment for 6 months. Patient denies history of asthma, COPD, cancer, skin disease, diabetes, and allergy.
Family history
Unremarkable, No history of neurofibromatosis.
Personal and social history
Patient had 1 pack year smoking history last 2014 and is an occasional alcoholic beverage drinker.
Patient has a 29-year old daughter.
Physical examination
General: awake, alert, coherent, not in respiratory distress
Vital signs: BP: 140/100, HR: 60, RR 20, Temp: 37°c
HEENT: Anicteric sclerae, pink palpebral conjunctivae, (-) cervical lymphadenopathies
Chest and lungs: decreased breath sounds, right base
Caridovascular: normal rate, regular rhythm, no murmurs
Gastrointestinal: soft non-tender, normoactive bowel sound
Extremities: warm to touch, no edema nor clubbing; no café-au-lait spots, no freckles, no gross malformations
Neurologic: No neurological deficit; no paresthesia nor numbness
Figure 2: A-As detailed above, axial and sagittal views using linear probe shows both testicles are normal in size and echopattern Both show homogeneous echopattern with no focal mass nor calcifications B-Fat equivalent heterogeneous focus is seen on both scrotal regions, with no evidence of peristalsis and associated vascularity on Color Doppler study, causing superolateral displacement of both testes Lymphdenopathy was not detected.
Diagnostic examination
Ultrasound was done for further evaluation of the scrotal mass showing a normal testes and epididymis with normal intratesticular flow. Fat equivalent heterogeneous focus is seen on both scrotal regions, with no evidence of peristaslsis, and associated vascularity on Color Doppler study, causing superolateral displacement of both testes. No evident hydrocele seen in both scrotal sacs with an impression of a neoplastic process.
A plain abdominal CT scan was also done showing a defined, mixed attenuation mass in the scrotum measuring 11.3 x 11.0 x 10.3 cm extending from the left levator ani muscle. The said mass is compressing and pushing both testes laterally.
Therapeutic approach
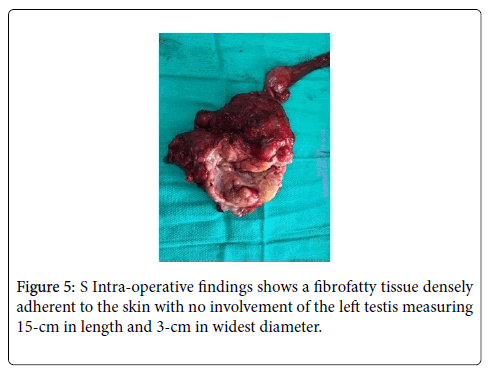
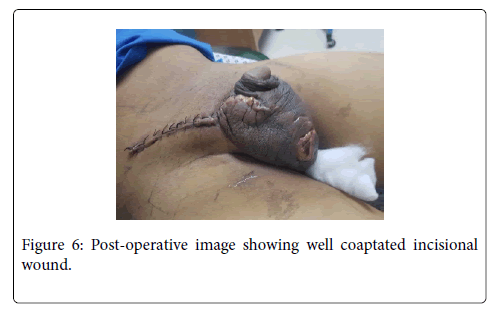
Patient was scheduled for an elective operation with an initial diagnosis of a fibrous pseudotumor, rule out paratesticular tumor in the right. Patient underwent right radical orchiectomy under spinal anesthesia.
Post-operative state
Patient tolerated procedure with no complications. Regular change of dressing was done. Pain medications were prescribed. After 6 months, patient reports no evidence of recurrence nor erectile dysfunction.
Gross and microsopic findings
Gross report: Right testis, epididymis and spermatic cord appeared grossly unremarkable. Paratesticular mass consists of a large, ovoid mass weighing 800 g measuring 15.1 x 14 x 8.4 cm. The outer surface is tan, smooth, and rubbery, but a few of nodules appear gray-tan, soft with myxoid, glistening cut surfaces. No hemorrhagic or necrotic areas.
HIstopathologic findings: Mass composing of spindle shaped, small plexiform palisading nodules exhibiting hypercellularity (Antoni A) and loose scarce cellular area (Antoni B) with a diagnosis of plexiform neurilemoma (plexiform schwannoma), paratesticular mass. No significant abnormality seen in the testis.
Immunohistochemistry for S-100 done on formalin-fixed, paraffinembedded tissue section showed diffuse, strong nuclear and cytoplasmic staining of tumor cells which confirm the neural (Schwann cell) origin of tumor cells.
Discussion
Plexiform schwannoma (PS) are usually superficial, occurring typically in the dermis and subcutaneous tissue [1]. A schwannoma is usually benign nerve sheath tumors composed of Schwann cells, which normal produce the insulating myelin sheath covering the peripheral nerves. Rate of pelvic schwannoma is 1% and are found in all age groups affecting both sexes equally. Malignant schwannomas are large, infiltrating, and fast-growing tumors [3]. Clinically schwannomas tend to be asymptomatic, however when they enlarge, they result in symptoms related to compression of the surrounding structures [5]. Malignant peripheral nerve sheath tumors (MPNST) have been described in the penis but are not associated with schwannoma. However, plexiform neurofibroma can progress to MPNST and therefore identifying plexiform schwannoma is essential due to their different biologic behavior [1].
Pre-operative diagnosis is difficult and challenging. Radiologic findings are often non-specific. Ultrasonography can differentiate between solid and cystic tumors [3]. US/CT/MRI play a role in establishing the size, extra testicular location, local involvement and distal spread of the lesion; however, they lack specific findings which can aid in diagnosing schwannoma [6] On ultrasound, all tumors are depicted as well-circumscribed heterogeneous mass, well separated from the testis and epididymis [4]. MRI signal is intermediate on T1- weighted images and bright on fat saturated T2-weighted images. The lesions show homogeneous enhancement after injection of gadolinium contrast. The signal changes are compatible with myxoid content of the solid tumor which features help in diagnosis of schwannoma [7].
Differential diagnosis includes adenomatoid tumor, fibroma, lipoma, leiomyoma, sarcoma, malignancy, and other schwannoma subtypes [1,4,7]. The most common extra testicular tumor is adenomatous tumor with peak of 20 and 50 years appearing homogenous and hyperechogenic in ultrasound. Leiomyoma is the second most common tumor of the epididymis showing variable sonographic appearance which may contain calcifications. Both present as slow growing and non-tender scrotal mass [4]. Lipoma are softer and more superficial [7].
Fine need aspirate (FNA) cytology is not often helpful because the tissue architectural information required is not obtainable from cytologic specimen [3]. The diagnosis of the usual type of schwannoma is easy, but diagnosis of variants, like cellular, ancient, and plexiform type is often difficult even on histology [6]. Histologically, PS presents several nodular and lobulated lesions with incomplete circular structures that are surrounded by a thin and stretched perineurium. These are composed of combination of predominantly cellular zone of Antoni A characterized by highly cellular spindle cells with nuclear palisading, and an interspersed loose cellular zone of Antoni B consisting of sparse spindle cells in myxoid stroma [2]. Malignant schwannomas are characterized histologically by perineural and intraneural spread, herniation into the lumina of the vessels and nuclear palisading [3].
S-100 immunostaining is weakly expressed in MPSNT while PS exhibit strong expression of the specific protein. Another differentiating feature is increased number of mitoses and cellular atypia seen in MPSNT [1].
Sexual dysfunction is the patient’s primary concern and is crucial in decision making [1].
The rate of local recurrence is extremely low after complete resection of free surgical margins. Tissue architectural information by either biopsy or excised specimen histology is the only gold standard diagnostic investigation. Local resection is the treatment of choice and regular follow-up is suggested [2].
Conflict of Interest
The author declares no conflict of interest.
Ethical Consideration
Verbal consent was secured from the subject. Subject’s data or patient record will be kept private and confidential. No monetary grants or compensation will be given.
Conclusion
Paratesticular schwannomas of plexiform type are rare and benign. Like other types of schwannoma, they present as slow growing non tender mass. Its diagnostic imaging findings are non-specific. However, MRI is the best modality in the localization of tumor margins. It should be included as a differential diagnosis when presented with the symptoms. It is important to differentiate such from plexiform neurofibroma since this is associated with neurofibromatosis (member of neurocutaneous syndrome). This tumor bears significant risk of malignant transformation. Surgery or excision of the mass remains the gold standard for the diagnosis of PS.
References
- Gkekas C, Kalyvas V, Symeonidis EN, Malioris A, Papathanasiou M, et al. (2019) Plexiform Schwannoma of the Penis: A rare subtype of Genital Schwanomma. Case Rep Urol 1-4.
- Lin T, Wu P, Lin T, Lee T, Lin TY (2010) An infrequent plexifom variant of schwannoma of the glans penis: a rare finding. Asian J Androl 12:455-457.
- Mahobia HS, Shrivastava M, Soni A (2018) Perineo-scrotal schwannoma: A rare case report. International Journal of Surgery Science 2:23-25.
- Kim MJ, Choi SJ, Shim YS, Kim HS, Kim JH, et al. (2014) Intrascrotal and Extratesticular Schwannoma: A Case Report. The Korean Society of Radiology 71:136-138.
- Bhanvadia V, Santwani PM (2010) Intrascrotal extratesticular schwannoma. J Cytol 27:37-39.
- Kumar U, Jha NK (2017) Schwannoma of the penis, presenting as a scrotal mass, rare entity with an uncommon presentation. Urol Ann 9:301.
- Shukla A, Pukar M (2017) Rare Case of Scrotal Schwannoma. Int J Adv Res Dev.
Citation: Alzona AML (2020) Paratesticular Plexiform Schwannoma: A Case Report. OMICS J Radiol 9: 1000327. DOI: 10.4172/2167-7964.1000327
Copyright: © 2020 Alzona AML. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2416
- [From(publication date): 0-2020 - Mar 29, 2025]
- Breakdown by view type
- HTML page views: 1697
- PDF downloads: 719