Case Report Open Access
Pancreatic Tumor Metastasis in the Tongue: Case Report
Bárbara Capitanio de Souza1, Rita Fabiane Teixeira Gomes1, Pedro Guilherme Schaefer2 and Maria Cristina Munerato1,2*1Faculty of Dentistry, Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, Brazil
2Hospital Porto Alegre Clinics (HCPA), Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, Brazil
- Corresponding Author:
- Maria Cristina Munerato
Faculty of Dentistry - UFRGS
Rua Ramiro Barcelos, 2492
Department of Conservative Dentistry, Ramiro Barcelos, 90035-003, RS, Brazil
Tel: +55 51 33598248
Fax: +55 51 33085005
E-mail: mcmunerato@gmail.com
Received date: April 20, 2016; Accepted date: May 23, 2016; Published date: May 28, 2016
Citation: De Souza BC, Gomes RFT, Schaefer PG, Munerato MC (2016) Pancreatic Tumor Metastasis in the Tongue: Case Report. J Interdiscipl Med Dent Sci 4:200. doi: 10.4172/2376-032X.1000200
Copyright: © 2016 De Souza BC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Accounting for only about 1% of all oral malignant lesions, metastatic tumors in the oral and maxillofacial region are relatively rare. More specifically, prevalence of these tumors in the tongue is even smaller, only 0.2%. Pancreatic cancer rarely metastasizes in this region. This case report describes the diagnosis of a malignant pancreatic tumor that metastasized to the tongue. Clinical manifestations are discussed in light of the rare nature and severity of this tumor.
Keywords
Oral metastasis; Pancreas cancer; Oral tongue cancer
Background
Metastatic tumors in the oral cavity are quite rare, representing only 1% of all malignant oral lesions [1-3]. Oral metastases are more often observed in mandible bones, being rarer in soft oral tissues [3]. The most affected soft tissues are the attached gingiva and the tongue, and the prevalence of metastatic lesions on the tongue is of approximately 0.2% [4]. Oral metastatic tumors may originate from primary malignant lesions affecting mainly the lungs, kidneys, breast, liver, thyroid, intestines, prostate, stomach, testicles, female genitals, and the bladder [3]. This case report describes the metastasis of a pancreatic adenocarcinoma on the tongue and discusses the clinical findings and diagnostic importance thereof.
Case Report
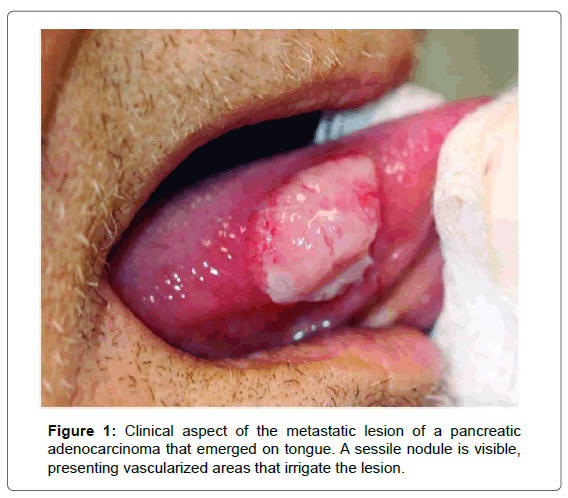
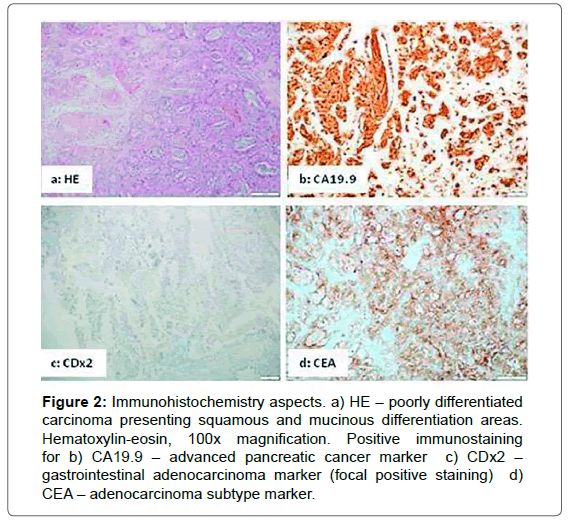
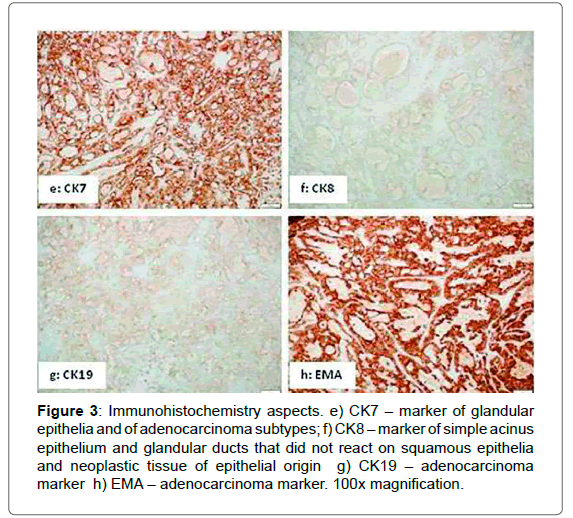
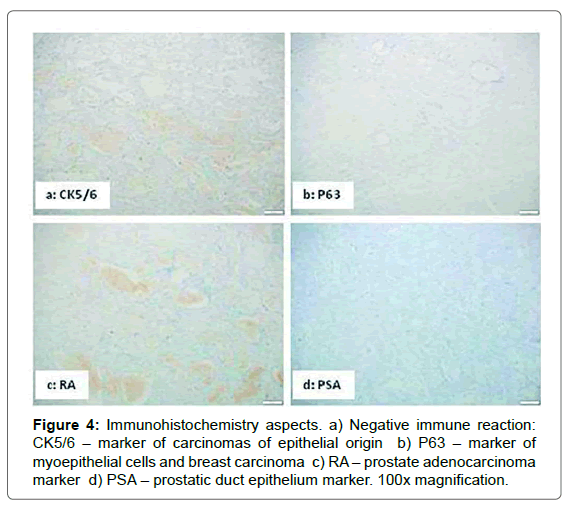
A 66-year-old man with a record of smoking and drinking habits under follow-up treatment for bilateral nephrolithiasis associated with lumbar and abdominal pain in Hospital de Clínicas de Porto Alegre (HCPA), Brazil was diagnosed with stage IV pancreatic adenocarcinoma. The patient was briefed about his clinical condition and referred to palliative oncological treatment. Sixty days into chemotherapy a nodule surfaced on the tongue (Figure 1). The patient was then referred to the Stomatology Service of HCPA for evaluation and differential diagnosis of the lesion. Examination revealed a sessile, fibrous, multilobar nodule measuring 15 mm on the right edge of the tongue. The patient reported pain and difficulty to feed and wear a prosthesis. After local anesthesia the nodule was biopsied and the material collected was submitted to an anatomopathological analysis. In order to improve diagnosis, the material was also submitted to immunohistochemical investigation (Figures 2-4) with the avidin-biotin-peroxidase complex (ABC) based on the percentage of positively stained cells, which confirmed the diagnosis of metastasis of pancreatic adenocarcinoma. The negative control used included marker antibodies of other neoplastic tissues. The patient was receiving palliative chemotherapy, but the unfavorable clinical conditions it was not possible to surgically resect the tumor. Sixty days after diagnosis the patient passed away.
Figure 2: Immunohistochemistry aspects. a) HE – poorly differentiated carcinoma presenting squamous and mucinous differentiation areas. Hematoxylin-eosin, 100x magnification. Positive immunostaining for b) CA19.9 – advanced pancreatic cancer marker c) CDx2 – gastrointestinal adenocarcinoma marker (focal positive staining) d) CEA – adenocarcinoma subtype marker.
Figure 3: Immunohistochemistry aspects. e) CK7 – marker of glandular epithelia and of adenocarcinoma subtypes; f) CK8 – marker of simple acinus epithelium and glandular ducts that did not react on squamous epithelia and neoplastic tissue of epithelial origin g) CK19 – adenocarcinoma marker h) EMA – adenocarcinoma marker. 100x magnification.
Discussion
Regardless of the region affected in the body, malignant tumors may metastasize to the oral cavity, though the first manifestation of the disease may actually be an oral metastasis [1,5]. Primary tumors in the gastrointestinal and genital and urinary tracts or even in the respiratory system are those that most commonly metastasize to the maxillomandibular complex [6]. This scenario is most often observed in the mandible, especially the molar region, since it contains a large mass of hematopoietic tissue and metastasis almost always propagates along the hematological route [7,8]. Among the mouth soft tissues, the attached gingiva is the site most frequently affected, followed by the tongue [1]. The likely routes of metastatic propagation to the tongue are the arterial, venous, and lymph routes. The tongue base is the most affected site, probably due to the presence of a rich network of blood and lymph vessels [3,9].
Pancreatic adenocarcinoma rarely metastasizes to the oral cavity. It may be assumed that the highly aggressive nature of this tumor does not allow for enough time for a metastasis to emerge in this region [2]. Although most patients are already under treatment when oral metastases are detected, these lesions signal the advanced evolution of the disease, which in turn may indicate the need to change the treatment approach, affecting prognosis [1,8]. If the primary tumor is successfully treated, the metastatic lesion should be addressed invasively, with procedures that include surgical resection, radiotherapy, chemotherapy, or a combination thereof. Upon recurrence that is characterized by generalized metastases, the lesion in the oral cavity requires a more conservative treatment approach [10,11].
In this case report the patient’s condition initially required a treatment for nephrolithiasis, and the tumor was diagnosed only when it was too late for a curative approach, when a palliative treatment was therefore offered. The oral metastasis was treated from a conservative perspective as a means to improve quality of life based on pain relief and prevention of hemorrhage, infections, and obstruction of the airways [9-11].
Distant metastasis of primary tumors in the respiratory system and gastrointestinal, genital, and urinary tracts are formed through the mediation of the Baston’s plexus [6]. This plexus includes an avalvular vessel system linked with thoracic and deep pelvic veins that drain the lower end of the abdomen and the regions around breasts and prostate to the internal vertebral venous plexuses [12]. The underlying biological mechanism of metastatic propagation is complex, and starts with a series of coordinated molecular changes that allow cells to lose adherence, acquiring mobility. The tumor cells propagate across the lung venous system, lodging on the associated structures of the maxillofacial complex [8]. The tongue, the gingiva, and parts of the mandible are fed the same blood supply line, suggesting that specific biological factors may play a key role in establishing the nature and the site the metastatic tumor will emerge [12].
The diagnosis of a metastatic lesion in the oral region poses considerable challenge. The practitioner has to be aware of the risks of these lesions, while the pathologist is required to determine the original tumor site based on immunohistochemistry, which is the supplementary method used to diagnose tumors. These efforts help characterize the histogenesis of a tumor, improving the chances of a successful differential diagnosis. This method also may be required in determining the most appropriate therapy to tumors [2]. Such tumors bear consistent clinical relevance, since they may be the first sign of an undiagnosed malignant disease in a remote primary site. They also stand as the first evidence that the tumor is spreading from its main site [13].
Conclusion
Malignant metastases on the tongue are rare, mainly when the primary tumor is pancreatic adenocarcinoma. When diagnosed early, the primary tumor has to be investigated. The approach adopted to treat tongue metastasis is defined considering the primary tumor stage. Immunohistochemistry is essential to diagnose this type of metastasis at this point, since several are the nodular lesions, whether malignant or not, that may evolve on the tongue and therefore be used in the differential diagnosis.
Conflict of Interest
We declare no conflict of interest.
References
- Hirshberg A, Buchner A (1995) Metastatic tumours to the oral region. An overview. Eur J Cancer B Oral Oncol 31: 355-360.
- Kucuktulu E, Kucuktulu U, Guner A, Cobanoglu HB, Mungan S, et al. (2013) Pancreatic Tumor Metastasis of the Tongue. Journal of Case Reports 3: 385-89.
- Lim SY, Kim SA, Ahn SG, Kim HK, Kim SG, et al. (2006) Metastatic tumours to the jaws and oral soft tissues: a retrospective analysis of 41 Korean patients. Int J Oral Maxillofac Surg 35: 412-415.
- Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R (2008) Metastatic tumours to the oral cavity - pathogenesis and analysis of 673 cases. Oral Oncol 44: 743-52.
- McClure SA, Movahed R, Salama A, Ord RA (2013) Maxillofacial metastases: a retrospective review of one institution's 15-year experience. J Oral Maxillofac Surg 71: 178-188.
- Hassona Y, Hughes C, Prime SS (2011) Metastatic tumours of the tongue. Oral Oncol 47: 308-311.
- Irania S, Moshref M, Lotfi A (2004) Metastasis of a gastric adenocarcinoma to the mandible. Oral Oncol Extra 40: 85-87.
- Murillo J, Bagan JV, Hens E, Diaz JM, Leopoldo M (2013) Tumors metastasizing to the oral cavity: a study of 16 cases. J Oral Maxillofac Surg 71: 1545-51.
- Longo R, BaldinI D, Gasparini G (2008) An atypical tongue metastasis of renal cell carcinoma in a patient with metachronous hepatocellular carcinoma. Cancer Therapy 6: 707-710.
- De Menezes JDS, Cappellari PFM, Capelari MM, Gon�§alves PZ, Toledo GL, et al. (2013) Mandibular metastasis of adenocarcinoma from prostate cancer: case report according to epidemiology and current therapeutical trends of the advanced prostate cancer. J Appl Oral Sci 21: 490-495.
- Gil-Julio H, VĂ?¡zquez-Alonso F, FernĂ?¡ndez-SĂ?¡nchez AJ, Puche-Sanz I, Flores-MartĂ?Ân JF, et al. ( 2012) Metastasis of Renal Cell Carcinoma to the Buccal Mucosa 19 Years after Radical Nephrectomy. Case Rep Oncol Med
- Azam F, Abubakerr M, Gollins S (2008) Tongue metastasis as an initial presentation of renal cell carcinoma: a case report and literature review. J Med Cas Rep 2: 249.
- Kumar G, Manjunatha BS (2013) Metastatic tumors to the jaws and oral cavity. J Oral Maxillofac Pathol 17: 71-75.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 14550
- [From(publication date):
August-2016 - Jul 18, 2025] - Breakdown by view type
- HTML page views : 13529
- PDF downloads : 1021