Palliative Care in Qatar, 2008-2016
Received: 19-Dec-2017 / Accepted Date: 27-Dec-2017 / Published Date: 02-Jan-2018 DOI: 10.4172/2165-7386.1000325
Abstract
With the increase of geriatric population, there is rise in demand for services aimed at improving end-of-life care. Palliative care, through its five-component approach, focuses on improving the quality of life and provide relief from complications of serious illnesses. Although a widely accepted concept in other parts of the world, palliative care is a relatively new concept in the Middle East, having been initiated in Qatar only in 2008. The paper discusses the development of palliative care program in Qatar from its initiation in 2008 to its development until 2016, and aims to delineate a stepwise approach for establishment of a successful palliative care program elsewhere, especially in the Middle East, through the model used in Qatar. Primary research data was obtained through analysis of patient demographics and interviews, and secondary data was attained through literature review using PubMed, CINAHL and Google Scholar respectively. Through its multi-faceted approach, aligning with the national health strategy, meeting the rising demands of Qatar’s population, involving a multi-disciplinary team, focusing on education and research, palliative care in Qatar has established a successful model. It is the first one in the region to get Joint Commission International accreditation, thus aligning in par with the international standards and is striving to meet the emerging needs of Qatar’s population and uphold its title as a successful model.
Keywords: Palliative care; Qatar; Middle East; End of life care; Elderly; DNAR
Introduction
By 2050, the global elderly population (defined as people over 60 years old) is projected to double in size from 2015, reaching almost 2.1 billion [1]. With its growing population, Qatar is also following the world’s trend. An earlier projection by the Qatar Statistics Authority for the population to reach 3.2 million by 2050 has been increased due to FIFA World Cup 2022 [2]. In fact, with the current rate of rise in population, the number is expected to reach 4 million by 2022 [2]. Moreover, while in 2010 the elderly population comprised only 2% of the entire population, this number is projected to rise to 20% by 2050 [2]. Thus, the two-fold rise in the total population as well as the mounting proportion of older people will increase the total number of the elderly population in Qatar. With such comes a rise in incidence of a constellation of acute and chronic diseases that will need special care. In addition, the absolute number of people who are suffering from lifestyle disorders like diabetes and obesity (affecting 40% of the current Qatari population) is also increasing, imposing a greater burden on healthcare. The chronic characteristic of these healthcare problems requires prolonged end-of-life care in order to improve the quality of patients’ lives.
When seeking healthcare services, ideally, patients wish to have a sense of control over their situation and over their pain and symptoms. They would also like to strengthen their relationship with their loved ones, and decrease the burden of loss on their family [3]. While it is the prime responsibility of healthcare services to take care of their patients’ demands, what actually happens is quite opposite. More than half of patients suffer moderate to severe pain for >50% of the time during their last three days of life [4]. Approximately 40% of people spend their last 10 days in the intensive care unit (ICU), on a ventilator or in a coma, which hampers their ability to strengthen bonds or say a goodbye to their loved ones [4]. Around 66% of geriatric patients have chronic pain, of which 34% is unrecognized by the physicians [4]. This establishes that, apart from the regular health care services provided by the hospital, there needs to be additional services aimed at improving the quality of life of those patients.
A service which aims at improving this quality of care is Palliative Care (PC). PC is defined by the Center to Advance Palliative Care (CAPC) as specialized medical care for patients with serious illnesses, and focuses on providing patients with relief from their symptoms, pain, and stress, regardless of the diagnosis [5]. PC encompasses a fivecomponent approach comprising of quality of life; patients and family; identification, impeccable assessment and treatment of symptoms; lifethreatening and life-limiting illness; and a holistic approach. Ensuring quality of life requires that the focus be on patient-centered care, respecting the patients’ preferences and values, providing information in an understandable form, promoting autonomy in decision making, and providing physical comfort and emotional support. The patients and families’ component addresses the need to take care of those who are affected while the patient is in the bereavement period. Identification, impeccable assessment, and treatment of symptoms involve knowledge and recognition of the symptoms, following professional evaluation and medical management and holistic intervention by a PC trained team. The fourth component covers lifethreatening and life-limiting illnesses like cancer, diabetes, AIDS, aging, heart diseases, and metabolic diseases to name a few. The holistic approach involves the care of the body, mind, and spirit and is provided by an interdisciplinary team. PC is appropriate at any age and at any stage in a serious illness, and can be provided together with curative treatment [6].
This paper aims to deliver a stepwise approach to describing the development of the PC service in Qatar, which includes the formulation of guidelines to implementation of the plan and periodical monitoring of the performance. The topics of discussion span from governmental support and the national health care strategy, the development of PC in Qatar through 2008-2016, to the scope of future development. Given the successful implementation of the PC program in Qatar, the paper attempts to provide an effective and a viable model for establishing PC elsewhere, especially in the Middle East region.
Methods
Several methods were used to obtain the primary and secondary research data. Primary research consisted of data collection from patient demographics and interviews with prominent individuals in different fields of medicine. Microsoft Excel was used to analyze the data and generate histograms and pie charts. Interviews were held with the Director of the PC unit, medical lawyers, religious leaders, nurses, and other healthcare personnel, thus giving a multifaceted perspective of PC. Secondary research involved literature review, which was done using PubMed, CINAHL, and Google Scholar as databases. The searches were focused towards relevant topics that fall under the subset of PC in Qatar: attitudes and knowledge to PC in Qatar, evolution of the multidisciplinary team, referral patterns, availability of drugs, aggressiveness of treatment, and evolution of Do Not Attempt Resuscitation (DNAR) policies in Qatar.
As the objective of the paper is to illustrate the development of PC in Qatar, the main inclusion criterion was relevance to PC in Qatar. Concerning the attitudes and knowledge to PC and complementary medicine, the search string used was ‘attitude knowledge palliative care cancer and Qatar’. The search yielded 4 hits. The additional inclusion criterion was specific to the topic of attitude or knowledge of PC in Qatar, which narrowed the search down to two papers, both of which were used as they were relevant to the topic at hand. For the evolution of the multidisciplinary team subset, the search string used was ‘(palliative care) and Qatar’, giving 30 hits. However, only 8 of those were directly relevant to Qatar. Out of those, 3 were chosen on the basis that they were concerned with the development of the PC teams. The next subset was the referral pattern of patients. The string entered was ‘Qatar + Palliative + Referral’, which only had one result. The paper was selected as it was relevant to Qatar, and pertains to collecting patient data and using them to standardize a referral program.
Afterwards, the availability of drugs was to be examined. The objectives were to outline the global requirements for a PC service with regards to drugs, the accessibility of these drugs, and the extent of their use. Concerning the global requirements, the International Association for Hospice and Palliative Care (IAHPC) is a branch of the Cancer Control Program of the WHO, which was used as the standard. Therefore, the first search string used was ‘Palliative care AND IAHPC medicine’, giving 14 results. Only one paper was chosen as it provided the global perspective that was required, whereas the remaining 13 were specific to certain regions. The second string entered was ‘opioid accessibility and Qatar’, but as it returned no results, the more general string used was ‘opioid accessibility and Middle East’ on the condition that only the papers which were relevant to Qatar would be used. One such article fit these criteria out of 15, and was used. Finally, the string ‘narcotic use and Qatar’ was entered for the last objective, which gave 18 papers, of which one was used as it was directly pertinent to both Qatar and the topic at hand.
Another subset was the policies dictating the aggressiveness of treatment. The first search string entered was ‘("Palliative Care"[Mesh]) and "Qatar"[Mesh]’ which gave 5 results. The extra inclusion criterion was relevance to the treatment strategies, narrowing down the search to 3 results, of which all were used. As PC patients in Qatar tended to be cancer patients, a second search was conducted with the string ‘("Neoplasms"[Mesh]) and "Qatar"[Mesh]’ to account for the treatment of cancer patients who eventually required PC. The search resulted in 43 hits. After applying both inclusion criteria, in addition to a third one – which the papers should pertain to only those cancer patients who were receiving PC – only one paper remained which was deemed relevant and used.
The final subset to be discussed is the evolution of the DNAR policy. The first attempt used the string ‘((DNR) OR DNAR) and Qatar’, but that yielded no results. More general terms were sought, and the string ‘“end of life” and Qatar’ gave 9 results, but only 3 were directly relevant to Qatar. One exclusion criterion was applied: those papers that concern with subjective experiences of patients and nurses and were irrelevant to the DNAR policy of Qatar, and only one paper remained and was used. In order to get a more complete picture of the development of the DNAR policy, interviews were conducted with the Qatar Faculty of Islamic Sciences (QFIS) to provide the Islamic perspectives on DNAR, and to appreciate how the religious and local cultural contexts shaped the DNAR policy in Qatar.
Although the literature provided a plethora of information on the development of PC, there are no publications concerning PC in Qatar after 2014. In order to acquire the latest relevant data, interviews were conducted with the National Centre for Cancer Care and Research (NCCCR) in Qatar to acquire data on the development of the aforementioned PC subsets from 2008 up to and including December 2016. The interviews completed the study with data which was not published, even until 2014. The Qatar National Health Strategy for 2017 – 2021 was also acquired from the NCCCR. Finally, the raw data from patient experiences was acquired from the NCCCR and analyzed according to appropriate statistical measures.
Results
Development through 2008-2016
PC is still a novel concept in the Middle East, having initially been introduced in Saudi Arabia in 1992, only to be followed and adopted recently by other countries in the region.
The dedicated PC unit was developed as part of the National Cancer Strategy (NCS) for Qatar, launched in 2011 by the Supreme Council of Health, with the goal of putting Qatar at the forefront of cancer care in the Gulf region as well as in the world [7]. Based on international evidence and acting in accordance with World Health Organization (WHO) standards, the strategy detailed the plan in improving provision of facilities to cancer patients in Qatar in terms of care, infrastructure, and practice. A total of 62 recommendations were made to be implemented, in areas spanning from education, prevention, early detection, treatment, to ongoing care, for which PC is featured as a critical component [8]. Other recommendations were also made in the areas of measuring performance, improving the workforce, and promoting research. The execution of such recommendations has been reliant upon and collectively accounted by the Ministry of Public Health, Hamad Medical Corporation (HMC), and the Primary Health Care Corporation [2].
The PC unit in Qatar has grown from drafting of policies to a fullfledged unit with JCI clinical program accreditation in the years 2012 and 2015 [9]. In Qatar, and under the main health care provider HMC, Al Amal PC service was the first and only palliative service opened its doors in July 2008 as a 10-bed specialized unit [7]. The years 2009-2010 witnessed the formulation of a PC committee, formation of a multidisciplinary team and a manpower and capital budget proposal. In 2011, a decision was made to plan for JCI clinical program accreditation, along with formulation of clinical guidelines, policies, pathways, and initiation of patient and family education [9]. The palliative program received its first JCI accreditation in 2012; and incorporated education and special training required by the nurses and physicians to serve the program better [9]. Currently, the service focuses on providing supportive care to cancer patients, which comprises 10% of all the patients seeking healthcare in Qatar [2].
Along with enactment of the NCS was the implementation of its accompanying investment plan, detailing the expenditure over a period of five years. The investment plan was divided into three main groups, notably staffing and wage costs (QAR 335 million), operating expenses (QAR 962 million), and capital costs (QAR 907 million), for an estimated total of QAR 2,204 million [2]. Pertaining specifically to PC were the refurbishment of old PC unit in Al-Amal hospital including space for multidisciplinary teams, and the construction of a new specialist PC unit, in addition to broader investment in staffing and the creation of new research programs at HMC [2]. The following sections discuss in more depth the many aspects of patient care and the development of the PC unit from 2008 to 2016.
The referral pattern
In 2012, it was recognized that most patients with cancer had no suboptimal access to PC in Qatar. Referral to PC was not standardized and patients did not receive counseling due to absence of predictive criteria of patients admitted to the cancer center. In addition, records indicated a significant number of patients dying within a month of their admission into PC, reflecting delayed utilization of PC services. Early referral is important, because administration of palliative measures has been shown to have positive influence on quality of life, patients and family satisfaction, as well as financial survival outcomes. The biggest hurdles to initiation of PC were the physicians' inability to assess need for palliative consultation due to personal attitudes, the absence of standardized criteria, and resistance to referral by the patients’ families.
A PC referral screening tool was developed to identify oncology patients appropriate for palliative consultation as well as patients appropriate for transfer into PC. The screening tool utilizes a scoring system that takes into account the stage of cancer, presence of comorbidities and uncontrollable symptoms, social limitations, and an Eastern Cooperative Oncology Group (ECOG) performance score [10]. A score of more than 5 out of 10 indicates PC consultation, and 7 indicates PC transfer [10]. The scoring system is detailed in Table 1.
| Scoring Items | Points | Score* |
| Presence of metastatic/relapsed/refractory or locally advanced cancer | 2 | - |
| ECOG performance status score | 0-4 | - |
| Presence of one or more serious complications of advanced cancer usually associated with a prognosis of <12 months (e.g. Brain metastases, hypercalcemia, spinal cord compression) | 1 | - |
| Presence of one or more serious comorbid diseases also associated with poor prognosis (e.g. moderate-severe COPD or CHF, dementia, AIDS, end-stage renal failure, end-stage liver cirrhosis) | 1 | - |
| Symptoms (e.g. pain, nausea & vomiting, SOB) uncontrolled by standard approaches for more than 3 days standard approaches for more than 3 days | 1 | - |
| Patient/family/social/psychological/nutritional limitations (caregiver limitations, inadequate social support, financial limitations, limited access to care, TPN/PEG) | 1 | - |
| Total | 0-10 | - |
| * A cut point of 5 has the best predictive value for palliative referral/consultation; ** A cut point of 7 has the best predictive value for palliative care Reason for non-referral if score>5 or >7 | ||
Table 1: Palliative care referral scoring.
Following application of this tool, consultations as well as transfers to PC showed a marked increase. Prior to application of the screening tool, 68% of patients who deemed appropriate for consultation by the PC team did not receive such service, contrasted with only 16% after the implementation of the screening tool [10]. This has had an impact on multiple aspects of patient satisfaction, quality of life and symptom management. Increase in referral has also contributed to improved patient, family and physician education.
Patient demographics
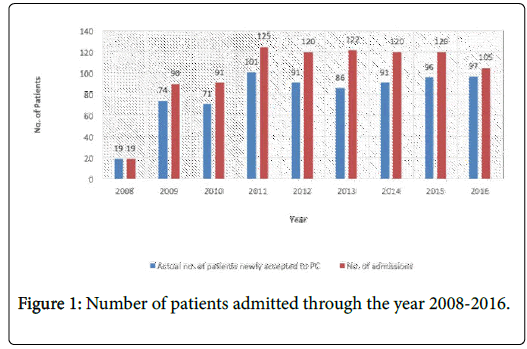
The number of patients admitted to the PC unit have increased from 2008 to 2009 but have remained almost stable thereafter, as shown in Figure 1. The eligibility criteria for admission requires the patients to be above 14 years of age, with a confirmed diagnosis of cancer and survival expectancy of more than 48 hours.
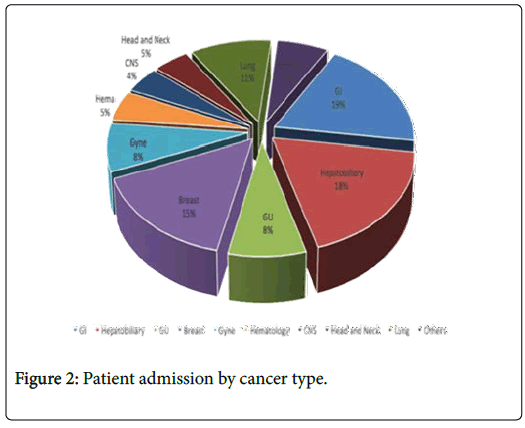
Figure 2 shows the percentage of patients admitted by cancer type in the PC unit. Cancer is the third leading cause of death in Qatar with an incidence as high as 1,466 cases in 2015 [11]. The highest incidence is accounted for by gastrointestinal and hepatobiliary cancer, followed closely by breast cancer [12]. The establishment of the PC unit and the DNAR policy in 2011 has led to a decline in the aggressive end-of-life care that was administered to the cancer patients earlier. This is helping fulfill some of the patients’ wishes, which includes avoidance of inappropriate prolongation of life and having an opportunity to strengthen their relationship with their loved ones.
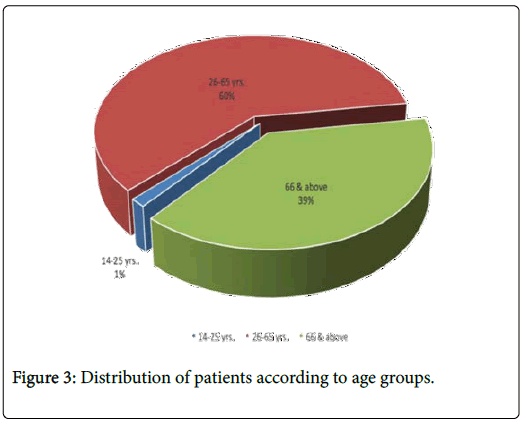
In terms of patient admission by age, the majority of patients are 22–65 years old (61%), while 37% of patients are 66 years and older (Figure 3). The proportion of patient populations in different age groups is not reflective of the age distribution in the normal population of Qatar. This can be explained by the increase in the incidence of cancer in the elderly population.
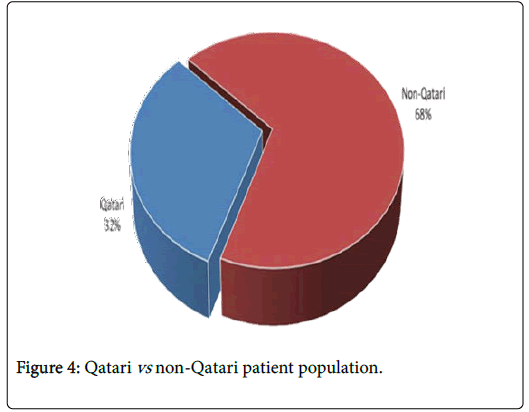
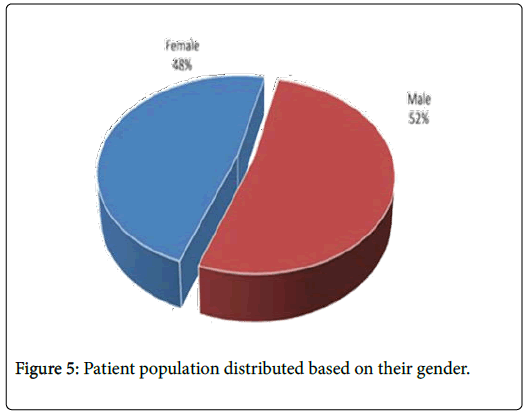
Further comparison of the patient population in terms of their nationalities (Qatari versus non-Qatari), reveals that the distribution is reflective of the country’s population distribution (Figure 4). The distribution of the patient population based on gender has been nondiscriminatory, as seen with the closely shared percentages between men and women - 52% and 48% respectively (Figure 5).
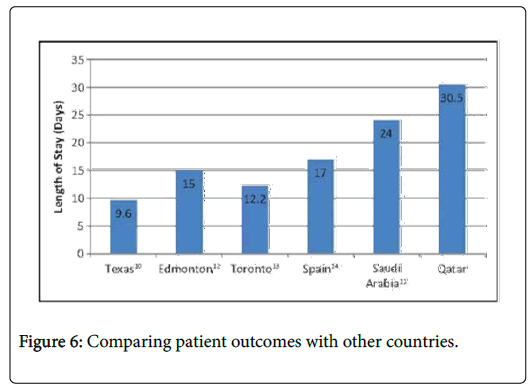
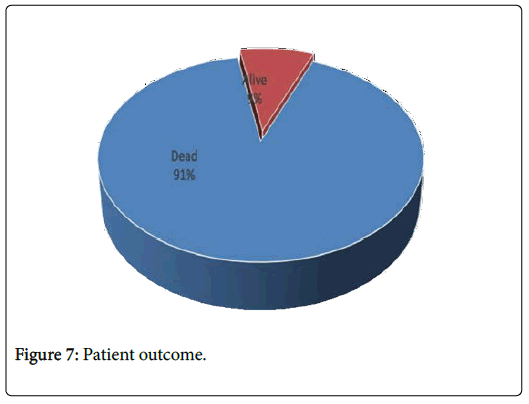
When comparing the patient outcomes to other countries, Qatar has one of the highest reported length of stays (30.5 days) (Figure 6). This can be explained by a lack of alternative PC/out-of-hospital chronic facilities (e.g. hospice, specialized nursing support), a cultural view that patients benefit more from staying in the hospital for longer periods, and the lack of competency to provide end-of-life care by the families. Almost 91% of patients die in the PC unit, with mean survival of 32 days and median survival of 16 days (Figure 7).
Evolution of multidisciplinary team
As the care of PC patients involves the consideration of many aspects, patients are cared for by a multidisciplinary team. Every patient has one specialized consultant and one clinical nurse specialist assigned to him/her, and the remainder of the team consists of a shared staff: a clinical pharmacist, a dietitian, a physiotherapist, a psychologist, a social worker, and a spiritual advisor, the last of which is a service shared with HMC [1].
As the demand for PC increases, the unit intends to expand its team ultimately through the training of human resources. From 2011, the University of Calgary in Qatar offers a Masters in nursing program which trains and graduated them to be Clinical Nurse specialists in Oncology and PC. The unit has also brought nurses from the UK temporarily to train local nurses and develop their capacity to serve as PC nurses [13].
Furthermore, to improve the pharmacy aspect of patients’ care, an academic cross-appointment program was founded between the College of Pharmacy in Qatar University (whose program has been accredited by the Canadian Council for Accreditation of Pharmacy Programs) and NCCCR in 2013 [14]. The cross-appointment selects faculty members to be established in the clinical practice, in addition to acting as preceptors for students on four-week internships [14]. They are on site two days a week [14].
Education and research
Given the dependence of quality of care upon the performance of the medical staff, the PC unit has dedicated considerable time in recruitment, training, and education of its staff. In fact, as part of the NCS, better coordination between primary and secondary health care is sought after. For instance, from 2011 to 2015, educators from the United Kingdom were recruited to equip staff with the necessary clinical expertise, with primary health care education as a priority. The ultimate goal focused on getting qualified specialist cancer nurses within primary health care centers who can facilitate early detection and referral from primary care [2]. In terms of physician staffing, besides recruiting consultants from abroad to allow greater specialization in PC, efforts have been allocated to encourage local family physicians to develop special interest in cancer by providing additional training and education. In addition, physicians within psychiatric specialties have been made more aware of differences between palliative and non-palliative patients, enhancing the effectiveness of patient support. Finally, the strategy is aimed at involving more new and locally trained doctors from Weill Cornell Medicine - Qatar and Qatar University medical schools to serve the growing needs of the community [2].
The palliative unit in and of itself has been involved in teaching programs that have been expanding over the past years. These include the training of anesthesia, hematology/oncology, and geriatric fellows, in the hopes of bridging different medical disciplines and bringing them to serve palliative patients. In addition, in January 2017, a 2-years dedicated fellowship program was initiated in the PC unit. In addition, the PC unit gives year-long training to medical students at Weill Cornell Medicine–Qatar to complement their growth and encourage future involvement within the PC program [2].
Also, a translational research program has been developing in order to keep pace with the latest scientific progress in cancer, with topics spanning from diagnostic approaches, genetics, treatment to epidemiology. The program involves collaboration between different partner organizations, including Qatar Foundation, HMC, Qatar Science and Technology Park, Qatar University, Weill Cornell Medicine - Qatar, and the University of Calgary [2]. One of the most recent ongoing research projects include a study on distress amongst cancer patients during diagnosis treatment and later stages to determine if there is any change in the level of distress along the disease trajectory, and to analyze the possible contributing factors.
Drug availability
In 2007, the IAHPC developed a list of essential medicines for PC in response to a request from the Cancer Control Program of the WHO [15]. This collaborative effort put together a list of medications that addresses the predictable symptoms, the most prominent being pain, of patients in hospice and PC units. Seven essential opioid medications recommended, including: immediate release oral morphine, controlled-release oral morphine, injectable morphine, oral immediate release oxycodone, transdermal fentanyl, and oral methadone [15,16]. By 2013, Qatar had all of the seven essential opioids as advised by the IAHPC, along with extra opioid analgesics such as combined paracetamol and codeine forms and sublingual fentanyl (100 & 200 mcg) were added to the list of opioid while the other medications were <25% of the actual drug cost [16].
The current Qatar National Health Strategy has outlined the need to educate health professionals regarding appropriate use of narcotics, and the importance of implementing strict regulations on trafficking, prescription and access [2]. In general, patients in either the inpatient or outpatient setting could have access to opioids, but only with special authorization as deemed necessary [17]. Currently, special prescription forms are required to prescribe opioids to both cancer and non-cancer patients [17]. Gaining access to these forms is easier for non-cancer patients as family physicians and general practitioners are eligible [17]. However, for cancer patients in Qatar, only oncologists and surgeons can obtain a special authorization permit to prescribe opioids to cancer patients, while family physicians are strictly prohibited. Currently, no emergency prescriptions are allowed by nurses or pharmacists. The available dispensing sites for prescription opioid analgesics are hospital pharmacies, while health centers throughout Qatar have injectable morphine available for emergency, non-prescription situations [15,16]. Overall, Qatar has many available opioids for use, but simultaneously has very strict regulations over eligibility, prescriptions and access.
Aggressiveness of treatment
Preliminary analysis of the aggressiveness of end-of-life care in Qatar, and of the GCC, was conducted by Azza et al., by analyzing deaths from cancer from January 1st, 2009 to December 31st, 2013. Indicators for aggressiveness were based on dosage of chemotherapy received in the last 30 days before death, the number of hospital and ER and ICU admissions 30 days before death, and the number of deaths in acute care [17]. Data showed that aggressiveness did decrease within this time from 82% of patients getting treated in ICU’s to 71%. This figure however is still much higher than other countries such as the United States, Canada and in Europe and Asia. This is attributed to a lack of other PC facilities, skepticism from oncologists about PC. The decline of aggressive end of life care is attributed to the PC unit opening at Al Amal hospital, the introduction of the DNAR order in 2011 and the addition of a modified National Comprehensive Cancer Network Screening hospitalized patients. The screening tool has led to earlier diagnoses and referral from 2012 [18].
Another report stated that most cancer patient deaths in Qatar occurred at the hospital, with only 0.4% of deaths occurring at home [19]. This is further compounded by the fact that many physicians only refer 50% of terminal cancer patients that they receive to PC, and only 36.7% admitted to receiving training in PC, although 57.8% reported knowing how to handle end-of-life care [20]. These factors might further contribute to the aggressiveness of treatment, with more patients seeking medical attention that might not be necessarily helpful in alleviating pain associated with the disease.
Evolution of DNAR policy in Qatar
The right of terminally ill patients to give advanced directives related to their treatment such as that of a Do-Not-Attempt- Resuscitation (DNAR) Order has been instituted in Qatar’s Palliative Care Protocol in 2004, adopted from the one in Saudi Arabia. Further revisions have been made until the major health institutions including HMC and the primary health centers have now incorporated the protocol [21]. HMC defines this policy as a legal right for a patient, given the circumstance of deterioration or imminent collapse, to be withheld from the following interventions: chest compression, defibrillation, endotracheal intubation, assisted ventilation, and administration of cardiac drugs.
The scope of the DNAR policy is one that has evolved over the years, as it tries to overcome reluctant and hostile attitudes from society, religion, and culture. For instance, this policy carries a universal stigma for having to hasten a loved one’s death. According to a retrospective, population-based study that looked into registered cancer deaths in Qatar between 2006 and 2012, Qatari families tend to refuse DNAR orders due to the family’s demand that every medical intervention – no matter how aggressive – that could prolong the patient’s life be done by the healthcare team [18]. It is notable that the family’s core values supersede religious beliefs, which support DNR status in terminally ill patients [22]. Suffering is an inseparable part of life in Islam and being issued a DNAR status is only permissible in the presence of a medically-approved terminal prognosis as it takes into account the urgent need for allocating such scarce resources to other patients who could greatly benefit from supportive care [23].
The taboo is further confounded by the ambiguity of medicolegal and ethico-legal laws regarding DNAR in nations predominated by Islam followers, leaving care to fall solely on hospital guidelines. As these guidelines are not always legally binding, physicians are often faced with having to acquiesce to patient’s family wishes of refusing to place a patient on DNAR status [23]. It is routine that the primary attending physician discuss DNAR policies with the patients; then, two other physicians who belong to the same department are required to mediate and decide futility [24]. Moreover, the JCI that oversees patient safety and quality of health care internationally requires the signature of the patient or a key member. This member will most likely be a family member, who in some cases would have to bear the guilt of “signing upon one’s death”.
This emotional burden is relieved by the presence of a strong multidisciplinary team that involve social workers like religious chaplains in Qatar [17]. However, during instances when there is a discord between the family’s insistence on aggressive treatment and the doctor’s plea for the patient to die in peace, a meeting is held with doctors, nurses, social workers, and spiritual advisors to encourage the family to not withhold DNR. Should the family remain adamant about making the patient continue receiving aggressive treatment and consequently prolong suffering, an ethical committee takes care of such cases. More importantly, the patient’s concern is prioritized given his/her sufficient competence and autonomous level, placing the priorities and decision of the patient’s family second.
In conjunction with better patient education through early personal discussion with the physician and exposure to health awareness videos and pamphlets about the decision of putting the patient under DNAR status, the DNAR policy has significantly reduced mortality and morbidity among patients who undergo aggressive interventions in Qatar.
Attitudes of healthcare professionals towards the palliative program
A 2012 survey conducted at NCCCR targeting oncology physicians reveals that fewer than 50% of doctors had certified training in PC and only slightly more than half of them reported confidence and competence in providing quality medical care to terminally ill patients. In fact, only about three fifths of physicians were aware of the clinical guidelines about PC and about the same percentage of them applied such guidelines in their routine clinical care. However, the majority of doctors promisingly expressed interest in learning more about this field and advocated for establishment of better PC service in Qatar in the future [19].
In the same year, oncology nurses working at NCCCR were given a similar survey inquiring about their attitude and knowledge of PC. Despite that 60% of nurses had more than a decade of clinical experiences, only one third of them had formal training in PC. Only about half of the nurses indicated that they were familiar with the WHO ladder for pain relief, knew the Palliative Performance Scale and the Edmonton Symptom Assessment System. As compared to the physicians’ attitudes, half of the nurses indicated only some kind of interest in palliative and 17% indicated of no interest. Majority of them attributed their unpreparedness for PC to lack of time, interest and financial issues [25].
Discussion
PC is considered an integral part of comprehensive cancer care programs. Generally, PC is still an emerging field in Middle Eastern countries with different degrees of development amongst the respective countries, namely Qatar, Kingdom of Saudi Arabia (KSA) and Jordan. There is some overlap between the systems, but a few differences exist.
KSA is the regional pioneer in terms of the formation of the PC unit. Its PC program began in 1992 in King Faisal Specialist Hospital and Research Center (KFSHRC), Riyadh [26]. In Jordan, 2001 marked the year of the Jordan Palliative Care Initiative (JPCI), a WHO initiative to set forth a comprehensive PC service in Jordan. By October 2004, the first PC team was formed in the King Hussein Cancer Center (KHCC) [27]. A few years later, in 2008, the PC program in Qatar was initiated, modeled after the KSA’s program.
In terms of the facilities offered at the PC units, both Al-Amal PC center in Qatar and KFSHRC in KSA have 10 beds dedicated to the PC units [7,28]. The PC beds in Qatar are exceptionally well-equipped with state-of-the-art equipment and comforting surroundings. In contrast, the PC unit in KHCC has 8 beds, but extra patients could be admitted to a different inpatient ward and still be provided with similar service. In Qatar, the vast majority (93%) of the PC patients that are referred to the PC unit come from the oncology department in Hamad General Hospital [7]. In contrast, slightly more than half (66%) of patients in the PC unit of KFSHRC hospital in Riyadh are referred from the emergency department [28]. KHCC’s PC unit in Jordan has a similar pattern of patient population [28]. In all three countries, PC has been integrated into the healthcare system, and is well-recognized amongst the physicians as a suitable alternative to curative care.
Another important factor to consider is the Length of Stay (LOS) of the patients in the inpatient PC unit. This parameter helps quantify the efficiency of the program and enables comparison with other countries, and hence standardization. Amongst the three countries, Qatar has the highest LOS with 30.5 days, Jordan has the lowest LOS with 11 days, and KSA has a 24.8 days average LOS [28]. The main reason for the extended LOS in Qatar may be due to the absence of out-of-hospital chronic facilities such as hospice care and specialized nursing facilities. The patients thus stay in the hospital until they expire and such contributes to the increased mortality rate in these PC settings [7,28]. In Jordan, however, the relatively short LOS could be attributed to the numerous admission criteria and the elaborate MDT assessment of the potential patients prior to admission, which could result in late involvement of PC and artificially shorten the LOS [29].
Overall, the development of PC in the Middle East is considered relatively recent due to the long struggle with opiophobia regionally. The increased acceptance of PC in the region stems not only from its proven effectiveness worldwide, but also from the public’s general awareness about it and its benefits. In Qatar, specifically, the demand on the PC unit has dramatically increased over the last few years in numbers that exceed the unit’s capacity, calling for further expansion and increased efficacy and is indicative of a successful future for the unit.
An evaluation of Qatar’s PC program in accordance to a global perspective and standard is also warranted. The WHO guidelines for the provision of PC include the supply of nation-wide high-quality end-of-life care that handles different diseases and involves adequate pain management strategies spanning all healthcare levels. The WHO also refers to a tripartite strategy of addressing the physical, psychological and social needs of the patient, the family or caregivers and the providers themselves [30]. The WHO espouses particular standards for assessment of a country’s PC system, so as to better understand its strengths and weaknesses, and develop a strategy moving forward according to established guidelines.
According to WHO’s recommendation for PC development, the country should start by asking where they are now. It is important to assess the number of people in need of cancer PC, the needs of patients, health-care providers and family caregivers, the existing PC plan and activities and finally, understand its social context [2] Secondly, the country should decide where they want to be, i.e. the end goals of its PC program. It is important to define the target population for PC, identify gaps in PC services, set goals and objectives for PC, assess feasibility of intervention and consider ethical issues [2]. Last but not least, the country should determine how they could reach these goals. To be more exact, this can be broken down into smaller questions such as: how to bridge the gaps in PC, how to raise the necessary resources, how to create PC teams, how to educate caregivers, how to educate the general public and policy-makers, how to ensure the availability of essential drugs, how to develop PC standards and how to evaluate and monitor the PC plan and activities [2].
The first two questions have been addressed by the extensive discussion regarding development of the PC unit from 2008-2016, from the establishment and implementation of the NCS, the establishment of the JCI-accredited PC unit run by a multidisciplinary team, and the enrichment of the facilities via recruitment, education, and research [2]. In response to the third question, while there are ample resources to address the emerging needs of the population, it can be postulated that adequate response to such needs would mirror a steady expansion of the unit and effectively provide sufficient end-oflife care. In fact, Qatar has begun cementing its PC framework with the launching of schemes such as the NCS [9]. Qatar’s aims therefore are currently focused on the PC of cancer, but hope to diversify to other chronic diseases to address the needs of a growing and aging population.
The strengths of Qatar’s current PC strategy are the emphasis on the development of current facilities and resource allocation, and the intense ongoing research being done on addressing the changing healthcare needs of Qatar’s diverse population. The JCI accreditations of the NCCCR PC unit in the years 2012 and 2015 are proof of Qatar’s ongoing commitment to becoming the standard of PC and of healthcare in the region. Political support for the development of healthcare is evidenced by Qatar’s ambitious yet commendable growth in line with the Qatar National Vision for 2030, which strives to build a comprehensive world-class healthcare system whose services are accessible to the whole population [31]. Nonetheless, it remains to be seen whether support for PC will continue to increase versus the more popular choice of aggressive treatment for end-stage conditions. Possible social and religious factors also present obstacles to policy implementation, especially with regards to DNAR orders as was previously discussed.
Possible future steps to be taken would include improving rates of early referral under the National Comprehensive Cancer Network Screening tool as has already been introduced and proven to be effective. Other long-term measures could include opening up PC services specializing in diseases other than cancer, increasing the number of beds in the existing PC unit, and introducing policies for moving patients back home or introducing hospice care facilities for long term care. Awareness about PC as an appropriate alternative for end-of-life care should be increased amongst doctors, patients and families alike. Infrastructure (the likes of which are already being put in place) to allow for the seamless transition of patients from acute care facilities such as the ICU and ER to the PC unit should be maintained. All of these would help mediate the increased sensitivity of Qatar’s healthcare system, as is evident in the developments of recent years, to the needs of its growing population while reducing unnecessary suffering and loss of quality of life through aggressive end-of-life treatment.
References
- Hassan AA (2014) Palliative care service in Qatar. Supreme Council of Health.
- Silver JK, Raj VS, Fu JB, Wisotzky EM, Smith SR, et al. (2015) Cancer rehabilitation and palliative care: Critical components in the delivery of high-quality oncology services. Support Care Can 23: 3633-3343.
- Walling AM (2010) The Quality of care provided to hospitalized patients at the end of life. Arch Intern Med 170: 1057-1063.
- Morrison RS, Meier DE (2015) America's Care of Serious Illness. Center to Advance Palliative Care.
- World Health Organisation (2014) Worldwide Palliative Care Alliance. Global Atlas of Palliative Care at the End of Life, pp: 54-55.
- Al-Kindi SG, Zeinah GFA, Hassan AA (2013) Pattern of hospitalization of patients with cancer in an acute palliative care setting: Qatar’s experience. Am J Hosp Palliat Med 30: 25-28.
- Ministry of Public Health (2017) National Cancer Strategy. State of Qatar.
- National Cancer Program (2016) The First Step On The Path To Excellence: National Cancer Strategy, 2011 - 2016 Review.
- Ministry of Public Health (2017) MOPH Announces the 2015 Cancer Incidence Data. State of Qatar.
- http://www.ucalgary.edu.qa/sites/default/files/master%20of%20nursing%20-%20v3.pdf
- Wilby KJ, Mohamad AA, Alyafei SA (2014) Evaluation of Clinical Pharmacy Services Offered for Palliative Care Patients in Qatar. J Pain Palliat Care Pharmacother 28: 212-215.
- Lima LD, Doyle D, Macdonald N, Krakauer EL, Lorenz K, et al. (2010) Ensuring palliative medicine availability: The development of the IAHPC list of essential medicines for palliative care. J Pain Symptom Manage 33: 521-526.
- Cleary J, Silbermann M, Scholten W, Radbruch L, Torode J, Cherny NI (2013) Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in the Middle East: A report from the Global Opioid Policy Initiative (GOPI). Ann of Oncol 24: 51-59.
- Hassan AA, Bharani T, Helmy IH, Menik AS, Othman YA, et al. (2017) Developments of Palliative Care in Qatar.
- Hassan AA, Mohsen H, Allam AA, Haddad P (2016) Trends in the aggressiveness of end-of-life cancer care in the state of Qatar. J Glob Oncol 2: 68-75.
- Hong JH, Rho S-Y, Hong YS (2013) Trends in the aggressiveness of end-of-life care for advanced stomach cancer patients. Can Res Treat 45: 270-275.
- Mohsen H, Haddad P, Allam A, Hassan A (2014) Patterns in place of cancer death in the state of Qatar: A population-based study. PLoS One 9: e109615.
- Zeinah GFA, Al-Kindi SG, Hassan AA (2012) Attitudes of medical oncologists in Qatar toward palliative care. Am J Hosp Palliat Med 30: 548-551.
- Begum A (2013) Using a screening tool to improve timely referral of patients from acute oncology-haematology to palliative care services. BMJ Qual Improv Rep 2.
- Ghaly M (2016) Islamic perspectives on the principles of biomedical ethics. London: World Scientific Publishing (UK) Ltd.
- Ghaly M, Othman YA, Soliman MM (2016) The islamic perspective on palliative care and DNR.
- Al-Kindi SG, Zeinah GFA, Hassan AA (2014) Palliative care knowledge and attitudes among oncology nurses in Qatar. Am J Hosp Palliat Med 31: 469-474.
- Nixon A (2004) Palliative care in Saudi Arabia. J Pain Palliat Care Pharmacother 17: 45-49.
- Stjernswärd J, Ferris FD, Khleif SN, Jamous W, Treish IM, et al. (2007) Jordan palliative care initiative: A WHO demonstration project. J Pain Symptom Manage 33: 628-633.
- Alsirafy SA, Hassan AA, Al-Shahri MZ (2009) Hospitalization pattern in a hospital-based palliative care program: An example from Saudi Arabia. American J Hospice Palliat Med 26: 52-56.
- Shamieh O, Hui D (2015) A comprehensive palliative care program at a tertiary cancer center in Jordan. American J Hospice and Palliat Med 32: 238-242.
Citation: Bharani T, Li Y, Helmy I, Menon L, Arachchige SM, et al. (2018) Palliative Care in Qatar, 2008-2016. J Palliat Care Med 8: 325. DOI: 10.4172/2165-7386.1000325
Copyright: © 2018 Bharani T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Conferences
42nd Global Conference on Nursing Care & Patient Safety
Toronto, CanadaRecommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5908
- [From(publication date): 0-2018 - Dec 23, 2024]
- Breakdown by view type
- HTML page views: 5191
- PDF downloads: 717