Editorial Open Access
Palliative Care Gains Roots in China
Lili Tang1 and Michael Silbermann2*1Department of Psycho-oncology, Key Laboratory of Carcinogenesis and Translational Research(Ministry of Education), Peking University Cancer Hospital & Institute, Beijing, China
2Executive Director and Professor, Middle East Cancer Consortium, Israel
- Corresponding Author:
- Michael Silbermann Executive Director and Professor Middle East Cancer Consortium, Israel Tel: 972-482-447-94 Fax: 972-483-463-38 E-mail: cancer@mecc-research.com
Received Date: May 03, 2017; Accepted Date: May 05, 2017; Published Date: May 10, 2017
Citation: Tang L, Silbermann M (2017) Palliative Care Gains Roots in China. J Palliat Care Med 7:e140. doi:10.4172/2165-7386.1000e140
Copyright: © 2017 Tang L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
In China over the past decade, palliative medicine has emerged as a new program. Development of this program requires attention to current opportunities, obstacles and cultural concerns. A selected review showed that there is an urgent need for palliative care in mainland China. Several challenges to implementing palliative care service in China include: (1) cultural perception and misunderstanding of palliative care; (2) lack of professionally trained health-care providers; (3) administrative and policy problems; and (4) limited funding for palliative care and research. More efforts should be made in clinical practice, education and research to develop and implement palliative care in mainland China.
Keywords
Cancer; Palliative care; Psycho-oncology; Hospice; Culture; China
Introduction
The WHO (World Health Organization) has changed the definition of palliative care from relating to late stage care only, to an approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness through the prevention and relief of suffering by means of early identification and accurate assessment and treatment of pain and other problems, whether physical, psychosocial and spiritual. It has been widely recognized that palliative care should be applied as early as possible in the course of any chronic, and ultimately fatal illness [1].
China is the most populous country in the world, with roughly 1.37 billion people [2], and has the largest low-middle class in the world. An estimated 4.292 million new cancer cases and 2.814 million cancer deaths occurred in China in 2015 [3]. Palliative medicine is in its infancy in China and faces many challenges and barriers [4,5].
Academic Institutes Serving Palliative Medicine in China
Hospice and palliative care is an emerging specialty in China. In 1988, the first research center for palliative care in China was established in Tianjin Medical University. This was followed two years later by the first hospice and palliative facility. One of the most important steps in the development of palliative care was the establishment of the Chinese Association for Hospice and Palliative Care in 1993, which can be considered as a milestone in the history of palliative care in China. Three years later, the Chinese Journal of Hospice and Palliative Care was founded, which largely promoted the development of hospice and palliative care in Chinese academic settings. In 2004, the Ministry of Health further stipulated that the existence of hospice and palliative care be one of the accreditation standards for general hospitals [6]. This accelerated the establishment of palliative care centers throughout Chinese hospitals. Yet, despite the increasing awareness of the importance of hospice and palliative care for patients with terminal cancer, palliative care remains relatively underdeveloped in China.
Two other academic institutes are involved in palliative care: the Committee for Rehabilitation and Palliative Care for Cancer in the Chinese Society of Clinical Oncology, and the Chinese Association for Life Care. The academic work of these institutions and organizations has promoted the development of palliative care in China independently of direct governmental involvement. Palliative care units in teaching hospitals connected to universities, hospitals in provinces, municipal hospitals, and health centers in the community are divided into two categories: ward care within the hospital, and home care in the community. Palliative ward services consist of 10 units that are located in Chengdu, Shanghai, Beijing, Kunming, Tianjin, and other major cities. Palliative ward care in Shanghai and Beijing is mainly located in the community health centers, such as the health center in the Lingfeng community, Zabei district; the geriatric hospital of the New Pudong district in Shanghai; Beijing Chaoyang Men’s Hospital; and the Songtang Hospice in Beijing.
Psychosocial Aspects of Palliative Care Service
Psychosocial oncology in China is a young field, yet it is emerging with guarded enthusiasm and a definite eagerness for the acquisition of knowledge and collaboration with palliative care professionals [7]. In 1995, the Beijing Cancer Hospital became the first cancer hospital in China to support the development of a Psycho-Oncology department. In 2006, the Chinese Psychosocial Oncology Society (CPOS) was established with 70 founding committee members. By now, there are more than 500 members, but the relative shortage of trained psychooncology professionals in China means that most CPOS members are oncologists and oncology nurses. Thus, the scarcity of psychooncology professionals is a problem in the palliative care area. The standard team of the National Hospice Service Program (NHSP) includes at least 2 physicians, 2 nurses, 1 social worker, 1 driver, and 1 clerk with a designated car. A psycho-oncology professional is not necessarily a member of this team. In the future, since the main aim of CPOS is “Integration of Psychosocial Care in Routine Cancer Care”, which includes palliative care service, psycho-oncology professionals will play a more important role in palliative care.
National Hospice Service Program (NHSP) funded by Li Ka Shing Foundation
The Li Ka Shing Foundation funded the first Affiliated Hospital of Shantou University Medical College and established the first Hospice Unit in mainland China in 1998. A “Heart of Gold” National Hospice Service Program was launched in 2001, offering impoverished terminally ill patients free home-based pain-relief medications, nursing care, bereavement support and psychological counseling, amongst its other services. As one of the Foundation’s long-term projects to date, the Program manages more than 30 Hospice Units across 26 provinces, autonomous regions and municipalities in mainland China. It is a nationwide holistic medical charity program which provides not only pain-relief medications, but also psychological, bereavement and social support, benefiting over 160,000 patients through more than two million service sessions (home visits 391,541, out-patient visits 1,211,809, phone call consultations 633,326). The objectives and principles of NHSP include:
• To improve the quality of life for patients and relatives.
• To provide “five domains of care”: whole person, whole family, whole course of illness, whole team, and whole community.
• To serve patients in poverty with advanced cancer at home without regard to payment
• To provide relief from pain and other distressing symptoms.
• To provide psychosocial, emotional, and spiritual assistance to the patients and their families.
• To develop education and training in palliative care for society [8].
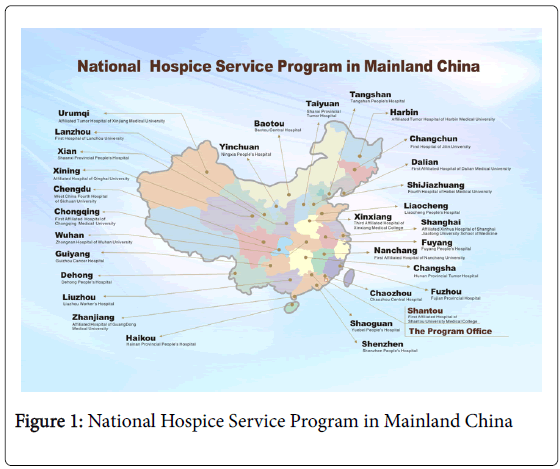
While palliative care has become a standard and integrated healthcare practice in many Western countries, it is still undeveloped in mainland China and has a short history. The first research center for palliative care was established in Tianjin Medical University in 1988, which marks the origin of this specialty in mainland China [9]. In 1998, the first Hospice in mainland China was set up in Shantou with the support of the Li Ka-shing Foundation. As of the end of 2016, there are 37 Hospice Units established throughout China, located in 31 cities in 26 provinces in mainland China (Figure 1), covering over 350 districts and counties. Over the past 28 years, not only did the hospices help many patients avoid pain and distress, they also heightened the knowledge of the Chinese public regarding palliative care in late-stage cancer patients. Nevertheless, so far the services provided by hospices are mainly homecare, which is inadequate for many patients, as some symptoms, such as pleural effusion, ascites and bleeding cannot be addressed at home. In recent years, several tertiary hospitals began to build palliative care wards or palliative care centers. Thus, we hope that a seamless model of palliative care with the collaboration of both hospital care and homecare can be developed in mainland China.
The estimated 4.292 million new cancer cases and 2.814 million cancer deaths in mainland China in 2015 revealed that around 80% of these fatalities were diagnosed as advanced disease [1]. Thus, there is an urgent need for palliative care in mainland China. However, there are significant barriers [10] to developing and implementing palliative care service in mainland China. First of all, cultural perception and misunderstanding of palliative care to “caring for a person approaching death” is unacceptable in Chinese public [11]. Further, people feel the withdrawal of all anticancer treatments means being abandoned by the doctors [12]. Secondly, the lack of professionally trained health-care providers and administrators is another major barrier. A survey among interns in a Chinese Medical University (N=400) [13] showed that less than 10% of the them felt competent in basic pain management, and nearly 80% did not feel adequately trained in discussing death with patients and family members. Thirdly, there are several administrative and policy problems. For example, most hospitals in China must generate their own incomes, and since palliative care is not very profitable, it is usually overlooked by the hospitals and clinicians [13]. Fourthly, a shortage of funding and donations to support the development of palliative care is also a barrier in mainland China. The services of oncologists are highly valued, while little value is placed on hospice or palliative care which are not a priority for public funding; moreover, it is viewed that funding is wasted on high-cost medications, and unnecessary and futile treatments for incurable conditions [14].
Palliative care needs a multidisciplinary team including oncologists, psychiatrists, psychologists, nurses and social workers. Yet psychooncology also plays an important role in palliative care, especially in early palliative care. When a patient is newly diagnosed with advanced cancer without many severe somatic symptoms, most of their distress at that time is psychosocial. Psychosocial care can help patients and their family cope better with the disease and treatments, communicate better with their medical care team, and ease their emotional distress. Yet psycho-oncology professionals are very limited in mainland China. Although in the past few years, with the help of the Chinese Psychosocial Oncology Society (CPOS), some provincial cancer hospitals have built Psycho-Oncology Departments and have begun to provide some psychosocial care for patients, the service capabilities of these departments are still insufficient due to lack of staff and financial support. As a result, the psychosocial service in urban areas of China is insufficient, let alone in more remote areas. Thus, the development of psycho-oncology is a critical task in the development of palliative care in mainland China.
Doctor-patient communication is another difficult task in implementing palliative care in mainland China. Families ask the doctors to withhold the bad news from patients in order to protect them, which is still a common phenomenon. Some patients have unrealistic expectations of curing their disease and insist on having aggressive treatments even at very late stages. Actually, the decision of palliative care should be made earlier, and good communication is the key approach to this vital decision-making. Doctor-patient communication training for palliative care professionals should be emphasized in the future.
The 2015 Quality of Death Index [15] shows that China ranked 71st of 80 countries, and was reported to be “facing difficulties from slow adoption of palliative care and a rapidly aging population”. More efforts should be made in clinical practice, education and research to develop and implement palliative care in mainland China.
References
- WHO (2002) National cancer control programmes: Policies and managerial guidelines. Geneva, World Health Organization.
- (2016) Infoplease, World’s 50 most populous countries.
- Chen W, Zheng R, Baade PD, Zhang S, Zeng H, et al. (2016) Cancer statistics in China, 2015. CA Cancer J Clin 66: 115-132.
- Li J, Davis MP, Gamier P (2011) Palliative medicine: Barriers and developments in mainland China. Curr Oncol Rep 13: 290-294.
- Huang QS (2015) A review on problems of China's hospice care and analysis of possible solutions. Chin Med J 128: 279-281.
- Wu Y, Li L, Su H, Yao X, Wen M (2016) Hospice and palliative care: Development and challenges in China. Clin J Oncol Nurs 20: 16-19.
- Tang L, Janet DG, Barry DB (2009) Psychosocial oncology in China - challenges and opportunities. Chinese-German J Clin Oncol 123-128.
- National hospice service program by LKSF (2011) Guidelines for hospice management.
- Wu Y, Li L, Su H, Yao X, Wen M (2016) Hospice and palliative care: Development and challenges in China. Clin J Oncol Nurs 20: 16.
- Hu K, Feng D (2016) Barriers in palliative care in China. Lancet 387: 1272.
- Gao W (2013) Palliative care in China: Current status and future directions. J Palliat Med 02.
- Li X, Xing YF, Chen ZH, Dong M, Wu XY (2013) Palliative care in urban areas of China. Lancet Oncol 14: 339.
- Jiang X, Liao Z, Hao J, Guo Y, Zhou Y, et al. (2011) Palliative care education in China: Insight into one medical university. J Pain Symptom Manage 41: 796-800.
- Zou M, O'Connor M, Peters L, Jiejun W (2013) Palliative Care in Mainland China. Asia Pac J Health Management 8.
- The Economist Intelligence Unit. Quality of death index 2015, ranking palliative care across the world.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 4351
- [From(publication date):
May-2017 - Apr 11, 2025] - Breakdown by view type
- HTML page views : 3405
- PDF downloads : 946