Research Article Open Access
Overweight-Obesity Prevalence in Children of North-West Italy: Efficacy of Counselling
Renata Colombo1, Elisabetta Scurati-Manzoni2*, Domenico Careddu3 and Andrea Guala2
1Azienda Sanitaria Locale, Vercelli, Regione Piemonte, Italy
2Struttura Operativa Complessa di Pediatria, Ospedale Castelli, Verbania, Italy
3Azienda Sanitaria Locale, Novara, Regione Piemonte, Italy
- *Corresponding Author:
- Elisabetta Scurati-Manzoni
Struttura Operativa Complessa di Pediatria
Ospedale Castelli; Verbania, Italy
Tel: 00393208010886
E-mail: lisa.scurati@libero.it
Received date: August 14, 2015 Accepted date: September 02, 2015 Published date: September 10, 2015
Citation: Colombo R, Scurati-Manzoni E, Careddu D, Guala A (2015) Overweight-Obesity Prevalence in Children of North-West Italy: Efficacy of Counseling. J Gastrointest Dig Syst 5:337. doi:10.4172/2161-069X.1000337
Copyright: © 2015 Colombo R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: The increased incidence of obesity and overweight, among adults and children, is the most alarming “epidemic” of this decade. The Italian annual survey “Okkio alla Salute – Promozione della salute e della crescita sana dei bambini della scuola primaria”, showed, in 2009, that overweight and obesity affect 32.8% of Italian children. After considering these results, 16 family pediatricians of the province of Vercelli, from January 2010 on carried out a survey in order to assess pediatric obesity prevalence in their province. Methods: During children’s routine medical checks, age ranges 3-4, 5-6 and 8-9, anthropometric parameters were collected. From 2011 counselling about exercise, diet and healthy lifestyle was offered as well. Results: The graphs show that the drops in prevalence of obese and overweight patients, between 2010 and 2013, are statistically significant among age ranges 3-4 and 5-6 (especially among the 3-4 age group), but statistically not significant among the age range 8-9. Conclusions: Family pediatricians have the resources to prevent and treat overweight and obesity, involving the family and children in target interventions with effectiveness, as also published data evidence, and referring only most critical cases to second level nutrition advisory service. Yet, it is very important to start offering the parents counselling, since the first days of children’s life, as the older the children are, the more difficult it is for them to modify diet habits and lifestyle.
Keywords
Overweight; Obesity; Waist size/height ratio; Counselling; Family pediatricians
Abbreviations
W.H.O: World Health Organization; C.N.E.S.P.S: Centro Nazionale di Epidemiologia Sorveglianza e Promozione Della Salute; I.S.S: Istituto Superiore Della Sanità; A.S.L: Azienda Sanitaria Locale
Introduction
The increased incidence of obesity and overweight, both among adults and children, is the most alarming “epidemic” of this decade. Because of the known health damages and consequent financial investments, the W.H.O. and (in Italy) the Ministero della Salute Italiano have identified obesity prevention as an overriding goal, in the public health domain. Moreover, Italian data emerging from the annual epidemiological survey “Okkio alla Salute – Promozione della salute e della crescita sana dei bambini della scuola primaria” [1] (a survey carried out every year by the Centro Nazionale di Epidemiologia Sorveglianza e Promozione della Salute (C.N.E.S.P.S) of the Istituto Superiore della Sanità (I.S.S)) and related to both the European program “Guadagnare salute” and the National Prevention Plan) are relevant. These data (obtained by monitoring every year, throughout the country, a significant sample of 8 to 9 years old children, attending Italian schools) showed, in 2009, that overweight and obesity globally affect 32.8% of Italian children, besides highlighting that children’s obesity and overweight depend largely on nutritional and behavioral mistakes (i.e. skipping breakfast, shortage of fruit and vegetables, lack of physical activity, indoor technological playing) and are in inverse proportion to parent’s schooling and directly proportional to their weight [2]. After considering the results of that survey and the importance and cost/benefit results of school prevention programs [3,4] family pediatricians belonging to the Azienda Sanitaria Locale (A.S.L., i.e. the Local Health Authority) of Vercelli (Piedmont, Italy) and responsible for the health of the whole pediatric population up to 14 years in the province of Vercelli, from January 2010 on, planned and carried out an epidemiological study in order to assess the prevalence of obesity and to monitor and address specifically this issue in their area. Since 2010, during children’s programmed-routine medical check, age ranges 3-4, 5-6, and 8-9, anthropometric parameters were collected, organized in files and then stored on a classified server. Subsequently from 2011 on, during the routine medical checks, counselling about diet, exercise and healthy life-style was given, the outcome of which was assessed with a questionnaire; the resulting data were registered and collected as well. Analysis of all the data that have been collected during the first four years of this survey, carried out in the province of Vercelli, allowed us to assess and monitor the pediatric population’s overweight and obesity prevalence in this area, to evaluate the effectiveness of family pediatricians’ intervention in obesity prevention and care and to address the issues that emerged along with the intervention itself.
Methods
Since January 2010, during children’s programmed-routine medical checks, age ranges 3-4, 5-6, and 8-9, all the 16 family pediatricians of the province of Vercelliinvolved in this survey, started collecting anamnestic data about breast-feeding, suckling, diet, accidents, parents’ smoking and nutritional habits and family chronic diseases, along with the anthropometric parameters. The evaluated pediatric population is representative of the pediatric population of Piedmont.
Weight and height were clinically evaluated by the pediatricians them-selves and plotted on WHO age related weight and height charts; weight didn’t include clothing or shoes, height was assessed not in shoes. The Body Mass Index (BMI) was calculated according to Cole’s rule (BMI: weight in Kg/height in m2) and plotted on WHO 2006 and 2007 age related BMI charts [5].
According to the WHO definitions, overweight was defined as Body Mass Index (BMI) >2 standard deviations above the WHO growth standard median; whereas obesity was defined as Body Mass Index (BMI) >3 standard deviations above the WHO growth standard median.
During the fourth year of the survey (2013), after specific training of all pediatricians, the waist circumference measure was introduced and the waist-to-height ratio was calculated in both overweight and obese subjects. The waist circumference was measured at the end of a normal expiration, with a folding ruler placed in the middle between the iliac crest and the costal arch. These last parameters, according to the most recent literature data [6-8], allow a more reliable quantification and stratification of both cardiovascular risk and metabolic syndrome [9-12]. Because it is internationally admitted that cut-offs must be specific for each population [13], a waist-height ratio cut-off equal to or higher than 0.50 for overweight children and 0.60 for obese children [14,15] was decided, in agreement with the literature specific for the Italian population. Yet, the waist/height ratio assessment was narrowed to the 5-6 and 8-9 age ranges, as we found that this measurement was not connected with the BMI in the 3-4 age range children [16]. Since 2011 (the second year of the project), in order to improve their intervention in obesity prevention, all the 16 pediatricians (after more specific training, managed by external consultants) introduced counseling about exercise, diet and healthy lifestyle. Counseling was given, during the medical check-up, together with an informative pamphlet, which was offered to all the parents and to the older children. The counseling outcome was assessed with a questionnaire, which evaluated positive changes in lifestyle and diet habits, achieved level of exercise, outdoor playing, level of satisfaction, emerging difficulties and issues: these data were registered and added to the ones already collected. Follow-up assessment was offered to all overweight subjects every two months, whereas the most critical obese patients were sent to a second level nutrition advisory service.
Just because there has been an increasing focus on obesity prevention at earlier stages of life course [4], in this survey data on the BMI of 24-30 months old patients were collected as well. Thanks to a sophisticated software (Pediabit) provided by the Azienda Sanitaria Locale (A.S.L., i.e. the Local Health Authority) of Vercelli, all the family pediatricians were able to organize in files all the collected data, which were hence available on- line. Finally, all the data were stored by the administration of the Azienda Sanitaria Locale (A.S.L., i.e. the Local Health Authority) of Vercelli, in a classified server. The prevalence trends of obesity, overweight and overweight-obesity were calculated for each year separately, using a two by two contingent table; subsequently prevalence of obesity, overweight and overweight-obesity between years 2010 and 2013 were compared using the chi-square test for clustered data. Differences were considered significant at p<0.05.
Results
Tables 1-3 show absolute numbers of obese, overweight and obeseoverweight children versus all the examined children.
| 2010 Examined children | 2010 Obese children | 2011 Examined children | 2011 Obese children | 2012 Examined children | 2012 Obese children | 2013 Examined children | 2013 Obese children | |
|---|---|---|---|---|---|---|---|---|
| 3-4 years | 400 (M220; 55%) | 25 (M15; 60%) | 749 (M351; 46.9%) | 27 (M14; 51.9) | 1023 (M497;48.6%) | 36 (M18;50%) | 940 (M516; 54.9%) | 23 (M13; 56.5%) |
| 5-6 years | 300 (M142; 47.3%) | 31 (M19; 61.3%) | 640 (M314;49%) | 45 (M24; 53.3%) | 888 (M450; 50.7%) | 43 (M20; 46.5%) | 839 (M399; 47.5%) | 39 (M23; 59%) |
| 8-9 years | 220 (M103; 46.8%) | 25 (M12; 48%) | 387 (M199; 51.4%) | 43 (M19; 44.2%) | 629 (M303; 48.2%) | 58 (M27; 46.5%) | 540 (M265; 49%) | 42 (M11; 26.2%) |
Table 1: Obese children versus examined children years 2010-2013 (absolute numbers, total males’ percentages and obese males’ percentages).
| 2010 Examined children | 2010 Overweight children | 2011 Examined children | 2011 Overweight children | 2012 Examined children | 2012 Overweight children | 2013 Examined children | 2013 Overweight children | |
|---|---|---|---|---|---|---|---|---|
| 3-4 years | 400(M220; 55%) | 53 (M21; 39.6%) | 749 (M351; 46.9%) | 88 (M45; 51.1%) | 1023 (M497;48.6%) | 96 (M50; 52%) | 940 | 65 (M35; 53.8%) |
| 5-6 years | 300 (M142; 47.3%) | 57 (M30; 52.6%) | 640 (M314;49%) | 99 (M46) | 888 (M450; 50.7%) | 121 (M66 54.5%) | 839 | 100 (M53; 53%) |
| 8-9 years | 220 (M103; 46.8%) | 58 M(26; 44.8%) | 387 (M199; 51.4%) | 103 (M57) | 629 (M303; 48.2%) | 129 (M65; 50.4%) | 540 | 111 (M60; 54%) |
Table 2: Overweight children versus examined children years 2010-2013 (absolute numbers, total males’ percentages and overweight males’ percentages).
| 2010 Examined children | 2010 Obese-overweight children | 2011 Examined children | 2011 Obese-overweight children | 2012 Examined children | 2012 Obese-overweight children | 2013 Examined children | 2013Obese-overweight children | |
|---|---|---|---|---|---|---|---|---|
| 3-4 years | 400(M220; 55%) | 78 (M36; 46.1%)) | 749 (M351; 46.9%) | 115 (M59; 51.3%) | 1023 (M497;48.6%) | 132 (M68) | 940 | 88 (M48) |
| 5-6 years | 300 (M142; 47.3%) | 88 (M49) | 640 (M314;49%) | 144 (M70; 48.6%) | 888 (M450; 50.7%) | 164 (M86) | 839 | 139 (M76) |
| 8-9 years | 220 (M103; 46.8%) | 83 (M38) | 387 (M199; 51.4%) | 146 (M76; 52%) | 629 (M303; 48.2%) | 187 (M92; 49.2%) | 540 | 153 (M71; 46.4%) |
Table 3: Obese-overweight children versus examined children years 2010-2013 (absolute numbers, total males’ percentages and obese-overweight males’ percentages).
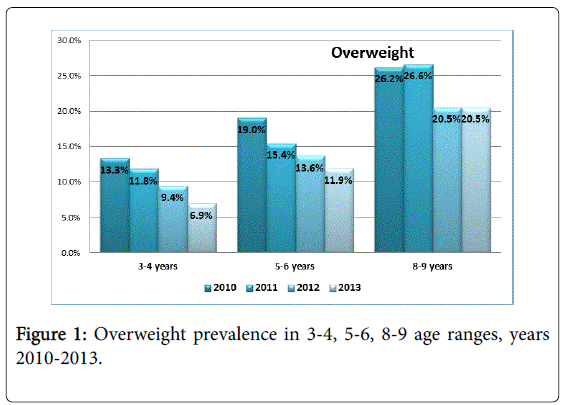
Figure 1 shows the overweight prevalence of the three age groups examined, in the years 2010-2011-2012-2013.In the 3-4 years range, the drop by 6.4%, between 2010 and 2013, is statistically significant (p 0.0003495). Similarly in the 5-6 years range, the drop by 7.1%, between 2010 and 2013, is statistically significant (p 0.004388).
In the 8-9 years range, instead, between 2010 and 2011 there is a slight increase (0.4%) in overweight prevalence; subsequently there is a decrease, in 2012, by 6.1%, which then remained stable in 2013. Yet the total drop by 5.7%, between 2010 and 2013, is not statistically significant (p 0.1010).
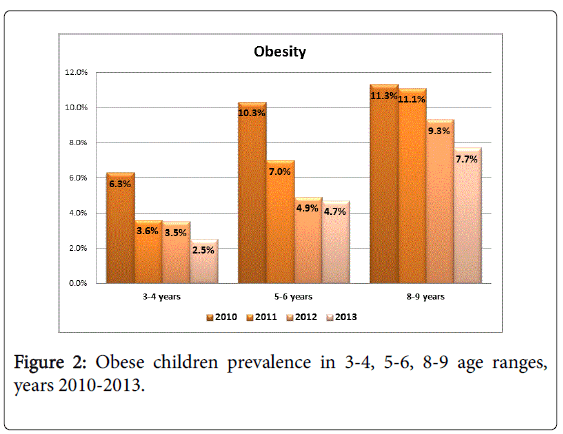
Figure 2 shows the obesity prevalence of the three age groups examined, in the years 2010-2011-2012-2013.In the 3-4 years range, the drop by 3.8%, between 2010 and 2013, is statistically significant (p 0.0005125) Similarly in the 5-6 years range, the drop by 5.6%, between 2010 and 2013, is statistically significant (p 0.0005006).
In the 8-9 years range, instead, the drop by 3.6%, between 2010 and 2013, is statistically not significant (p 0.07531).
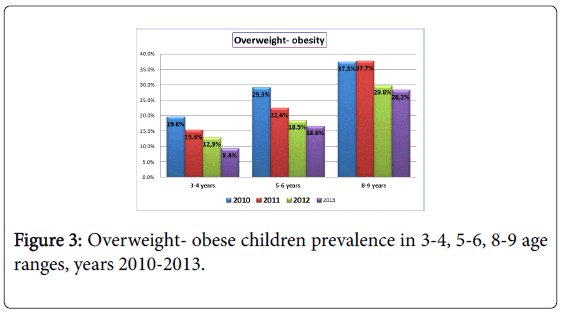
Figure 3 shows the overweight-obesity prevalence of the three age groups examined, in the years 2010-2011-2012-2013.
In the 3-4 years range, between 2010 and 2013, there is a global drop by 10.2% that is statistically significant (p 0.000003829).
Similarly in the 5-6 years range, there is a global drop by 12.7%, between 2010 and 2013, which is statistically significant (p 0.00007489).
Finally in the 8-9 years range, the global drop by 9.3%, between 2010 and 2013, is statistically not significant (p 0.04158).
Surprisingly, sixty nine children with normal BMI (especially in the 5-6 age range) had a waist/height ratio higher than 0,5.The data about the counselling outcome were organized in files, which amounted to 1776 in 2011, 2540 in 2012 and 2319 in 2013.
The total drop-out of all the children in the age ranges 3-4 and 5-6, was relatively low (144 children=8-9%). The collected data of the 8-9 years range, instead, represent only about half of the resident children, who (according to Italian regulations) passed over to family GPs’ care not involved in this survey.
Among the included 24-30 months old patients, even if comparatively few (i.e. 393 children), we calculated a 6% prevalence of obese-overweight children (i.e. 23 children); these data are graphically represented within the 3-4 age group.
The total number of overweight-obese children (calculated in four years survey), at high risk of metabolic and cardiovascular diseases amounts to 101 (i.e. 34.47% of overweight-obese children): 85 obese (40.28%) and 16 overweight (19.5%), equally distributed among the 5-6 and 8-9 age ranges. This means that more than one third of the children are therefore at high risk of these diseases.
Discussion
Both graphs of obese and overweight subjects show, from 2010 to 2013, a considerable overall decline in the prevalence, which can be attributed to the effectiveness of the action aimed at improving diet habits, lifestyle and exercise. The results relating to the 3-4 age range, are very significant: we registered an important statistically significant decline of both overweight and obese subjects in the subsequent years (obesity prevalence decrease from 6.3% in 2010 to 2.5% in 2013, overweight prevalence decrease from 13.3% in 2010 to 6.9% in 2013).
These successful resultsmust be attributed to the pediatricians’ early intervention with counselling, since the first days of children’s life, on diet (breast milk, age of weaning, caloric intake control, lower protein intake), exercise in infancy and healthy lifestyle. Besides, it is likely that these children, whose parents received the counselling since the very beginning, will provide more satisfactory results when evaluated at 5-6 years of age. In the 5-6 age range, we can certainly see the efficacy of the pediatricians’ counselling on diet (regular meals, caloric intake control, increase in fruit and vegetables consumption), regular exercise and healthy lifestyle, in both obese and overweight subjects. Yet, there is very little reduction of the prevalence of obese subjects between 2012 and 2013, which means that not all subjects responded to the counselling: we presume that this could be due to the genetic origin of the obesity, which affect some of the subjects, but mainly to our late and only partially efficacious intervention in changing established western lifestyles, as also other data published in literature confirm [15,17].
In the 8-9 years range (whose prevalence of the overweight was the same for two years running, i.e. 2012-2013), we can notice a partial efficacy of the pediatricians’ intervention on both obese and overweight children. Yet, our very late intervention on well-established and unchangeable wrong lifestyles was even more, only to a small extent effective; besides genetically determined obesity, the same as for the 5-6 years group, had also its influence on the outcome. Moreover, there certainly was a loss of a certain number of 8-9 years old children, who were no longer followed by the family pediatricians, but by adults’ GPs of the province of Vercelli, who were not involved in this survey.
According to the National Italian Health System children from 8 years on, can be followed by GP for adults, which not always have enough competence in addressing pediatric health issues. Hence obese and overweight children of the 8-9 years range, were probably more than the amount estimated in our survey. This shows how important it is to detect the problem early, to intervene as soon as possible and to follow the obese subjects as long as possible, as the older the children are, the more difficult it is for them to modify their diet habits and lifestyle: this project started four years ago, when unfortunately most of the children included in our survey were not in the younger age range.
According to recent data, 60% percent of children who are overweight at any time during the preschool period and 80% of children who are overweight at any time during the elementary school, will also be overweight at 12 years old [18]. Moreover, the latest literature on this subject points out the challenge in addressing the childhood obesity epidemic [19] and stresses the importance of early prevention and treatment, in order to reduce the costs of the chronic diseases in adult age, i.e. cardiovascular diseases, type 2 diabetes, high blood pressure [20-23]. The analysis of our survey highlights, on one end overall encouraging results, on the other end the concerning data of more than one third of the examined children (i.e. 101 out of all the examined subjects) being already at high risk of metabolic syndrome and cardiovascular disease, besides nonalcoholic fatty liver disease, which is associated with the metabolic syndrome and in the pathophysiology of which, insulin resistance plays a main role [19,24-26].
Hence it is paramount to continue improving both these counselling and survey and to go on watching out very carefully also for overweight and obese children with low socio-cultural level parents [27], who do respond to offered counselling, as demonstrated also in recent literature [17].
Our near future programs foresee the introduction of a set of tests for more critical patients, in order to identify even more closely those candidates for second level nutrition advisory service. These tests include blood levels of cholesterol and triglycerides, glucose tolerance testing and hepatic ultrasonography, the latter in order to discover a possible hepatic steatosis [19,24-26]. Besides we intend to offer personalized nutrition consultancy, with the help of a dietitian consultant, working together with family pediatricians.
Conclusions
We conclude that family pediatricians have the skills and the resources to prevent and treat both overweight and childhood obesity, involving the family and children in target interventions with effectiveness, as also published data evidence [23], and referring only most critical cases to second level nutrition advisory service.
The sooner the intervention the better, as the older the children are, the more difficult it is for them to modify their well-established diet habits and lifestyles. Hence it is paramount for family pediatricians to start early offering the parents counselling, since the first days of children’s life, on diet (breast milk, age of weaning, caloric intake control, lower protein intake), exercise in infancy and healthy lifestyle.
Acknowledgement
Here are the members of this survey: Livio Barberis, Gianna Calderini, Daniela Campra, Lucrezio Coscarelli, Loredano Guaraglia, Maria Cristina Mirabelli, Monica Gaggero, Elisa Montanari, Piercarlo Michelone, Gaetano Musco, Antonella Pezzera, Sandro Provera, Maura Rossi, Sandro Sandri, Marcello Trada, all family pediatricians of A.S.L .of Vercelli, Piedmont, Italy.
References
- Bastien M, Poirier P, Lemieux I, Després JP (2014) Overview of epidemiology and contribution of obesity to cardiovascular disease. ProgCardiovasc Dis 56: 369-381.
- Browning LM, Hsieh SD, Ashwell M (2010) A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev 23: 247-269.
- Campagnolo PD, Hoffman DJ, Vitolo MR (2011) Waist-to-height ratio as a screening tool for children with risk factors for cardiovascular disease. Ann Hum Biol 38: 265-270.
- Lumeng JC, Taveras EM, Birch L, Yanovski SZ (2015) Prevention of obesity in infancy and early childhood: a National Institutes of Health workshop. JAMA Pediatr 169: 484-490.
- Centers for Disease Control and Prevention (CDC) (2013) Vital signs: obesity among low-income, preschool-aged children--United States, 2008-2011. MMWR Morb Mortal Wkly Rep 62: 629-634.
- Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320: 1240-1243.
- Cunningham SA, Kramer MR, Narayan KM (2014) Incidence of childhood obesity in the United States. N Engl J Med 370: 403-411.
- Danielsson P, Kowalski J, Ekblom Ö, Marcus C (2012) Response of severely obese children and adolescents to behavioral treatment. Arch PediatrAdolesc Med 166: 1103-1108.
- de Mutsert R, Sun Q, Willett WC, Hu FB, van Dam RM (2014) Overweight in early adulthood, adult weight change, and risk of type 2 diabetes, cardiovascular diseases, and certain cancers in men: a cohort study. Am J Epidemiol 179: 1353-1365.
- Graves L, Garnett SP, Cowell CT, Baur LA, Ness A, et al. (2014) Waist-to-height ratio and cardiometabolic risk factors in adolescence: findings from a prospective birth cohort. PediatrObes 9: 327-338.
- Griffiths C, Gately P, Marchant PR, Cooke CB (2013) A five year longitudinal study investigating the prevalence of childhood obesity: comparison of BMI and waist circumference. Public Health 127: 1090-1096.
- Keefer DJ, Caputo JL, Tseh W (2013) Waist-to-height ratio and body mass index as indicators of cardiovascular risk in youth. J Sch Health 83: 805-809.
- Kelsey MM, Zaepfel A, Bjornstad P, Nadeau KJ (2014) Age-related consequences of childhood obesity. Gerontology 60: 222-228.
- Kesztyüs D, Schreiber A, Wirt T, Wiedom M, Dreyhaupt J, et al. (2013) Economic evaluation of URMEL-ICE, a school-based overweight prevention programme comprising metabolism, exercise and lifestyle intervention in children. Eur J Health Econ 14: 185-195.
- Kuba VM, Leone C, Damiani D (2013) Is waist-to-height ratio a useful indicator of cardio-metabolic risk in 6-10-year-old children? BMC Pediatr 13: 91.
- Lehto R, Ray C, Lahti-Koski M, Roos E (2011) Health behaviors, waist circumference and waist-to-height ratio in children. Eur J ClinNutr 65: 841-848.
- Maffeis C, Banzato C, Talamini G; Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology (2008) Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr 152: 207-213.
- Marzuillo P, Del Giudice EM, Santoro N (2014) Pediatric non-alcoholic fatty liver disease: New insights and future directions. World J Hepatol 6: 217-225.
- Morandi A, Maffeis C (2014) Predictors of metabolic risk in childhood obesity. Horm Res Paediatr 82: 3-11.
- Turner AJ, Hick PE (1975) Inhibition of aldehyde reductase by acidic metabolites of the biogenic amines. BiochemPharmacol 24: 1731-1733.
- Nader PR, O'Brien M, Houts R, Bradley R, Belsky J, et al. (2006) Identifying risk for obesity in early childhood. Pediatrics 118: e594-601.
- Nambiar S, Hughes I, Davies PS (2010) Developing waist-to-height ratio cut-offs to define overweight and obesity in children and adolescents. Public Health Nutr 13: 1566-1574.
- Quattrin T, Roemmich JN, Paluch R, Yu J, Epstein LH, et al. (2014) Treatment outcomes of overweight children and parents in the medical home. Pediatrics 134: 290-297.
- Santoro N, Amato A, Grandone A, Brienza C, Savarese P, et al. (2013) Predicting metabolic syndrome in obese children and adolescents: look, measure and ask. Obes Facts 6: 48-56.
- Savva SC, Lamnisos D, Kafatos AG (2013) Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes MetabSyndrObes 6: 403-419.
- Sijtsma A, Bocca G, L'abée C, Liem ET, Sauer PJ, et al. (2014) Waist-to-height ratio, waist circumference and BMI as indicators of percentage fat mass and cardiometabolic risk factors in children aged 3-7 years. ClinNutr 33: 311-315.
- Zhang HX, Xu XQ, Fu JF, Lai C, Chen XF (2015) Predicting hepatic steatosis and liver fat content in obese children based on biochemical parameters and anthropometry. PediatrObes 10: 112-117.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13882
- [From(publication date):
October-2015 - Apr 05, 2025] - Breakdown by view type
- HTML page views : 9386
- PDF downloads : 4496