Overview: Epidemiology, Diagnostic and Therapeutic Challenges of Pediatric community acquired Pneumonia
Received: 27-Jun-2022 / Manuscript No. ECR-22-70012 / Editor assigned: 30-Jun-2022 / PreQC No. ECR-22-70012 / Reviewed: 13-Jul-2022 / QC No. ECR-22-70012 / Revised: 18-Jul-2022 / Manuscript No. ECR-22-70012 / Published Date: 25-Jul-2022 DOI: 10.4172/2161-1165.1000450
Abstract
Pediatric community-acquired pneumonia (CAP) is still one of the most prevalent and dangerous illnesses in children and it continue to cause significant morbidity. The prevalence of invasive diseases brought on by Streptococcus pneumoniae has significantly decreased as a result of routine childhood vaccination. Molecular diagnostics have made it clearer how crucial respiratory viruses are in paediatric CAP, but bacterial diagnostics are still not up to par. In-depth research is currently being done on biomarkers and the molecular host responses to infection, which may help us better, understand the causes of pneumonia and its course. A viral and bacterial infection of the lower airways is known as pneumonia. Clinical pneumonia symptoms and signs picked up outside of a hospital setting are known as "community-acquired pneumonia" (CAP). It is one of the most prevalent severe illnesses in children, and in 2015, it was responsible for over 900,000 fatalities in children under the age of five. Although the death rate from CAP is substantially lower in high-income nations than it is in the developing world, CAP nevertheless accounts for a sizable fraction of visits to the doctor and hospital stays. This review focuses on paediatric CAP in the United States and other developed countries, highlighting the evolving epidemiology of CAP, the difficulties in diagnosing and treating it, and potential research areas.
Keywords
Paediatric; Pneumothorax; Necrotizing Pneumonia
Introduction
Children who are hospitalised for hypoxemia or respiratory distress, as well as those with probable sequelae including parapneumonic effusions, necrotizing pneumonia, or pneumothorax, should have chest radiographs. Compared to chest radiography, chest ultrasound has higher sensitivity (92 percent to 98 percent) and specificity (92 percent to 100 percent) for detecting lung consolidation. Chest ultrasound is most frequently used to assess local consequences, such as parapneumonic effusion and empyema. 9–13 Chest ultra sonographies additionally has the advantages of not using ionizing radiation and being accessible in most emergency room settings. The evaluation and interpretation of ultrasonography are heavily operator dependent, which is a significant restriction [1]. Therefore, large-scale, practical investigations are required to more thoroughly assess the efficiency of this imaging technology compared to normal chest radiography, despite these encouraging early results. Numerous pathogens, such as viruses and bacteria, can cause the diverse disease pneumonia. In the past, Streptococcus pneumoniae, Haemophilus influenzae, Streptococcus pyogenes, and Staphylococcus aureus were thought to be the main causes of CAP. However, the prevalence of sickness brought on by Streptococcus pneumoniae and H influenzae has significantly decreased since routine childhood vaccination against these infections was introduced. In addition, extremely sensitive molecular tests for viral respiratory infections have increased awareness of the role that viruses play in CAP. A 2004 study by Michelow and colleagues15 is a good example of an aetiology study conducted before the PCV era [2].
Materials and Methods
The pathogens in 154 hospitalised children with radiographically confirmed lower respiratory infections at a single institution were identified using conventional culture techniques, pneumolysin-based polymerase chain reaction (PCR) assays, viral direct fluorescent antibody tests, and serologic tests for viruses, Mycoplasma spp, and Chlamydia spp. Streptococcus pneumoniae, which was found in 73 percent of the children with bacterial sickness, was the most often found infection in the majority of patients (60 percent), whereas viruses were found in 45 percent of the children. More than 2300 paediatric CAP hospitalizations in the US were the subject of the multicenter Centers for Disease Control and Prevention (CDC) Etiology of Pneumonia in the Community (EPIC) Study, which was carried out from 2010 to 2012. Eight distinct viruses were identified in this investigation using serology and nasopharyngeal PCR; usual bacteria were identified using culture-based techniques and whole-blood PCR (pneumococcal lyt-A); and atypical bacteria were identified using nasopharyngeal PCR [3]. In contrast to bacteria, which were only found in 15% of children, viruses were found in more than 70% of young ones. Respiratory syncytial virus (RSV), human rhinovirus, human metapneumovirus, and adenovirus were the most prevalent viral infections, all of which were found in more than 10% of children. Children under the age of 5 were more likely to contract RSV, adenovirus, and human metapneumovirus. Compared to older kids, 5 years old. Streptococcus pneumoniae was only found in 4% of children in the CDC EPIC survey, although bacteria were found in about 15% of kids overall, highlighting the influence PCV has had on the epidemiology of paediatric CAP. 4 The most common bacterial pathogen discovered was Mycoplasma pneumoniae, which was found in 8% of children, including 19% of school-aged children but just 3% of children under the age of 5. In 1% or fewer of the kids, other germs were discovered. Importantly, in the CDC EPIC study, 19% of the children had no infection found, underlining the ongoing need for improved diagnostics and cutting-edge pathogen detection methods [4].
Epidemiology
Mycobacterium tuberculosis, fungi, Burkholderia cepacia, Aspergillus fumigatus, and Pseudomonas aeruginosa are other pathogens that are less frequently observed in US children. These infections typically affect people who have underlying risk factors, such as immune-compromising conditions, chronic illnesses like cystic fibrosis and spinal muscular atrophy, or a history of international travel. Patients who fail to respond to therapy for more prevalent etiologic agents should also be suspected of having these infections. Blood cultures should be taken in children hospitalised with CAP, according to the 2011 PIDS/IDSA CAP guideline. Blood cultures in this situation, however, only detect a pathogen in 2 to 7 percent of CAP patients. Blood cultures are more frequently positive in kids with parapneumonic effusion [5], with rates ranging from 10% to 35%. Blood cultures are not typically advised in the outpatient context due to the low positive rates and the likelihood that the results will alter care. Blood cultures presently offer the best chance to identify typical bacterial infections in the majority of children with CAP, despite their low yield. By only using blood cultures on patients who have a higher pre-test likelihood of having a positive culture, such as those who are very unwell or have parapneumonic pneumonia, the diagnostic yield of blood cultures can be maximised.
Patients who have received antibiotics prior to specimen collection experience much reduced pathogenic organism isolation. Additionally, studies have shown that every additional milliliter of blood collected results in a higher yield of blood cultures [6]. For unexplained reasons, obtaining sufficient weight-based blood volumes is also linked to lower contamination rates in blood cultures. Following the right sterile collection procedures will also help to reduce contamination rates. Every time pleural fluid is taken, pleural fluid cultures should be carried out because they are positive in up to 35% of cases. But other than when required for clinical care, it is impractical to obtain pleural fluid specimens due to the intrusive techniques connected with sampling the pleural space. Except in cases of failure to respond to medication, extremely severe pneumonia, or immunocompromised hosts in whom opportunistic microorganisms are suspected, bronchoalveolar lavage is infrequently needed in CAP. Due to the inability of the majority of young children with pneumonia to produce an acceptable sputum sample, sputum cultures have a low diagnostic yield in children. Antibiotic pretreatment reduces diagnostic yield even further. The possibility of gathering sputum samples from young infants using induced sputum has been investigated, however its usefulness is constrained In children with pneumonia, upper respiratory tract bacteria are frequently found, and pathogen recovery rates are comparable to those of children who do not have pneumonia [7-10].
Diagnosis
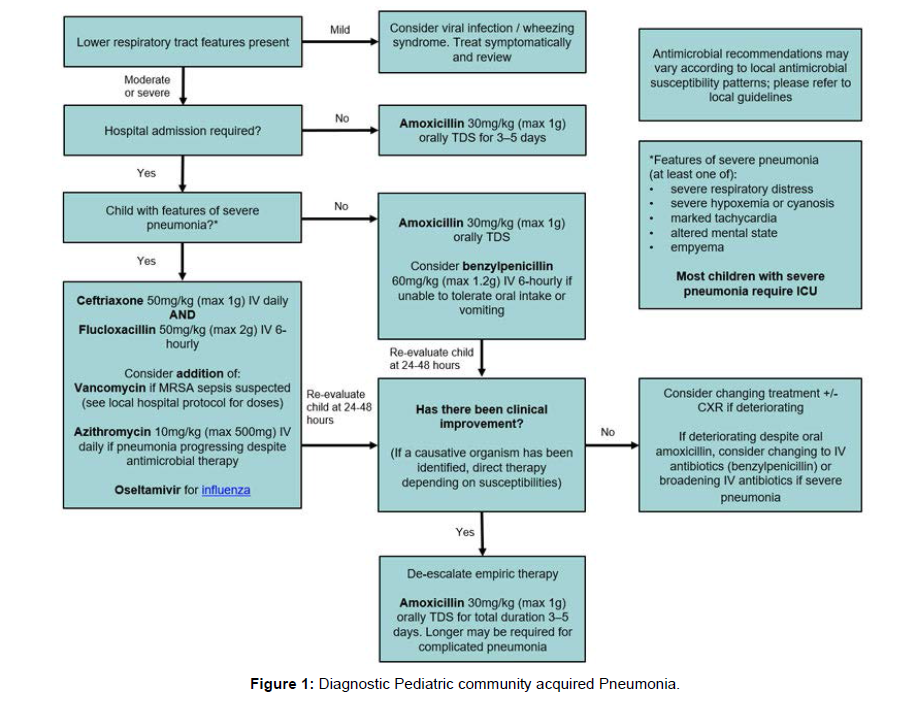
Adult patients with pneumonia are frequently evaluated with pneumococcal urine antigen testing. However, due to high rates of nasopharyngeal colonisation in children, the detection of Streptococcus pneumoniae urine antigen is linked to false-positive results. More recently, a serotype-specific urine antigen detection technique for people with pneumonia has been created and validated. It is yet to be seen if this test would be beneficial for children. Wholeblood pneumococcal PCR (lyt-A) has been utilised in epidemiologic research, such as EPIC and Pneumonia Etiology Research for Child Health, while not being frequently employed in clinical settings (PERCH). When compared to culture-based approaches, advantages could include increased sensitivity, quick turnaround times, and reduced impact from antibiotic pretreatment [Figure 1].
Streptococcus pneumoniae PCR results for 2.5 percent of the children examined in the EPIC research were positive. Only 1% of children had pneumococcus in their blood cultures, however. In the PERCH trial, only 44 children (denominator not given) had a positive blood culture for Streptococcus pneumoniae, compared to 291 children with pneumonia who were pneumococcal PCR-positive. Furthermore, the PERCH investigation found pneumococcal DNA in the blood of 273 control children despite earlier research showing 100% specificity of lyt-A pneumococcal PCR from blood50 (5.5 percent). As a result, interpretation is hampered by subpar test specificity even though pneumococcal PCR may boost detection rates over blood cultures [8].Discussion
Despite recent developments, CAP still has a high morbidity and fatality rate and is difficult to diagnose and treat. The introduction of molecular diagnostics has highlighted the critical role that respiratory viruses play in disease pathogenesis while also posing new challenges [9]. Vaccination against Haemophilus influenzae type b and Streptococcus pneumoniae has significantly decreased the rates of invasive disease caused by these pathogens. This new information raises the question of whether antibiotic medication would be beneficial for all CAP patients and, if so, which treatments could be most efficient. However, limitations of the available diagnostics prevent progress in answering these crucial concerns. Current research is focused on biomarkers and host responses to infection, which may help us better understand the causes of pneumonia and its effects. Future epidemiologic investigations utilising cutting-edge diagnostics will continue to play a crucial role in advancing knowledge of the evolving epidemiology of CAP as this significant study moves forward. The national guideline has had a conflicting impact on prescription thus far. Approximately 4 years following the publication of the guidelines, 48 tertiary care children's hospitals in the United States saw a rise in penicillin use of about 27.6% and a drop in cephalosporin use of about 27.8%, however there was significant variation amongst the hospitals.
Conclusion
In the outpatient context, same variability still exists. Local clinical practise guidelines, quality improvement techniques, and antimicrobial stewardship programmes all contribute significantly to spreading knowledge of these suggestions and minimising unnecessary and inappropriate antibiotic use. Although two significant paediatric randomised controlled studies, the Community-Acquired Pneumonia Study (CAP-IT) in the United Kingdom and the Community-Acquired Pneumonia Study (CAP-IT) in the United States, are currently evaluating the safety and efficacy of shorter courses of antibiotics, current practises for treating uncomplicated CAP typically use 7- to 10-day antibiotic courses.
Acknowledgement
None
Conflict of Interest
None
References
- Blasi F, Mantero M, Santus P, Tarsia P (2012) Understanding the burden of pneumococcal disease in adults. Clin Microbiol Infect 18 Suppl 5:7-14.
- Wiesenberger C (2010) An update of Streptococcus pneumoniae: from genomic to clinic. Med Mal Infect 40(10):605-609.
- McCracken GH Jr (2000) Diagnosis and management of pneumonia in children. Pediatr Infect Dis J 19(9):924-928.
- Ferreira-Coimbra J, Sarda C, Rello J (2020) Burden of Community-Acquired Pneumonia and Unmet Clinical Needs. Adv Ther 37(4):1302-1318.
- Tan TQ (2002) Update on pneumococcal infections of the respiratory tract. Semin Respir Infect 17(1):3-9.
- Hernandez-Garcia M, Girona-Alarcon M, Bobillo-Perez S, Urrea-Ayala M, Sole-Ribalta A, et al (2022) Ventilator-associated pneumonia is linked to a worse prognosis than community-acquired pneumonia in children. PLoS One 17(7):e0271450
- Roh EJ, Lee MH, Lee JY, Kim HB, Ahn YM, et al (2022) Analysis of national surveillance of respiratory pathogens for community-acquired pneumonia in children and adolescents. BMC Infect Dis 22(1):3-30.
- Xin KZ, Li D, Yi PH (2022) Limited generalizability of deep learning algorithm for pediatric pneumonia classification on external data. Emerg Radiol 29(1):107-113.
- Wang T, Xu Q, Dai G, Hong Y, Chen Z, et al (2021) Clinical characteristics of children with airway malacia complicated by pneumonia. BMC Infect Dis 21(1):902.
- Esposito S, Carrothers TJ, Riccobene T, Stone GG, Kantecki M (2021) Ceftaroline Fosamil for Treatment of Pediatric Complicated Skin and Soft Tissue Infections and Community-Acquired Pneumonia. Paediatr Drugs 23(6):549-563.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Britton P (2022) Overview: Epidemiology, Diagnostic and Therapeutic Challenges of Pediatric community acquired Pneumonia. Epidemiol Sci, 12: 450. DOI: 10.4172/2161-1165.1000450
Copyright: © 2022 Britton P. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1071
- [From(publication date): 0-2022 - Jan 12, 2025]
- Breakdown by view type
- HTML page views: 885
- PDF downloads: 186