Outcomes of Non-Surgical Spinal Decompression Therapy in Patients with a Herniated Disc Across Different Age Groups
Received: 09-Jan-2023 / Manuscript No. jnp-23-86374 / Editor assigned: 11-Jan-2023 / PreQC No. jnp-23-86374 (PQ) / Reviewed: 25-Jan-2023 / QC No. jnp-23-86374 / Revised: 30-Jan-2023 / Manuscript No. jnp-23-86374 / Published Date: 06-Feb-2023
Abstract
A retrospective trial conducted in an independent clinic focused on the efficiency of a novel spinal decompression method and the dependence of its outcomes on patients’ age. Questionnaires of thirty-eight adult patients diagnosed with lumbar or cervical disc herniation treated with a spinal decompression (BTL Industries Ltd.) treatment program comprising 6 therapy sessions were reviewed. Oswestry low back pain questionnaire or Neck disability questionnaire and Numeric Pain Rating Scale obtained before the first and after the last treatment was assessed.
Significant improvement by 26% and 31% in the disability index and by 48% and 53% in pain perception was reported for disc herniation at the lumbar and cervical levels, respectively. While a significant correlation between patients’ age and Oswestry Disability Index obtained before and after the spinal decompression treatment program was observed, there was no significant association between age and the magnitude of therapy outcomes. Spinal decompression therapy demonstrated a significant impact in patients with herniated discs at both lumbar and cervical levels. No significant association between patients’ age and therapy outcomes was observed, predisposing this approach to becoming a universal tool in the treatment of back pain regardless of patients’ age, herniated disc location, or movement limitations.
Keywords
Cervical disc herniation; Lumbar disc herniat ion; Neck disability index; Non-surgical spinal decompression; Numeric pain rating scale; Oswestry disability index
Lay abstract
A herniated disc is the most common cause of back pain. Novel spinal decompression technology enables treatment without the active involvement of the patient, which can be advantageous, especially in the treatment of elderly patients.
Thirty-eight participants of different age groups suffering from disc herniation in the lumbar or cervical region underwent six spinal decompression treatments during a two-week period. Patients were asked to self-fill standardized disability questionnaires and to selfevaluate their pain perception before the first and after the last treatment. By comparing the before and after scores, an improvement of 26% and 31% in the disability and 48% and 53% in pain perception were reported for lumbar and cervical levels, respectively. No association between patients’ age and therapy outcomes was found which leads to the assumption that the device has the potential to achieve similar results on patients of all age groups.
Introduction
An intervertebral disc comprises three main parts - the nucleus pulposus, the annulus fibrosus, and the cartilaginous endplates forming a mechanical barrier. Annulus fibrosus forms an outer ring around the gel-like nucleus pulposus capable of withstanding axial loads [1, 2].
Damage of annulus fibrosus and consecutive displacement of nucleus pulposus from intervertebral space is called disc herniation [3, 4]. The main causes of such conditions include degenerative processes associated with loss of hydration and weakening of the nucleus pulposus due to aging and trauma mostly caused by heavy lifting, extensive flexion, and twisting [2, 3].
Even though the most prone to a herniated disc are patients in their third to the fifth decade of life, based on the identified risk factors, this condition can happen to almost anyone regardless of age [3]. Major risk factors include obesity, diabetes, hyperlipidemia, smoking, a job involving strenuous physical activity or high level of stress, genetics, and aging [2, 5-13].
Due to the global population aging, an increase in the number of elderly patients with disc herniation is expected in the future [14]. Thus it is essential to develop procedures in the treatment of herniated discs that are suitable for all age groups and provide effective treatment regardless of the patient's physical condition and abilities.
Current treatment modalities involve drug therapy, conventional physiotherapy programs, and surgical intervention. Even though these methods are proven and effective, they show varying degrees of suitability for individual age groups. Medication brings a risk of multiple adverse events, addictions, and polypharmacy, mostly in the elderly and patients with associated disorders, e.g. depression, anxiety, and sleep disorders [15, 16]. Conventional physiotherapy is usually provided in the form of a multimodal package containing multiple physiotherapy methods. Despite the low risk of side effects and zero downtime, achieving the desired improvement can be somehow complicated, especially in older patients, due to reduced mobility. There is existing clinical evidence considering different physical activities as unsuitable in the treatment of elderly patients with chronic low back pain [17, 18]. Surgery is considered the last source of relief due to the associated risk of complications, required postoperative downtime and rehabilitation, the possibility of necessary reoperation, and of course high cost.
The constraints of current techniques create space for new technologies that will bring relief to a similar extent to all patients, regardless of age or other limitations. It is recommended to implement approaches in which the patient is only passively present and the impaired segment is stimulated by external manipulation. Such an alternative might represent non-surgical spinal decompression therapy applying an external force to the patient positioned on the treatment couch. The primary aim of the present trial is to confirm the safety and efficacy of spinal decompression therapy in patients with herniated discs. The existing clinical evidence focuses on patients within productive age, who statistically represent the most at-risk group. The current trial, as a secondary aim, will evaluate the association between outcomes and patients’ age [19-26].
Methods
Private clinic ЗДОРОВЬЕ ВСЕМ (Zdorovje Vsem, Tashkent, Uzbekistan) conducted this retrospective pilot trial with the primary aim of objectively evaluating short-term effects of spinal decompression therapy in individuals with cervical and lumbar disc herniation. The secondary aim was to evaluate the relationship between outcome measures and patients’ age.
Male and female adult participants experiencing lumbar or cervical back pain due to herniated disc willing to sign written consent were included. Non-cooperative or pregnant patients with conditions including disc extrusion or sequestration, spinal stenosis, spinal tumors, spinal infections, vertebra fracture, previous spinal surgery, and severe vascular/ pulmonary or coronary artery diseases were excluded.
Before the first treatment session, every patient received and signed written informed consent containing information about the course of the treatment program, possible side effects, benefits, and agreement with participation and possible future results publication. The study was designed in accordance with the 1975 Declaration of Helsinki ethical guidelines adopted by the General Assembly of the World Medical Association (1997-2000) and by the Convention on Human Rights and Biomedicine of the Council of Europe (1997) [27, 28].
The treatment protocol consisted of 6 spinal decompression therapies (BTL Industries Ltd.) performed over the course of 3 weeks (2 therapies/week). During the treatment, the patient was positioned on the treatment couch in a supine, prone, or side-line position and fixed by a system of belts. For treatment of the cervical area, the patient's head was placed on the integrated cervical slider enabling tilt in the range of 0-30° to target energy to the proper segment of the cervical spine. To the best of the author's knowledge, this is the first accessory enabling precise spinal decompression therapy settings for the treatment of the neck area. Patients’ position was further fine-tuned via a system of movable parts to target the exact spot of the impaired segment. For the lumbar region, the angle was tilted within the range of 0-25° while for the thoracic region, the cervical adapter was used. Before the beginning of the active part of the therapy, force settings were precisely adjusted by 100-gram step increments according to patients’ tolerance and health condition. Fine-tuning of applied force via integrated traction test is essential for successful therapy outcomes. For lumbar treatment, the force did not exceed 50% of the patient’s body weight while for cervical treatment limitation was 20%. Once the stimulation part was over, the patient was asked to remain in a stable position to relax and stabilize.
Outcomes of spinal decompression therapy were measured by the changes in the Numeric Pain Rating Scale (NPRS), Oswestry Disability Index (ODI) in patients experiencing pain in the lumbar region, and Neck Disability Index (NDI) in patients with cervical pain. These were obtained via Russian versions of the Oswestry low back pain questionnaire, NDI questionnaire and standard NPRS before the first and after the last treatment [29, 30]. The Numeric Pain Rating Scale belongs to standard pain assessment tools [7]. Patients are asked to circle the number between 0 representing “no pain at all” and 10 representing “the worst ever possible pain”. The main advantage of this method is the fact that it can be assessed verbally, e.g., during a phone interview [31]. The level of disability during day-to-day activities was determined by the Oswestry low back pain questionnaire. To evaluate the final score, ten categories assessing limitations in regular life are rated and multiplied by two. Similarly, the Neck Disability Index questionnaire determines the level of daily life limitation due to neck pain.
Custom-written program (MatLab software processes, MatLab R2010b, Mathworks, Inc., Natick, MA, USA) was prepared for data analysis and statistical evaluation. Statistical analysis included a nonparametric Wilcoxon paired test following a test of data normality (Shapiro-Wilk test). Correlations were evaluated using the Pearson correlation coefficient. Relationships between ODI/NPRS data obtained before and after the full course of the study and patients’ age were assessed. Association between baseline and after score difference as a measure of improvement and patients’ age was evaluated. Improvement was also numerically expressed by averaging baseline and after-score differences across the patients (Mean Improvement).
Results
Between February 2021 and March 2021, a total of 38 patients with the same sex ratio and mean age of 41.22 (15.73) were assigned in the current retrospective clinical study. Among enrolled participants, 7 were suffering from cervical pain while the remaining 31 were dealing with low back pain. Two patients reporting lower back pain were diagnosed with multiple disc herniation, 18 of the remaining patients had herniation at the L4-L5 level and 11 at the L5-S1 level. Among patients suffering from cervical pain, 5 patients were diagnosed with herniation at the C6-C7 level and 2 patients at the C5-C6 level. No adverse events were reported throughout the trial.
Oswestry Disability Index
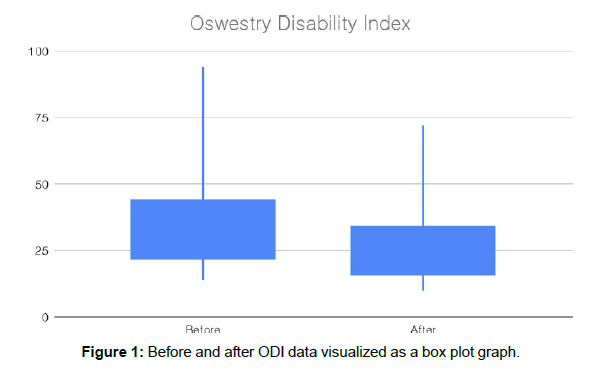
At baseline, participants experiencing low back pain responded with a mean score of 35.16 (18.68) while after 6 treatments the assessed score decreased to 26.13 (14.71). A mean improvement of 9.03 (5.49) expressed as a percentage change from baseline data 26% is statistically significant (P<0.05). All participants treated at the lumbar spine level reported improvement in terms of disability after the study course.
The distribution of before and after ODI data is graphically displayed via a box plot in Figure 1. The decrease and hence the improvement of the baseline data is noticeable.
Neck Disability Index
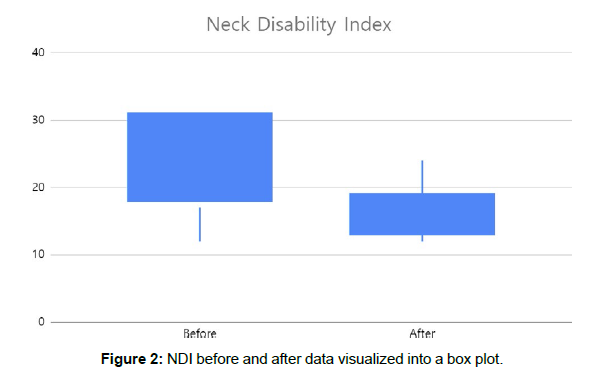
At baseline, participants suffering from cervical pain responded with a mean score of 22.86 (8.86) while after 6 treatments the obtained score decreased to 15.71 (5.82). A Mean Improvement of 7.14 (5.52) expressed as a percentage change from baseline data 31% is statistically significant (P<0.05). All participants treated at the cervical spine level reported improvement in terms of disability after finishing the study course.
The distribution of before and after NDI data is graphically displayed via a box plot in (Figure 2). The drop and thus improvement of the baseline data is noticeable.
Numeric Pain Rating Scale
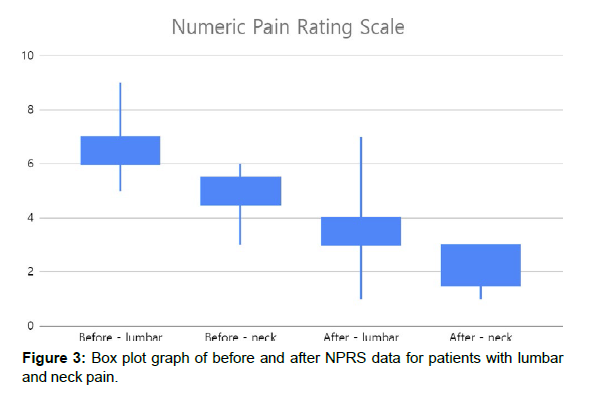
Baseline NPRS data of patients treated at lumbar level 6.32 (1.01) were slightly higher than NPRS baseline values of patients with cervical pain 4.86 (1.07). After 6 spinal decompression treatments, scores dropped for lumbar pain to 3.42 (1.15) and cervical pain to 2.29 (0.95). Both groups experienced significant improvement (P<0.05) with Mean Improvements of 3.03 (1.62) and 2.57 (0.53) and percentage changes of 48% and 53% for the lumbar and cervical groups respectively. Data are graphically visualized in (Figure 3). All patients except for three experienced improvements in terms of pain perception. Two patients stayed with no difference while one patient reported worse pain after the spinal decompression treatment program.
Relationship between age and ODI/NPRS
ODI/NPRS data were analyzed for possible dependence on age in patients with low back pain. The Group of patients with cervical pain was too small and hence insufficient for such analysis.
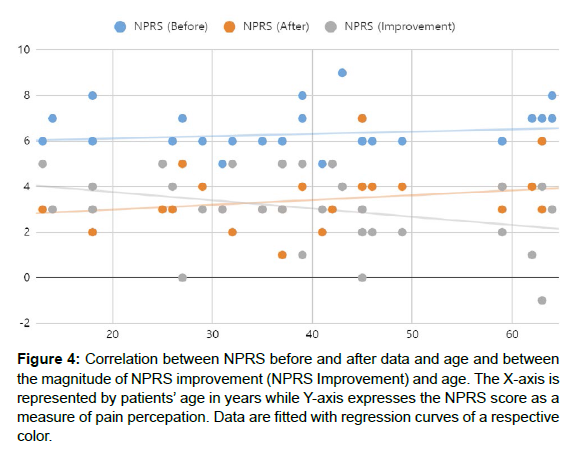
The correlation coefficient between before/after NPRS data and age indicated a non-significant small positive relationship while there was a non-significant very small negative relationship between age and magnitude of NPRS improvement (Figure 4).
Figure 4: Correlation between NPRS before and after data and age and between the magnitude of NPRS improvement (NPRS Improvement) and age. The X-axis is represented by patients’ age in years while Y-axis expresses the NPRS score as a measure of pain percepation. Data are fitted with regression curves of a respective color.
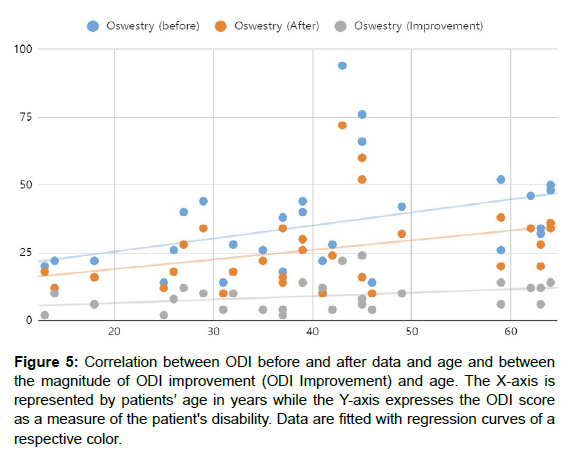
The correlation coefficient between before/after ODI data and age indicated a significant (P<0.05) medium-positive relationship. There was a non-significant medium positive relationship between age and the magnitude of ODI improvement (Figure 5).
Figure 5: Correlation between ODI before and after data and age and between the magnitude of ODI improvement (ODI Improvement) and age. The X-axis is represented by patients’ age in years while the Y-axis expresses the ODI score as a measure of the patient's disability. Data are fitted with regression curves of a respective color.
Discussion
The current retrospective pilot trial confirmed the expected significant impact of non-surgical spinal decompression therapy on pain and disability levels in patients with lumbar and cervical disc herniation. Improvement by 26% and 31% in the disability index and by 48% and 53% in pain perception was reported by participants suffering from pain at the lumbar and cervical levels, respectively. Such finding is consistent with existing clinical evidence [19-26]. Compared to the previous studies, the present one is based on a significantly lower number of therapy sessions. Previously, 15-20 spinal decompression treatments were considered necessary to achieve significant improvement, currently, only 6 sessions were performed with satisfactory results.
To better understand reported results, it is essential to describe the principle of spinal decompression technology. The spinal nerve root decompression is performed non-surgically by providing a motorized segmental distraction for a specific time inducing a physical change to the disc. A sensitive computerized feedback mechanism controls the amount of delivered decompression force to precisely dose the required spinal load. This prevents an excessive increase in muscle tone, cause of muscular or ligamentous stress and thus para-spinal muscle spasms. Decompression force yields a widening of intervertebral space, creating negative pressure within the impaired segment and therefore decreasing pressure on the disc. Disc height restoration and disc repositioning may be accompanied [32]. In the present trial, a spinal decompression device (BTL Industries Ltd.) with the most precise force dosing system enabling incremental steps of 100g and a positioning system with the greatest settings variability was used. It is believed that fine-tuning patients’ positions by moving and tilting various parts of the treatment couch yields targeting of specific spots within the impaired segment. Subsequent delivery of precisely dosed energy is resulting in effective treatment within fewer treatment sessions.
The entire procedure is performed in a comfortable lying position without the need for the patient's assistance. Thus the therapy is suitable for both patients with reduced mobility and those without major limitations. The enormous range of symptoms and ages of patients with herniated discs predetermines this device to become an indispensable tool of every practice. The secondary aim of the present study was to determine the relationship between patients’ age and spinal decompression therapy outcomes.
While a significant correlation between patients’ age and ODI obtained before and after the spinal decompression treatment program was observed, there was no significant association between age and magnitude of therapy outcomes. The relationship between pain perception and disability and patients’ age was previously studied and conclusions are well-aligned with the findings of the present trial. Gautschi et al. conducted research focusing on the influence of age on pain intensity, functional impairment, and health-related quality of life in patients undergoing surgery for lumbar degenerative disc disease [14]. While there was no relationship between age and pain, a weak correlation has been found between age and ODI. Thomas et al. were specifically focusing on the prevalence of pain and pain interference within the population of older adults [33]. Similarly to Gautschi, while no relationship between pain and age was found, the positive association between interference of pain with everyday life and patients’ age was reported.
A significant correlation between the patient's age and pre/posttreatment disability score indicates that with aging the degree of disability is naturally worsing . Interestingly, this trend was not reflected in the magnitude of ODI improvement leading to the conclusion that there is no clear association between age and outcomes of spinal decompression therapy [10]. In other words, it is believed that spinal decompression therapy yields the same effect on patients among all age groups. This finding makes the technology a universal tool for patients suffering from back pain caused by herniated discs.
We have to admit that the current study has certain limitations, of which probably the most important is the absence of a control group. The necessity to compare results to a sham group of untreated patients or to distinguish the difference between innovative approaches and traditional therapy methods is essential for the validation of outcomes. Furthermore, the number of enrolled participants was insufficient - the cohort of patients with neck pain was so small that it did not enable more detailed analysis. For evaluation of age impact, significantly more patients among all age groups should be included. Finally, a follow-up period for the evaluation of long-term results is missing.
Using subjective methods such as the Numeric Pain Rating Scale, Oswestry Disability Index, and Neck Disability Index might be considered as another limitation, but it must be considered that these tools are commonly used during research assessing the impact of various aspects in patients with back pain [19-26].
As a pilot study, the current research certainly shows limitations, but the findings regarding the effect of spinal decompression therapy on patients of different ages give clinical specialists important information about the suitable approach in the treatment of herniated discs. Despite the existence of many treatment methods and procedures, there is a lack of treatments suitable and effective across all age groups. Spinal decompression therapy demonstrated effects in patients regardless of their age or movement limitations. In addition, it does not require downtime and brings almost no risk of side effects. Follow-up studies should aim to verify the conclusions on a larger number of patients and other spinal regions and conditions.
Acknowledgement
The authors would like to acknowledge and thank the patients and staff who participated in the treatment program. The authors have no conflicts of interest to declare.
References
- Nedresky D, Reddy V, Singh G (2022) Anatomy, Back, Nucleus Pulposus. StatPearls Publishing LLC, United states.
- Schroeder GD, Guyre CA , Vaccaro AR (2016) The epidemiology and pathophysiology of lumbar disc herniations. Semin Spine Surg 28 : 2-7.
- Dydyk AM, Ngnitewe Massa R, Mesfin FB (2022) Disc Herniation. StatPearls Publishing LLC, United states.
- Azemi ES, Kola S, Kola I, Tanka M, Bilaj F, Abazaj E (2022) Lumbar Disk Herniation: A Clinical Epidemiological and Radiological Evaluation. J Med Sci 10(B):1588-1594.
- Shiri R, Lallukka T, Karppinen J, Viikari-Juntura E (2014) Obesity as a risk factor for sciatica: a meta-analysis. Am J Epidemiol 179:929-937.
- Weiler C, Lopez-Ramos M, Mayer HM, Korge A, Siepe CJ ,et.al.(2011) Histological analysis of surgical lumbar intervertebral disc tissue provides evidence for an association between disc degeneration and increased body mass index. BMC Res Notes 16:4-497.
- Meredith DS, Huang RC, Nguyen J, Lyman S (2010). Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J 10:575-580.
- Mobbs RJ, Newcombe RL, Chandran KN (2001). Lumbar discectomy and the diabetic patient: incidence and outcome. J Clin Neurosci 8:10-3.
- Longo UG, Denaro L, Spiezia F, Forriol F, Maffulli N, Denaro V (2011). Symptomatic disc herniation and serum lipid levels. Eur Spine J. 2011 Oct;20(10):1658-62. Epub 2011 Mar 9 .
- Jordan J, Konstantinou K, O'Dowd J (2009) Herniated lumbar disc. BMJ Clin Evid 26:1118.
- Sørensen IG, Jacobsen P, Gyntelberg F, Suadicani P (2011). Occupational and other predictors of herniated lumbar disc disease-a 33-year follow-up in the Copenhagen male study. Spine 36 :1541-1546 .
- Zhang YG, Sun Z, Zhang Z, Liu J, Guo X (2009) Risk factors for lumbar intervertebral disc herniation in Chinese population: a case-control study. Spine : 34(25):E918-22.
- Gautschi OP, Smoll NR, Joswig H, Corniola MV, Schaller K, et.al . (2016) Influence of age on pain intensity, functional impairment and health-related quality of life before and after surgery for lumbar degenerative disc disease. Clin Neurol Neurosurg. 150:33-39 .
- Ali A, Arif AW, Bhan C, Kumar D, Malik MB,et.al. (2018) Managing Chronic Pain in the Elderly: An Overview of the Recent Therapeutic Advancements. Cureus. 13:10(9):e3293.
- Park HJ, Moon DE. Pharmacologic management of chronic pain. Korean J Pain. 2010 Jun;23(2):99-108. doi: 10.3344/kjp.2010.23.2.99. Epub 2010 May 31. PMID: 20556211; PMCID: PMC2886242.
- Teut M, Knilli J, Daus D, Roll S, Witt CM (2016). Qigong or Yoga Versus No Intervention in Older Adults With Chronic Low Back Pain-A Randomized Controlled Trial. J Pain.17:796-805.
- Ma, Sang-Yeol & Je, Hyun & Kim, Hyeong-Dong. (2011). A Multimodal Treatment Approach using Spinal Decompression via SpineMED, Flexion-Distraction Mobilization of the Cervical Spine, and Cervical Stabilization Exercises for the Treatment of Cervical Radiculopathy. J Phys Ther Sci23. 1-6 .
- Gaowgzeh RAM, Chevidikunnan MF, BinMulayh EA, Khan F (2020). Effect of spinal decompression therapy and core stabilization exercises in management of lumbar disc prolapse: A single blind randomized controlled trial. J Back Musculoskelet Rehabil. 33:225-231.
- Choi J, Lee S, Hwangbo G (2015). Influences of spinal decompression therapy and general traction therapy on the pain, disability, and straight leg raising of patients with intervertebral disc herniation. J Phys Ther Sci. 27(2):481-3.
- Hakkinen A, Kautiainen H, Jarvenpaa S, Arkela-Kautiainen M, Ylinen J (2007). Changes in the total Oswestry Index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J.16:347-52 .
- Yang HS, Yoo WG (2014). The Effects of Stretching with Lumbar Traction on VAS and Oswestry Scales of Patients with Lumbar 4-5 Herniated Intervertebral Disc. J Phys The Sci. 2014 26:1049-50.
- Demirel A, Yorubulut M, Ergun N (2017). Regression of lumbar disc herniation by physiotherapy. Does non-surgical spinal decompression therapy make a difference? Double-blind randomized controlled trial. J Back Musculoskelet Rehabil. 22:30:1015-1022 .
- Ma,Sang-Yeol and Hyeong-Dong Kim (2010). “The Efficacy of Spinal Decompression via DRX3000 Combined with a Spinal Mobilization and a Lumbar Stabilization Exercise Program for Patients with Discogenic Low Back Pain”.J Phys Ther Sci.22 : 345-354.
- Pattern and Outcome of Surgery for Degenerative Disease of the Lumbar Spine using the Visual Analogue Score (VAS) and Oswestry Disability Index (ODI) at a Tertiary Hospital. Clin Surg 5: 2775.
- World Medical Association Declaration of Helsinki (1997) JAMA 277: 925.
- Council of Europe (1997) Convention for Protection of Human Rights and Dignity of the Human Being with Regard to the Application of Biology and Biomedicine: Convention on Human Rights and Biomedicine. Kennedy Inst Ethics J 7: 277-290.
- Yu EM , Nosova EV, Falkenstein Y, Prasad P, Leasure JM ,et al (2016). Validation of a Russian Language Oswestry Disability Index Questionnaire. Global Spine J.6:636-639.
- Bakhtadze MA, Vernon H, Zakharova OB, Kuzminov KO, Bolotov DA (2015). The Neck Disability Index-Russian Language Version (NDI-RU): A Study of Validity and Reliability. 40:1115-21.
- Haefeli M, Elfering A (2006). Pain assessment. Eur Spine J. 15 S17-24.
- Amjad F, Mohseni-BandpeiM A , Gilani S A. ,et al. (2022) Effects of non-surgical decompression therapy in addition to routine physical therapy on pain, range of motion, endurance, functional disability and quality of life versus routine physical therapy alone in patients with lumbar radiculopathy; a randomized controlled trial. BMC Musculoskelet Disord 23, 255
- Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain. 2004 Jul;110(1-2):361-8. doi: 10.1016/j.pain.2004.04.017.
- Amjad F, Mohseni-Bandpei M A , Gilani S A. ,et al. (2022) Effects of non-surgical decompression therapy in addition to routine physical therapy on pain, range of motion, endurance, functional disability and quality of life versus routine physical therapy alone in patients with lumbar radiculopathy; a randomized controlled trial. BMC Musculoskelet Disord 23, 255
- Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain.110::361-8.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Kasimovich KN, Dmitrievich SE (2023) Outcomes of Non-Surgical SpinalDecompression Therapy in Patients with a Herniated Disc Across Different AgeGroups. J Nov Physiother 13: 564.
Copyright: © 2023 Kasimovich KN, et al. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2027
- [From(publication date): 0-2023 - Apr 03, 2025]
- Breakdown by view type
- HTML page views: 1713
- PDF downloads: 314