Outcome: Hematopoietic Stem Cell Transplantation Experience of a Single Centre
Received: 03-Jul-2022 / Manuscript No. jcet-22-70896 / Editor assigned: 06-Jul-2022 / PreQC No. jcet-22-70896 / Reviewed: 20-Jul-2022 / QC No. jcet-22-70896 / Revised: 23-Aug-2022 / Manuscript No. jcet-22-70896 / Published Date: 30-Jul-2022 DOI: 10.4172/2475-7640.1000137
Abstract
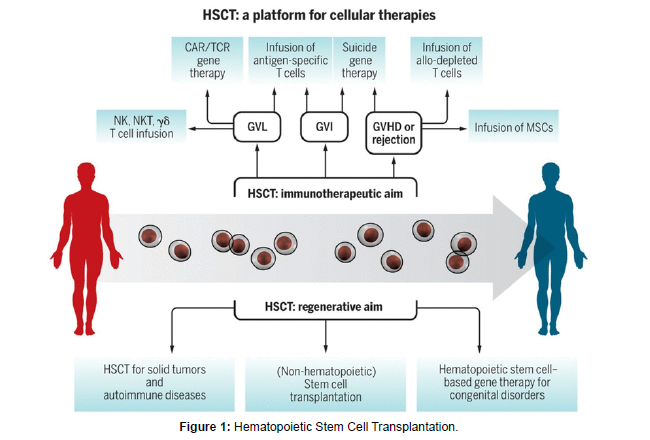
Many haematological disease patients can be cured with hematopoietic stem cell transplantation. Genetic inequity between donors and recipients, particularly when it involves the human leukocyte antigen system, is a crucial determinant in the success of transplants. To assess retrospectively the characteristics of the donors and their relationships to the occurrence of acute and chronic graft-versus-host disease, disease-free survival, and overall survival in a Brazilian population that underwent allogeneic hematopoietic stem cell transplantation between 1994 and 2012 at a single centre. There were 347 transplants that happened one after another. There were substantially more related transplants (81.2%) than unrelated transplants (18.7%); donor and recipient median ages were 34 and 33 years, respectively; and 333 (95.9%) patients had donor HLAs that matched their HLAs. ABO incompatibility, CMV status, and donor gender had no impact on the total five-year survival rate. In univariate analysis, the occurrence of acute graft-versus-host disease had a detrimental effect on overall survival. For many patients suffering from hematologic diseases, hematopoietic stem cell transplantation (HSCT) is a curative procedure. The plan is to use healthy hematopoietic stem cells from an HLA-compatible donor to replace the patient’s immune and hematopoietic systems. For HSCT to be successful, genetic differences between the donor and recipient, particularly at HLA loci, are crucial. Acute and chronic graft-versus-host disease (GVHD) continue to be major causes of morbidity and mortality after HSCT despite improvements in genetic characterisation, immuno-suppressive medications, and supportive treatment. Along with genetic differences and GVHD, the source of the stem cells, conditioning regimens, and infection problems are linked to the success of HSCT.
Keywords: Transplantation; Antibodies; Hematopoietic Stem Cell; Lymphoblastic
Introduction
Other donor-related factors, such as gender, age, and the presence or absence of cytomegalovirus (CMV) antibodies with their distinct roles having been investigated with varying degrees of success, ABO incompatibility may also be related to the results of HSCT. 7–10 The reactivation of CMV illness is still a significant source of morbidity and mortality despite preventative therapy. The development of reduced intensity conditioning (RIC) regimens has led to an increase in the number of people over 50 who undergo HSCT. Because of the regeneration potential of hematopoietic stem cells (HSC) and potential comorbidities, older related suitable donors are also accepted, and recent research have shown that donor age may be a risk factor for acute and chronic GVHD [1]. Currently, ABO incompatibility is present in between 30 and 50 percent of HSCT procedures. Although it is commonly known that ABO incompatibility raises the risk of haemolytic responses, recent research indicates that it has no impact on the results of HSCT. In this study, the effects of donor attributes such age, gender, CMV status, cell source, ABO compatibility, and donor type were assessed. the results of 347 patients who underwent HSCT at the Hospital de Clinics in Porto Alegre, southern Brazil. We were interested in learning whether these traits may be used to predict outcomes in this Latin American cohort of patients who underwent single-center transplants [2].
Materials and Method
Retrospective evaluations were performed on 347 patients who underwent allogeneic HSCT at a single location between January 1994 and December 2012. Acute and chronic GVHD, disease-free survival (DFS), and overall survival were all connected with the donor and recipient ages, gender, CMV status, ABO compatibility, type of donor (matched related and matched unrelated), and patient’s disease status (OS). At the time of the procedure, each patient provided written informed permission, and the local ethics committee authorised the study [3-5]. Refractory disease, a second or more remission from a cancerous condition, or a diagnosis of a benign condition more than a year old were all considered to have advanced disease status at HSCT. Prior to 2000, poor resolution DNA-based typing was used to determine the HLA Class I and Class II of patients and related donors. Since 2005, unrelated donor HSCT procedures have been carried out in this centre. High resolution HLA typing was done for 6/6 matches up until 2008 and 8/8 or 10/10 matches after that. Standard myeloablative conditioning (MAC) included total body irradiation (TBI), 2 60 mg/ kg of cyclophosphamide (CY), and 14–16 mg/kg of oral busulfan (BU) (12 Gy fractioned dosage). The following RIC regimens were used: BU 8–10 mg/kg PO + Flu (90–120 mg/m2), Flu (120 mg/m2) plus Melphalan (140 mg/m2), or CY 60 mg/kg. Additionally, patients undergoing MUD transplants were given rabbit thymoglobulin (7–14 mg/kg) [6].
Patients on the MDR and MAC regimens started receiving cyclosporin A (CYA) (3 mg/kg IV) on Day 1 and a short course of methotrexate (MTX) (15 mg/m2) on Day 1 and 10 mg/m2 on Days +3, +6 and +11. Tacrolimus (0.05 mg/kg IV) was used with a brief course of MTX for people receiving MUD transplantation. For RIC, GVHD prophylaxis was achieved by starting on Day 2 with 3 mg/kg PO of pluS CYA and 2 g mycophenolate mofetil per day [7-9]. The brief course of MTX was not used when umbilical cord HSC was the source. Peripheral granulocyte counts over 500/-L for three straight days were engraftment. When engraftment was not achieved in the parent tissue, the failure or rejection of the patients who remained alive following a transplant for more than 28 days. Day 100 following the operation saw a calculation of the engraftment failure rate [10].
Laminar high efficiency particulate air (HEPA) filters were used to keep all patients in a secure setting. All patients received standard prophylactic doses of acyclovir, fluconazole, and sulfamethoxazole along with trimethoprim. Weekly CMV monitoring was done via antigenemia assaying after 2005 and qualitative DNA-polymerase chain reaction (PCR) up until that point. After two consecutive positive PCR results or one positive cell in the antigenemia assay, preventive 10 mg/kg ganciclovir was started [11]. All blood components underwent irradiation and filtration. According to the guidelines issued by the hospital transfusion committee, minimum values were established to initiate platelet and red blood cell transfusions to maintain platelet counts above 20 109/L and haemoglobin levels above 7 g/dL, respectively. Broad-spectrum antibiotics were used to treat neutropenic fever, according to base on our microbiological sensitivity profile and the Infection Dis- eases Society of America (IDSA) Guidelines for our hospital protocols [12]
Patients’ and donors’ characteristics are shown as frequencies for categorical variables and as medians and ranges for continuous variables. The OS was the main outcome measure, and the incidence of acute and chronic GVHD, DFS, and transplant-related mortality served as secondary endpoints (TRM). The number and severity of organ involvement were used to stage and grade acute GVHD (Grade 0-IV). Utilizing the Kaplan-Meyer method, OS was calculated. The logrank test was used to compare the curves. We compared categorical data using the Chi-square test. Age and gender of patients and donors, patient and donor gender combinations, patient and donor CMVserological status, stem cell source bone marrow (BM), peripheral blood stem cells (PBSC), and cord blood] were all were included in the studies. MAC vs. RIC, MUD vs. MRD, dosage of CD34+ cells, patient’s illness condition, and stem cell (CBSC). Multivariate analysis included factors with p-values 0.2. For multivariate analysis, the Cox proportional hazard regression model was employed [13].
Result
Based on the literature and the relatively lower age of patients and donors in our cohort, a cut-off value of 40 years was chosen to assess the impact of donor age on transplant outcomes. The HCPA Ethics Committee approved this study, and the Declaration of Helsinki for studies involving human subjects was followed when analysing the data in an anonymous manner [14]. Acute lymphoblastic leukaemia, 82 (23%) had chronic myeloid leukaemia, 18 (5.2%) had myelodysplastic syndrome, 21 (8.8 %) had lymphomas, 57 (16%) had aplastic anaemia, and 26 (7%) had additional diseases. In 151 (43.5%) individuals, the disease condition was progressed (beyond the second remission). In 265 (85.8%) of the patients and donors, respectively, and 218 (87.2%) of the donors, the CMV serological status was positive. The median age of the donors was 33 years, 182 (52.2%) of them were men, and 282 (81.3%) of them were connected to the recipients by blood.
Discussion
The overall group’s five-year OS was 49.1 percent 95% confidence interval (CI): 41-54 percent. In 317 patients (92.4 percent), engraftment took place, with a mean engraftment time of 19 days (range: 8–45). The average dose of CD34+ cells was 3.4 106/kg (the range was 1-34 106/ kg) .ABO incompatibility was present in 113 (32.3%) transplants with 65 recipients (18.5 percent). having 48 (13.8%) minor and 1 significant incompatibility. Major and minor incompatibility had no effect on engraftment, which took place after 20.3 days (p-value = 0.293) and 18.6 days (p-value = 0.100), respectively, compared to 19.5 days for patients without incompatibility.
Conclusion
Time to engraftment did not differ between younger (19.7 days) and older (18.7 days; p-value = 0.063) donors.185 patients (62.5%) had acute GVHD (Grades I–IV), while 131 had chronic GVHD (50.4 percent).
Both the cumulative incidence of acute GVHD for MRD vs. MUD (147- 57.5 percent and 39-65 percent, respectively; p-value = 0.358) and the cumulative incidence of chronic GVHD (110-52.6 percent and 20-46.7 percent, respectively; p-value = 0.573) did not differ. Donors older than 40 years had a considerably higher incidence of both acute and chronic GVHD. 77 people experienced acute GVHD (65.8 percent). receivers from donors who were older (>40 years) and 92 (52 percent) from donors who were younger (p-value = 0.03) Chronic GVHD occurred in 64 (43%) recipients from younger donors and 54 (60%) recipients from older (>40 years) donors (p-value = 0.015). The occurrence of acute or chronic GVHD was unaffected by ABO incompatibility, donor gender, MRD or MUD, or CMV serological status. With the advent of nonmyeloablative conditioning regimens, DNA-based high resolution HLA typing, and improved clinical support, much has been done in the last ten years to increase the efficacy of HSCT [15]. As a result, there are more MUD transplants performed globally, and while acute and chronic GVHD rates are greater, survival rates are comparable to those seen with MRD transplants. The ability to transplant older patients has increased thanks to the introduction of RIC regimens, which has led to an increase in donor age in the MRD scenario. Age of the donor and female-to-male transplants have been demonstrated to affect GVHD and survival, while these factors are still debatable. MUD transplants have involved elder donors.
Conflict of Interest
None
Acknowledgement
None
References
- Swaminathan VV, Uppuluri R, Patel S, Ravichandran N, Ramanan KM, et al (2020) Matched Family versus Alternative Donor Hematopoietic Stem Cell Transplantation for Patients with Thalassemia Major: Experience from a Tertiary Referral Center in South India. Biol Blood Marrow Transplant 26(7):1326-1331.
- Choudhary D, Sharma SK, Gupta N, Kharya G, Pavecha P, et al (2013) Treosulfan-thiotepa-fludarabine-based conditioning regimen for allogeneic transplantation in patients with thalassemia major: a single-center experience from north India. Biol Blood Marrow Transplant 19(3):492-495.
- Qatawneh M, Aljazazi M, Altarawneh M, Aljamaen H, Mustafa M, et al (2021) Hematopoietic Stem Cell Transplantation During the Era of COVID-19 in Queen Rania Children's Hospital. Mater Sociomed. 33(2):131-137.
- Shenoy S, Walters MC, Ngwube A, Soni S, Jacobsohn D, et al (2018) Unrelated Donor Transplantation in Children with Thalassemia using Reduced-Intensity Conditioning: The URTH Trial. Biol Blood Marrow Transplant (6):1216-1222.
- Holtick U, Albrecht M, Chemnitz JM, Theurich S, Skoetz N, et al (2014) Bone marrow versus peripheral blood allogeneic haematopoietic stem cell transplantation for haematological malignancies in adults. Cochrane Database Syst Rev (4):CD010189.
- Zakaria NA, Bahar R, Abdullah WZ, Mohamed Yusoff AA, Shamsuddin S, et al (2022) Genetic Manipulation Strategies for β-Thalassemia: A Review. Front Pediatr. 2022 Jun 15; 10:901605.
- Modell B, Darlison M (2008) Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 86(6):480–487.
- Mohamed SY (2017) Thalassemia Major: Transplantation or Transfusion and Chelation. Hematol Oncol Stem Cell Ther 10(4):290–298.
- Lucarelli G, Isgrò A, Sodani P, Gaziev J (2012) Hematopoietic stem cell transplantation in thalassemia and sickle cell anemia. Cold Spring Harb Perspect Med 2(5):118-125.
- Reddy NM, Perales MA (2014) Stem cell transplantation in Hodgkin lymphoma. Hematol Oncol Clin North Am 28(6):1097-1112.
- Kelta M, Zekri J, Abdelghany E, Rehman JU, Khan ZA, et al (2018) High-dose chemotherapy and peripheral hematopoietic stem cell transplantation in relapsed/refractory Hodgkin's lymphoma. Tumori. 104(6):471-475.
- Sun L, Li S, El-Jawahri A, Armand P, Dey BR, et al (2018) Autologous Stem Cell Transplantation in Elderly Lymphoma Patients in Their 70s: Outcomes and Analysis. Oncologist 23(5):624-630.
- William BM, Loberiza Jr, Whalen V, Bierman PJ, Bociek RG, et al (2013) Impact of conditioning regimen on outcome of 2-year disease-free survivors of autologous stem cell transplantation for Hodgkin lymphoma. Clin Lymphoma Myeloma Leuk 13(4):417-423.
- Grisariu S, Shapira MY, Avni B (2018) Thiotepa, Etoposide, Cyclophosphamide, Cytarabine, and Melphalan (TECAM) Conditioning Regimen for Autologous Stem Cell Transplantation in Lymphoma. Clin Lymphoma Myeloma Leuk 18(4):272-279.
- Smeltzer JP, Cashen AF, Zhang Q, Homb A, Dehdashti F(2011) Prognostic significance of FDG-PET in relapsed or refractory classical Hodgkin lymphoma treated with standard salvage chemotherapy and autologous stem cell transplantation. Biol Blood Marrow Transplant 17(11):1646-1652.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Zujia W (2022) Outcome: Hematopoietic Stem Cell Transplantation Experience of a Single Centre. J Clin Exp Transplant 7: 137. DOI: 10.4172/2475-7640.1000137
Copyright: © 2022 Zujia W. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 1742
- [From(publication date): 0-2022 - Apr 17, 2025]
- Breakdown by view type
- HTML page views: 1414
- PDF downloads: 328