Osteoid Osteoma of the Proximal Phalanx of the Hallux: A Case Report of a Challenging Diagnosis
Received: 15-Oct-2018 / Accepted Date: 31-Oct-2018 / Published Date: 07-Nov-2018 DOI: 10.4172/2329-910X.1000279
Keywords: Osteoid osteoma; Foot; Hallux; Phalanx; Excision
Level of Clinical Evidence
Four
Introduction
Osteoid osteoma (OO) is a common benign bone lesion that accounts for approximately 10% to 12% of all benign bone tumors analyzed by biopsy [1]. These tumors were first recognized in 1932 thanks to Jaffe’s work [2]. Its peak of incidence is during the second decade of life although more than 80% of lesions occur in patients between 5 to 25 years old. Males are more commonly affected with a ratio of 3:1. It is an osteoblastic tumor; at least 50% of these tumors occur in the diaphyseal and metaphyseal regions of long bones of the lower extremities. The foot is rarely involved [3], indeed in a review Jackson found an incidence of less than 4% in the foot and of 1.7% in the metatarsals [4]. It is histologically characterized by a central region of fibro-osseous tumor (usually smaller than 1.5 cm) surrounded by a distinctive zone of reactive bone sclerosis [5].
The characteristic clinical feature is a local pain pattern, which is rapidly alleviated by the administration of NSAIDs or aspirin. This pain is typically referred at rest and at night. When the lesion is superficial, it could be also associated with local swelling [6,7].
Not usual locations and unclear symptoms could delay diagnosis. The typical X-ray appearance for lesions localized in cortical bone shows a “nidus”, consisting of a central lucency surrounded by a sclerotic rim of bone. When the Osteoid osteoma is located in the cancellous bone or in the sub-periosteal region of small bones of the foot, X-ray could not exhibit the typical sclerotic image around the nidus [8,9]. This article describes the case of a 27-years-old woman with an uncommon Osteoid osteoma of the proximal phalanx of the great toe.
Method
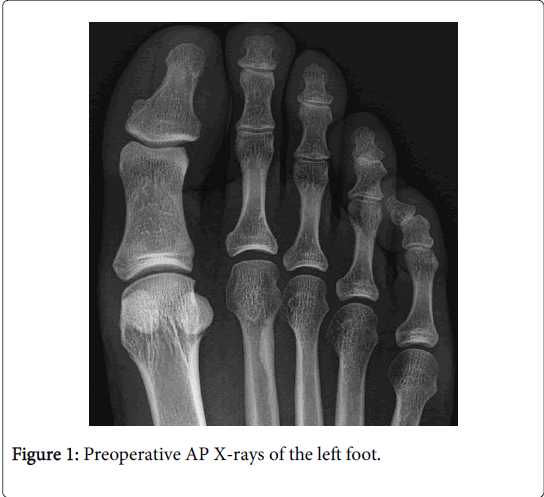
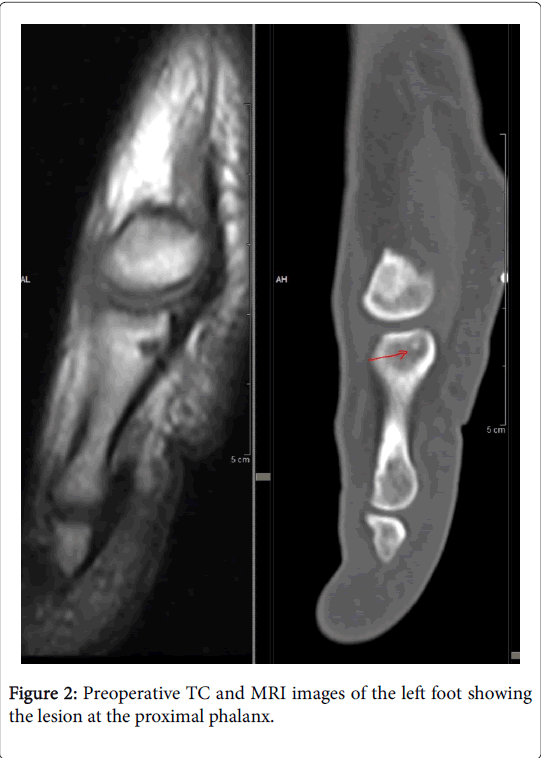
A 27-years-old woman presented in September 2016 with dull aching pain at the proximal phalanx of the great toe of the left foot for over 12 months, with no previous history of trauma, no other diseases, no allergies, no previous surgery. The patient didn’t refer about other joint pain and family history. She didn’t show any local sign, except for a slight painful motion at metatarsophalangeal joint. The pain was worse at night, but remitted partially with NSAIDs or aspirin assumption. Local palpation exacerbated the pain. There were no neurovascular disorders in the limb, laboratory parameters and inflammatory markers were within normal limits. Plain X-rays (Figure 1) didn’t show any lesion at the hallux. Otherwise CT scan and MRI revealed a focal lesion (maximum diameter 2.5 mm) with a central hypodense area and sclerotic peripheral component (Figure 2).
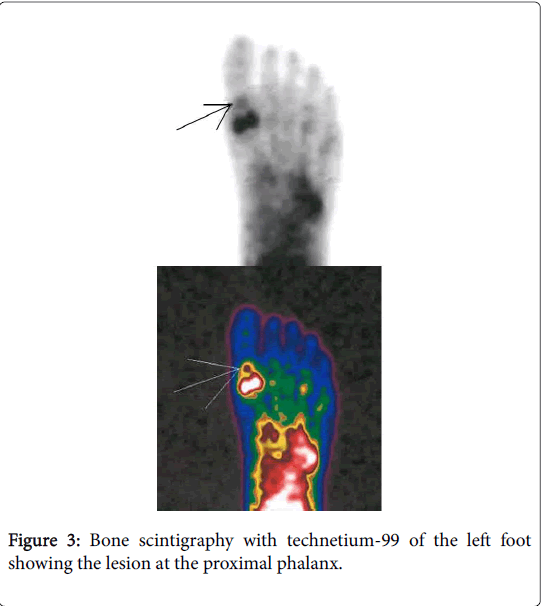
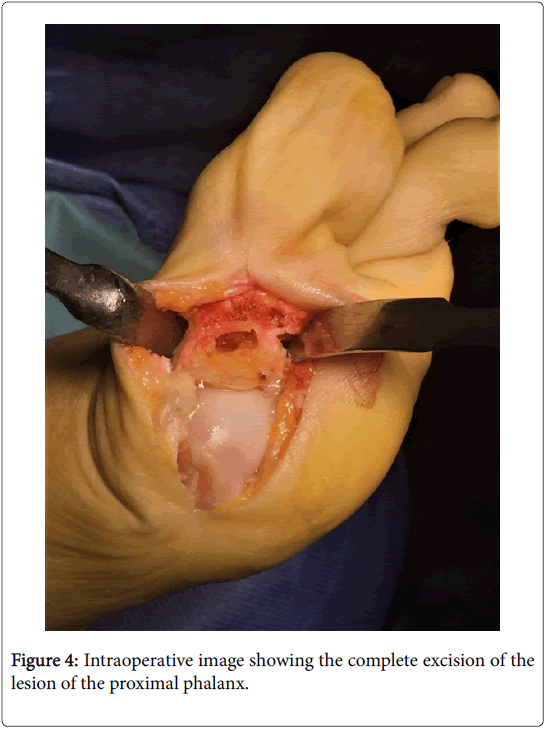
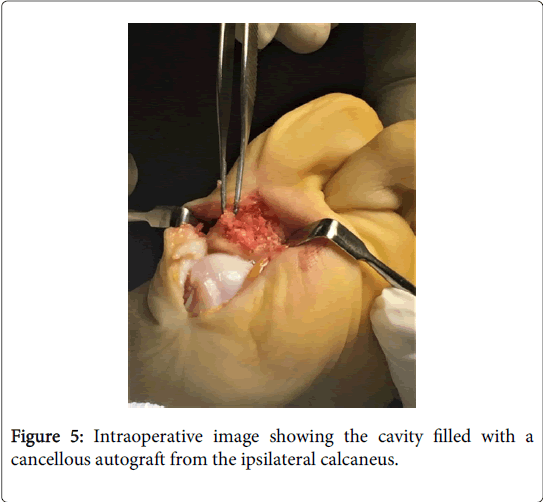
Bone scintigraphy with technetium-99 Figure 3 revealed a small area of hypermetabolic activity at the base of the proximal phalanx of the great toe to the left foot. These appearances were suggestive of an osteoid osteoma. After discussion with the patient, due to poor pain control, the decision was made to undertake an excisional biopsy of the lesion (November 2016). The definitive diagnosis could only be confirmed by histologic examination. A medial incision, centered on the lesion was made over the proximal phalanx of the hallux. The area of the lesion was identified and an en-bloc excision was performed using a chisel (Figure 4). The cavity was then filled with a cancellous autograft from the ipsilateral calcaneus (Figure 5).
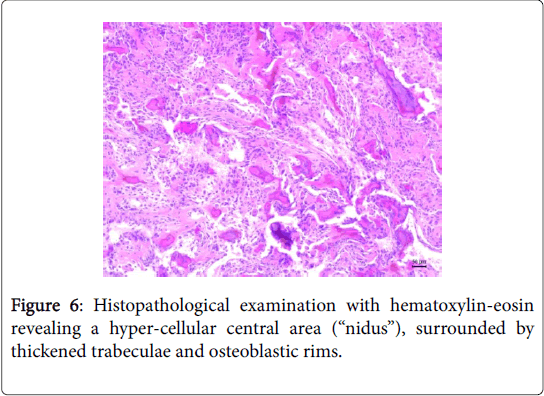
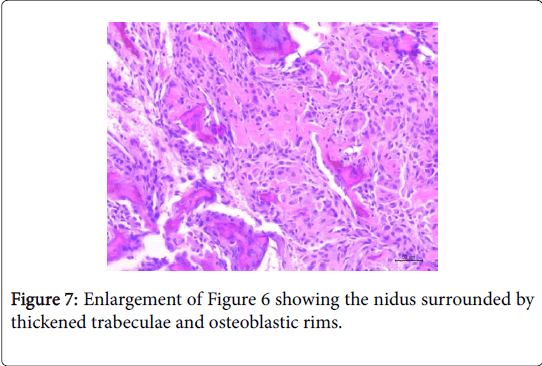
The bone wedge was sent for histopathological examination. Evaluation with hematoxylin-eosin staining revealed a hyper-cellular central area (“nidus”) without atypical cells, surrounded by areas with thickened trabeculae and osteoblastic rims (Figures 6 and 7), confirming the diagnosis of Osteoid osteoma. The patient began weight-bearing after surgery with postoperative flat-soled shoe for 4 weeks. The pain remitted immediately after surgery. Early rehabilitation showed marked improvement of joint mobility. At 12 months post-operative follow-up (November 2017), the patient remained asymptomatic with no signs of joint degeneration or any evidence of Osteoid osteoma recurrence. She resumed her usual activities and had no complications.
Discussion
Osteoid osteoma (OO) of the foot is a rare event. The talus is the most commonly involved, but other bones as the calcaneus, cuboid, navicular, and phalanges may be affected in a few cases [4,7,10-12]. Sproule reported a case of osteoid osteoma of the second toe [12]. Lacroix et al. reported a sub periosteal Osteoid osteoma at the distal phalanx of the fourth toe [13]. With regard to the great toe, cases involving the distal phalanges seem to be rare. Case reports showed Osteoid osteoma in the proximal phalanx with involvement of the interphalangeal joint, [7] and in the distal phalanx [14-17]. In this paper we report our experience with an osteoid osteoma of the proximal phalanx of the hallux, without articular involvement. The cortical type of Osteoid osteoma is the most common, but the cancellous and sub-periosteal varieties appear to be more frequent in the small bones of the hand and foot [18,19]. Local swelling and temperature increase can be confused with an infectious process, but in OO there is no increase in C-reactive protein. Kahn et al. [20] reported a case of a young female with a dull ache in the great toe, associated with local erythematous changes. X-rays revealed an area of radiolucency on the distal phalanx of the hallux. The lesion was excised and microscopy revealed signs consistent with an osteoid osteoma. In our case, the patient didn’t show local sign that could be misdiagnosed with an infectious process. Although an uncommon finding in the foot, Osteoid osteoma it should always be considered a differential diagnosis in patients presenting with a history of pain and a local increase in temperature. The X-ray appearance of Osteoid osteoma in small bones of the foot is different from long bones. In these cases the nidus is usually located in cancellous bone, and osteosclerosis is mild or absent and may be far from the lesion [14]. The case reported in this paper in fact didn’t show any sign on plain X-rays. CT scan might be helpful for the diagnosis, showing in many cases the contrast between the nidus and the normal trabecular tissue around it [21]. MRI may aid, but it is usually less useful than CT in defining bone lesions. Moreover the images may be confused with a malignant process or osteomyelitis due to edema of the cancellous bone. However further investigation with bone scintigraphy should be always performed to reach a correct diagnosis [6]. During last decades, noninvasive techniques have been used in the treatment of these lesions, such as CT guided radiofrequency ablation or thermal RFA. The reported results are similar to those obtained in open surgery, though they can’t provide a definitive histologic diagnosis. Moreover the CT-guided thermal RFA in a small area like proximal phalanx could damage the surrounding structures including the overlying skin and adjacent nerves structures. Other complications that must be taken into account are the incomplete ablation or recurrence of the lesion, or the fracture of the treated bone. For this reason, surgical resection of the lesion could be considered the treatment of choice and often lead to a resolution of the symptoms. After surgery, recurrence occurs only if the resection of the nidus is not complete [6,7]. Our patient reported a complete resolution of symptoms after surgical resection of the lesion.
Conclusion
The phalanx of the hallux is an uncommon localization for Osteoid osteoma, but this entity should be always considered as a possible diagnosis in cases of local dull nocturnal pain without associated etiology. A timely approach followed by clinical and radiological evaluation could avoid delays in diagnosis and in the definitive treatment of the lesion, which is only confirmed by surgical excision and histopathological examination. Even if plain X-rays don’t show any significant sign, in cases of persistent pain CT scan, MRI and a SPECT exam should be performed to identify the lesion and carry out a correct diagnostic and therapeutic approach.
References
- Frassica FJ, Waltrip RL, Sponseller PD, Ma LD, McCarthy EF (1996) Clinicopathologic features and treatment of osteoid osteoma and osteoblastoma in children and adolescents. Orthop Clin North Am 27: 559-574.
- Jaffe HL (1935) Osteoid osteoma: A benign osteoblastic tumour composed of osteoide and atypical bone. Arch Surg 31: 709-728.
- Spencer EE, Beirman JS, Femino JE (2002) Osteoid osteoma of the fifth metatarsal: A case report and literature review. Foot Ankle Surg 8: 71-78.
- Jackson RP, Reckling FW, Mantz FA (1977) Osteoid osteoma and osteoblastoma. Similar histologic lesions with different natural histories. Clin Orthop Relat Res 128: 303-313.
- Anderson WA, Kissane JM (1977) Pathology. St. Louis: Mosby CV pp: 1970–2011.
- Asunción J, Torrent J, González C, Poggio D (2013) Intra-articular osteoid osteoma of the first metatarsal. Foot Ankle Int 34: 448-454.
- Jowett CR, Singh D (2010) Osteoid osteoma of the great toe: A case report. Foot Ankle Surg 16: 12-15.
- Shereff MJ, Cullivan WT, Johnson KA (1983) Osteoid-osteoma of the foot. J Bone Joint Surg Am 65: 638-641.
- Shukla S, Clarke AW, Saifuddin A (2010) Imaging features of foot osteoid osteoma. Skeletal Radiol 39: 683-689.
- Benchakroun M, El Bardouni A, Kharmaz M, Zaddoug O, Chiboub H, et al. (2004) The osteoid osteoma of the foot (in about of 10 cases ). Med Foot Surg 20: 23-28.
- Ebrahimzadeh MH, Omidi-Kashani F, Hoseini MR (2009) Painful and tender toe, osteoid osteoma of the distal phalanx of toe, a diagnostic dilemma. Foot 19: 232-235.
- Sproule JA, Khan F, Fogarty EE (2004) Osteoid osteoma: Painful enlargement of the second toe. Arch Orthop Trauma Surg 124: 354-356.
- LaCroix ML, Thomas JR, Nicholas RW (2001) Subperiosteal osteoid osteoma of the distal phalanx of the fourth toe. Orthopedics 24: 695–696.
- Hattori H, Takase K, Morohashi A (2011) Osteoma osteoid of the great toe. Orthopedics 34: 432-435.
- Öztürk A, Yalçinkaya U, Özkan Y, Yalçin N (2008) Subperiosteas osteoid osteoma in the hallux of a 9-year-old female. J Foot Ankle Surg 47: 579-582.
- Rapp M, Kaiser MM (2010) Osteoid osteoma: A painless enlargement of the great toe. Surg J 5: 9-12.
- Onoue K, Kudawara I (2007) Osteoid osteoma with cartilage formation of the distal phalanx in the toe. Orthopedics 30: 670–671.
- Ekmekci P, Bostanci S, Erdogan N, Akcaboy B, Gungey E (2001) A painless subungal osteoid osteoma. Dermatol Surg 27: 764–765.
- Ostrowski ML, Spjut HJ (1997) Lesions of the bones of the hands and feet. Am J Surg Pathol 21: 676–690.
- Kahn MD, Tiano FJ, Lillie RC (1983) Osteoid osteoma of the great toe. J Foot Surg 22: 325–328.
- Franceschi F, Marinozzi A, Papalia R, Longo UG, Gualdi G, et al. (2006). Intra and juxtaarticular osteoid osteoma: A diagnostic challenge: Misdiagnosis and successful treatment: A report of four cases. Arch Orthop Trauma Surg 126: 660-667.
Citation: Attilio B, Maria LF, Alberto F, Carboni L, Carmine Z, et al. (2018) Osteoid Osteoma of the Proximal Phalanx of the Hallux: A Case Report of a Challenging Diagnosis. Clin Res Foot Ankle 6: 279. DOI: 10.4172/2329-910X.1000279
Copyright: © 2018 Attilio B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3205
- [From(publication date): 0-2015 - Feb 07, 2025]
- Breakdown by view type
- HTML page views: 2625
- PDF downloads: 580