Osteiod Osteoma of Mandibular Condyle: A Rare Case Report
Received: 07-Jun-2022 / Manuscript No. jdpm-22-66085 / Editor assigned: 09-Jun-2022 / PreQC No. jdpm-22-66085 / Reviewed: 23-Jun-2022 / QC No. jdpm-22-66085 / Revised: 28-Jun-2022 / Manuscript No. jdpm-22-66085 / Accepted Date: 04-Jul-2022 / Published Date: 05-Jul-2022 DOI: 10.4172/jdpm.1000125
Introduction
The first description of osteoid osteoma was given by Jaffe in 1935 [1]. Pathogenesis of osteoid osteoma varies from uncontrolled growth to inflammatory reaction to abnormal healing [2]. It consists of osteoid and trabeculae of new bone deposited in the basement of highly vascularized osteogenic connective tissue [3]. It is a slow‑growing lesion. The lesion usually do not grow more 2 cm in size and prevalent in young adults [4]. Here, we present a case where osteoid osteoma is located on the mandibular condyle, with size more than 2 cm which is unlike osteoid osteoma and is a rarity.
Case Report
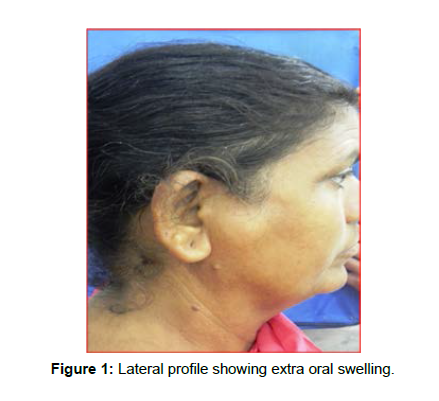
A female patient of 45 years old had asymptomatic swelling on the right side of her face (Figure 1).
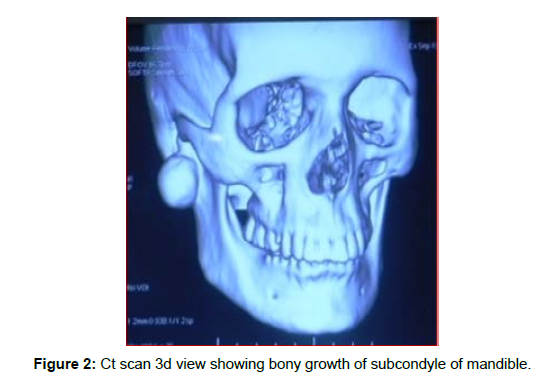
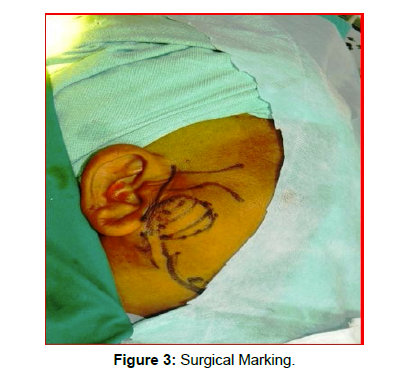
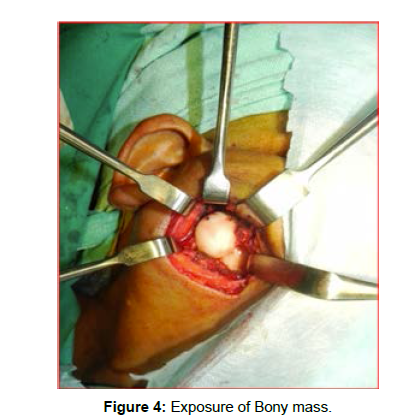
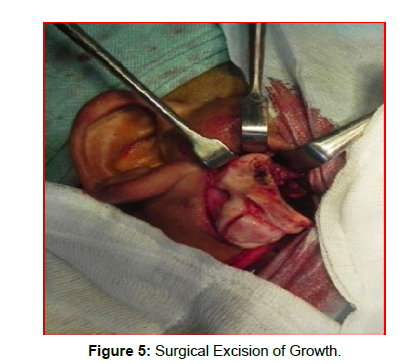
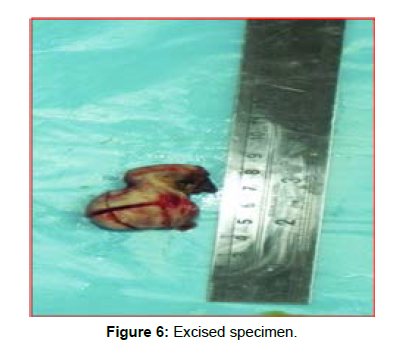
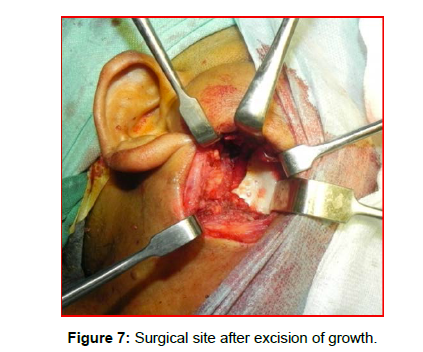
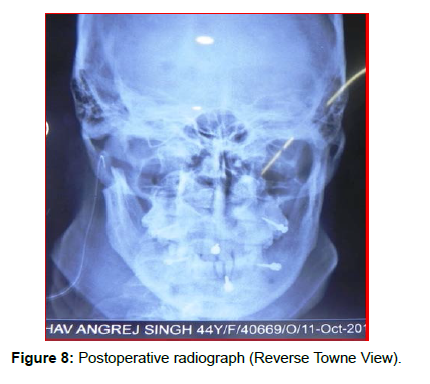
She noticed this swelling for 1½ months. It gradually increased in size. There was a prominence on Rt condyle region of mandible. No history of facial trauma was present. Medical history was not significant. There was evident extraoral swelling. The swelling was 3 cm × 3 cm in largest diameter. It was immobile, nontender, and hard. It was present along the condyle of the mandible. Computed tomography (CT) scan showed a radiopaque mass on the right condyle of mandible (Figure 2). The density of mass was similar to the adjacent bone structure. After clinical and radiographic examination, initial diagnosis of osteoma of the mandible was made. The patient was planned for surgery after all the required investigations. The lesion was planned for surgical excision. The patient was operated under general anesthesia. Retromandibular incision was used (Figure 3). Anterior parotid transmasseteric approach (Figure 4) was used. An oval mass was attached to the bone. It was removed using a bur and chisel. The mandibular condyle was also amputated as lesion was involving a major part of condyle (Figures 5‑7). Postoperative radiograph was taken (Figure 8). The specimen was sent for microscopic examination, which confirmed diagnosis as osteoid osteoma. Bone wax was used to achieve hemostasis. A layer‑by‑layer closure was done. The patient recovered well, postoperatively. Till date, no recurrence has been found. The patient is under follow‑up and will be rehabilitated using total joint replacement on the right side.Discussion
Osteoid osteoma is more prevalent in males than females in a ratio of 3:1 [5,6]. According to many authors, osteoid osteoma do not grow more than 2 cm in size [2,5,6] but in this case, osteoid osteoma was having a size of 3 cm × 3 cm. Clinically, osteoid osteoma is associated with pain, but this patient was asympatomatic. Radiographically, this lesion has a central nidus with a sclerotic bony margin. According to Jaffe [1] the central point was more radiolucent and is adjoined by reactive radiopacity, which was enlarged at irregular distances from the focal point. Premature osteoid osteoma has a radiopaque focal point; on maturation, it changes to a radiolucent focal point. According to Pritchard and Mckay [7], in the later developmental stages, calcification of the osteoid forms a central opaque body. The osteoid varies in density as per calcification stage. Osteoid osteoma is best diagnosed with CT scans. When compared with conventional radiography, CT scan shows more detail between the tumor and adjacent structures. We diagnosed this case using CT scan. CT scan disclosed the exact dimension and range of the lesion. It also helped in better surgical contemplating. In case of osteoid osteoma, Gardner syndrome should be ruled out. Gardner syndrome is an autosomal dominant trait characterized by multiple osteomas, gastrointestinal polyps, skin and soft‑tissue tumors and multiple impacted or supernumerary teeth [8]. Huvos has described three histopathologic stages of ossification [4,9]. Initial stage consists of densely packed actively proliferating osteoblasts in a highly vascularized stroma. In intermediate stage, there is osteoid deposition between the osteoblasts. In the mature stage, there is transformation of osteoid into well‑calcified compact trabeculae of an atypical bone. These trabeculae are neither woven nor lamellar. Differential diagnosis of osteoid osteoma is fibro‑osseous lesion, ossifying fibroma or giant cell granuloma. Fibrous dysplasia is a poorly defined lesion. It has radiolucent and ground‑glass appearances in the early and mature stages, respectively. Ossifying fibromas have some features identical to osteoid osteomas, both clinically and radiographically. Ossifying fibromas are without nidus and usually painless [2]. Giant cell granulomas are distinguished on the basis of multinucleated giant cells [10]. The probable etiological factors of osteoid osteomas are: developmental, neoplastic, and reactive [11]. According to some, it grows extemporaneously. Osteoid osteoma is associated with trauma and not to the inflammation [12]. In the majority of cases of Osteiod osteomas are asymptomatic. They are incidentally found on a routine radiographic survey. Osteoid osteomas remain undetected until they cause facial asymmetry or functional disability [13]. In some cases, mandibular deviation on opening, limited mandibular movement, occlusal dysfunction, headache or exophthalmos can occur. In case of large osteomas which cause facial asymmetry and functional disability, surgical intervention is advisable. Complete surgical excision is the treatment for osteoid osteomas. Osteoid osteoma of mandible can be treated by intra‑ and extraoral approaches. According to Longo et al., in case of large tumors located in posterior mandible, extraoral approach is more desirable. It allows for a better exposure and visibility.
Extraoral approach avoids damage to the important structures in the region [14]. We selected extraoral approach, as in this case, size of osteoid osteoma was large. Surgical treatment can be opted in case of cosmetic disfigurement; limitation of function, for a histopathological diagnosis, when there is a significant growth rate. Surgical treatment is also indicated when the symptoms secondary to osteoma are not improving, in spite of medical therapy.
Conclusion
Unusual positions and presentation of osteoid osteomas in and around the orofacial region should always keep in mind for management. For proper diagnosis of these lesions, good clinical knowledge is essential. Although recurrence is rare, periodic follow‑up should be done to rule out recurrence.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship: Nil
Conflicts of interest
There are no conflicts of interest.
References
- Jaffe HL (1935) Osteoid Osteoma: A Benign Osteoblastic Tumor Composed of Osteoid and Atypical Bone. Arch Surg 31: 709‑728.
- Mohammed I, Jannan NA, Elrmali A (2013) Osteoid Osteoma Associated with the Teeth: Unusual Presentation. Int J Oral Maxillofac Surg 42: 298‑302.
- Singh A, Solomon MC (2017) Osteoid Osteoma of the Mandible: A Case Report with Review of the Literature. J Dent Sci 12: 185‑189.
- Ida M, Kurabayashi T, Takahashi Y, Takagi M, Sasaki T (2002) Osteoid Osteoma in the Mandible. Dentomaxillofac Radiol 31: 385‑387.
- Gupta OP, Jain RK, Agarwal MK, Khanna S, Shrivastava A (1985) Osteoid Osteoma of the Mandible. Ear Nose Throat J 64: 206-208.
- Tochihara S, Sato T, Yamamoto H, Asada K, Ishibashi K (2001) Osteoid Osteoma in Mandibular Condyle. Int J Oral Maxillofac Surg 30: 455‑457.
- Pritchard JE, McKay JW (1948) Osteoid Osteoma. Can Med Assoc J 58: 567‑575.
- Karandikar S, Thakur G, Tijare M, Shreenivas K, Agrawal K (2011) Osteoid Osteoma of Mandible. BMJ Case Rep 2011: bcr1020114886.
- Chaudhary M, Kulkarni M (2007) Osteoid Osteoma of the Mandible. J Oral Maxillofac Pathol 11: 52‑55.
- Rahsepar B, Nikgoo A, Fatemitabar SA (2009) Osteoid Osteoma of Subcondylar Region: Case Report and Review of the Literature. J Oral Maxillofac Surg 67: 888‑893.
- Regezi JA, Sciubba J. Oral Pathology. 2nd ed. Philadelphia, PA: Saunders; 1993. p. 407.
- Thoma KH, Goldman HM (1960) Oral Pathology. 5th ed St Louis: Mosby Company 231‑241.
- Aghabeigi B, Evans AW, Crean SJ, Hopper C (2003) Simultaneous Repair of an Orbital Floor Fracture and Removal of an Ethmoid Osteoma: Case Report and Re View of the Literature. Int J Oral Maxillofac Surg 32: 94‑96.
- Longo F, Califano L, De Maria G, Ciccarelli R (2001) Solitary Osteoma of the Mandibular Ramus: Report of A Case. J Oral Maxillofac Surg 59: 698‑700.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Kumar A, Chowdhury SKR, Rana RPS (2022) Osteiod Osteoma of Mandibular Condyle: A Rare Case Report. J Dent Pathol Med 6: 125. DOI: 10.4172/jdpm.1000125
Copyright: © 2022 Kumar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2717
- [From(publication date): 0-2022 - Nov 17, 2025]
- Breakdown by view type
- HTML page views: 2221
- PDF downloads: 496